Chronic obstructive pulmonary disease (COPD) is term used to describe a group of progressives lung diseases that make it harder to breathe.
Some people have one of two types of COPD—chronic bronchitis or emphysema. Others have a combination of both.
COPD is often stable for periods and then suddenly flares up.
If you smoke, quitting now can keep COPD from getting worse. With medication, exercise, and other steps, you can live well for decades with COPD.
What is COPD?
COPD stands for chronic obstructive pulmonary disease. COPD is a lung disease that makes it hard to breathe. COPD includes chronic bronchitis and emphysema, two lung conditions that often share a common cause—smoking.
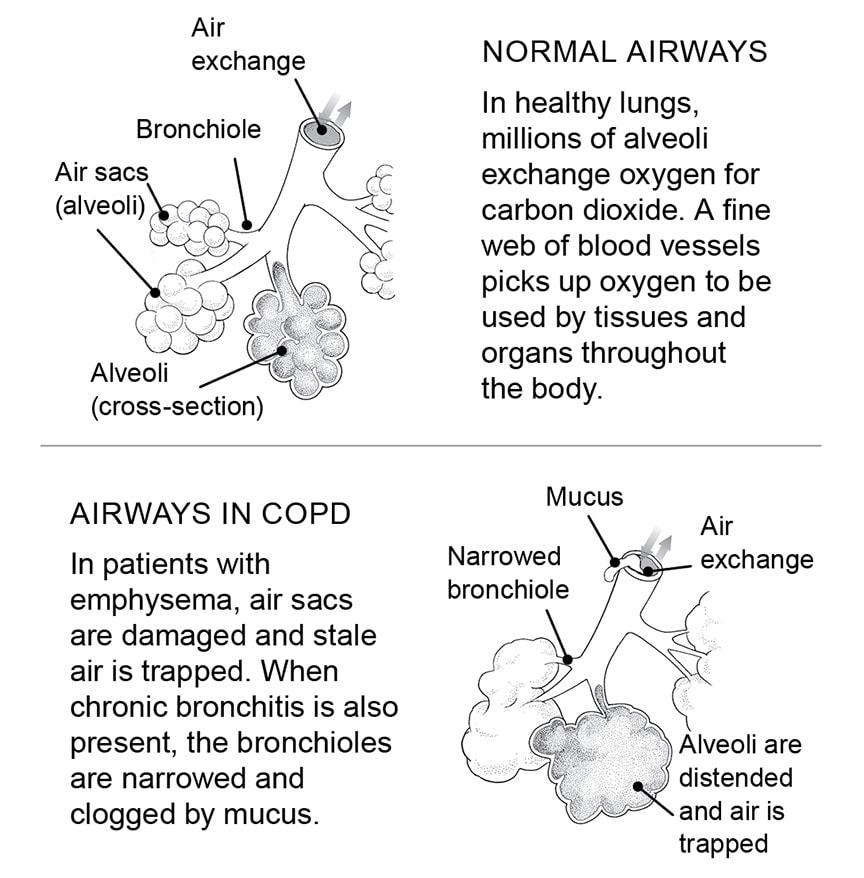
Normally, when you take a breath, air travels from your nose and mouth through your windpipe and into the bronchi. Bronchi are air passages that branch off into each lung. The bronchi branch further into thousands of smaller, thinner tubes called bronchioles. These tubes end in grape-like clusters of small, round air sacs called alveoli.
Tiny blood vessels, called capillaries, absorb oxygen from the air through the walls of the alveoli and deliver it to cells throughout the body. Carbon dioxide moves in the opposite direction. It passes out of the bloodstream, back into the alveoli, and is then eliminated from the body when you breathe out.
How COPD affects the lungs
In COPD, less air flows in and out of the airways, for several reasons:
- The airways and air sacs can’t expand and contract as they should.
- The walls between air sacs break down. This means less surface area for oxygen to pass into the capillaries and the rest of the body.
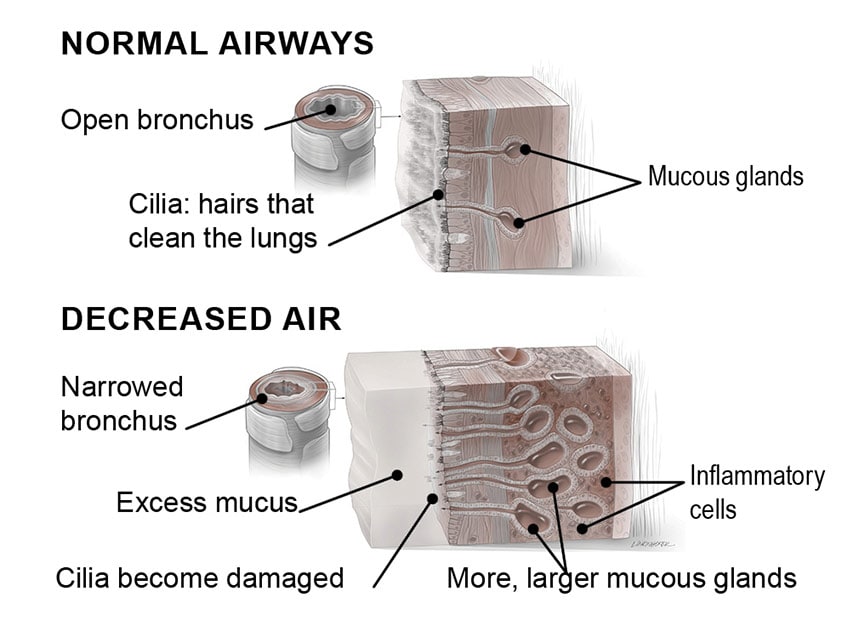
- The walls of the airways become thick and inflamed.
- The airways make more mucus, making it hard for air to flow freely.
Focus On: Chronic bronchitis
Chronic bronchitis develops when the bronchi are irritated day after day. This can trigger overproduction of mucus along with inflammation and swelling of the airways.
Inflammation narrows the airways. Mucus blocks them further. Like traffic crawling on a congested road, air moves slowly in and out of your lungs. You may wheeze as you work hard to breathe, and cough to clear mucus from your airways.
People with chronic bronchitis find it increasingly difficult to exercise and remain active.
Symptoms of chronic bronchitis include:
- ongoing cough with mucus
- wheezing
- shortness of breath
Focus On: Emphysema
Emphysema affects the lung tissue itself. This is different from chronic bronchitis, which affects the passages that carry air to and from the lungs.
Emphysema destroys the walls between the tiny air sacs (alveoli). This leaves the lungs less able to deliver oxygen to the bloodstream and remove carbon dioxide from the bloodstream.
Lung tissue also loses its resilience, which prevents it from stretching and contracting properly. When the lungs lack resilience, they cannot fully push out air. Instead, some air remains trapped in the air sacs.
Symptoms of emphysema include:
- shortness of breath
- weight loss
- loss of muscle
- a barrel chest, from over inflation of the lungs
The main symptom of emphysema is breathlessness. At first, you have difficulty catching your breath during activity. Over time, you may feel breathless after taking a few steps, or when sitting or lying down.
How is COPD diagnosed?
Your story of your health and how you are feeling can alert your doctor to test you for COPD.
Medical history and physical exam
Your doctor will ask whether you smoke. He or she may also ask whether you have breathed in toxic chemicals on the job. The doctor will need to know how easily you become short of breath and when. Do you have trouble climbing stairs? How long can you walk before you have to stop and rest?
Next, the doctor will listen to your lungs through a stethoscope for telltale signs of COPD.
Blood tests
Lab tests can show how much COPD has affected your lungs’ ability to take up oxygen and eliminate carbon dioxide.
- Pulse oximetry. The doctor places a probe on your finger that measures whether the oxygen level in your blood is normal or low.
- Arterial blood gas. This blood test measures how much oxygen and carbon dioxide are in your blood.
Pulmonary function tests
Pulmonary function tests show how well your lungs work. You breathe in and out through a spirometer, a tube that is connected to various machines.
These tests measure two things:
- Forced vital capacity shows the maximum amount of air you can breathe out in one breath.
- Forced expiratory volume in one second is the maximum amount of air you can exhale in one second. If it is low (below 80%), you may benefit from taking COPD medications. If it is very low (less than 50%), ask your doctor if you should see a lung specialist.
Pulmonary function tests are simple and painless.
X-rays
If you have emphysema, your lungs may appear larger than normal on a chest x-ray and hold abnormally large amounts of air.
Your diaphragm (the main muscle involved in breathing) may appear flattened.
If you have chronic bronchitis, a chest x-ray is likely to look normal.
Causes
Smoking is the main cause of COPD. Most people who develop COPD smoke.
Smoking
- In most people with COPD, years of smoking irritate the respiratory tract. The body’s immune system sends out inflammatory cells to attack the irritants. This triggers a cascade of events that damages the airways and lung tissue.
- Breathing in secondhand smoke over a long period of time also increases the risk of developing COPD.
Other causes
- Inherited problems can cause COPD.
- So can long-term exposure to toxic fumes, industrial smoke, and dust.
Taking control of COPD
If you smoke, quitting is the most important thing you can do to stop COPD from getting worse.
Smoking leads to both physical and behavioral addiction. So it is a hard habit to break.
Medications and therapy can help you overcome physical addiction to nicotine.
Quit-smoking medications
Nicotine-replacement medications deliver a low dose of nicotine into your bloodstream to ease or erase withdrawal symptoms. Gradually you wean yourself off tobacco and nicotine replacement.
Nicotine replacement products are available in several forms:
- patches
- gum
- nasal sprays
- inhalers
- lozenges
Two other prescription quit-smoking medications don't contain nicotine. They act on the brain to decrease cravings, withdrawal symptoms, or both.
Behavioral therapy
Therapy, either one-on-one with a counselor or group counseling with people who have quit or are trying to, can help you break long-held habits.
Treating COPD
Medications and other treatments won’t cure COPD. But they can help you breathe better and remain active.
Bronchodilators
Bronchodilators open up the airways. They are the cornerstone of COPD treatment. Once you begin using a bronchodilator, you should have less shortness of breath and more capacity for exercise.
Long-acting bronchodilators are used every day to keep airways open and relaxed. Short-acting bronchodilators are used mainly for quick relief during a flare-up.
Bronchodilators are usually inhaled.
Corticosteroids
Corticosteroids are powerful drugs that curb inflammation and help open airways. They are available in inhalers and as pills.
Inhaled corticosteroids are effective but can increase the risk of pneumonia. They are mainly for people with severe COPD or those who have frequent lung infections.
Corticosteroids in pill form can cause even more serious side effects, but they can effectively control flare-ups.
Antibiotics
Antibiotics are used to treat lung infections caused by bacteria. People with COPD often need antibiotics for respiratory infections. Early treatment is very important.
Oxygen therapy
As COPD becomes more severe, the oxygen level in your blood may become dangerously low. If this happens to you, breathing in extra oxygen can help you live longer. And it can help you avoid problems that can occur when your body isn’t getting enough oxygen on its own.
Some oxygen delivery systems are small and lightweight enough to use while doing regular activities, such as shopping or running errands.
Surgery
Surgery may help if you have emphysema. Lung volume reduction surgery involves removing some damaged lung tissue. This gives healthier lung tissue more room to expand and contract. It also helps the lungs work more effectively.
A lung transplant may be an option for people with severe emphysema who cannot benefit from other types of lung surgery.
Pulmonary rehabilitation
Pulmonary rehabilitation can help individuals with COPD control their symptoms.
Rehabilitation can improve quality of life, helping individuals carry out day-to-day activities with greater ease and independence. Rehabilitation includes:
-
Exercise therapy - Exercise, particularly aerobic exercise, increases your endurance and strengthens your muscles.
-
Breathing retraining - Rehabilitation teaches you to adjust your breathing, so you don’t run out of air when you are active. This should improve your stamina and decrease breathlessness.
-
Education - A nurse may demonstrate how to use an inhaler correctly. Or you may get some tips on how to use oxygen therapy most effectively.
-
Psychological support - Ongoing breathing difficulties can lead to depression and anxiety. Therapy can help you sort through your feelings and teach stress reduction techniques to help you cope.
Get immunized
COPD increases your risk of lung infections.
These infections can make COPD symptoms worse. Such flare-ups are called exacerbations.
If you have COPD, get a flu shot every year. Request the injectable flu shot, which contains killed virus, rather than the nasal spray vaccine, which is made with live, weakened flu virus.
You should also get the pneumococcal vaccine, which protects against the most common type of pneumonia.
Have a COPD action plan
Your doctor should discuss an action plan in case you have an exacerbation. If you have symptoms of increased cough with thick, discolored mucus, particularly if you have shortness of breath, contact your doctor right away. Your doctor will determine if you need an antibiotic and/or oral corticosteroids to manage your symptoms.
Talk with your doctor
Whether this is your first visit or a follow-up, ask your doctor:
- Do I have chronic bronchitis, emphysema, or both?
- Should I be on any additional medications or therapies to help my breathing?
- Am I using my inhaler correctly?
- Should I get the flu shot and pneumococcal vaccine?
- What are the warning signs that my COPD is flaring up?
- What should I do if I get a lung infection?
- Would I benefit from pulmonary rehabilitation?
Tell your doctor if:
- You have had any respiratory infections since your last visit.
- Your activity level has decreased due to trouble breathing.
- You think your medications are causing any side effects.