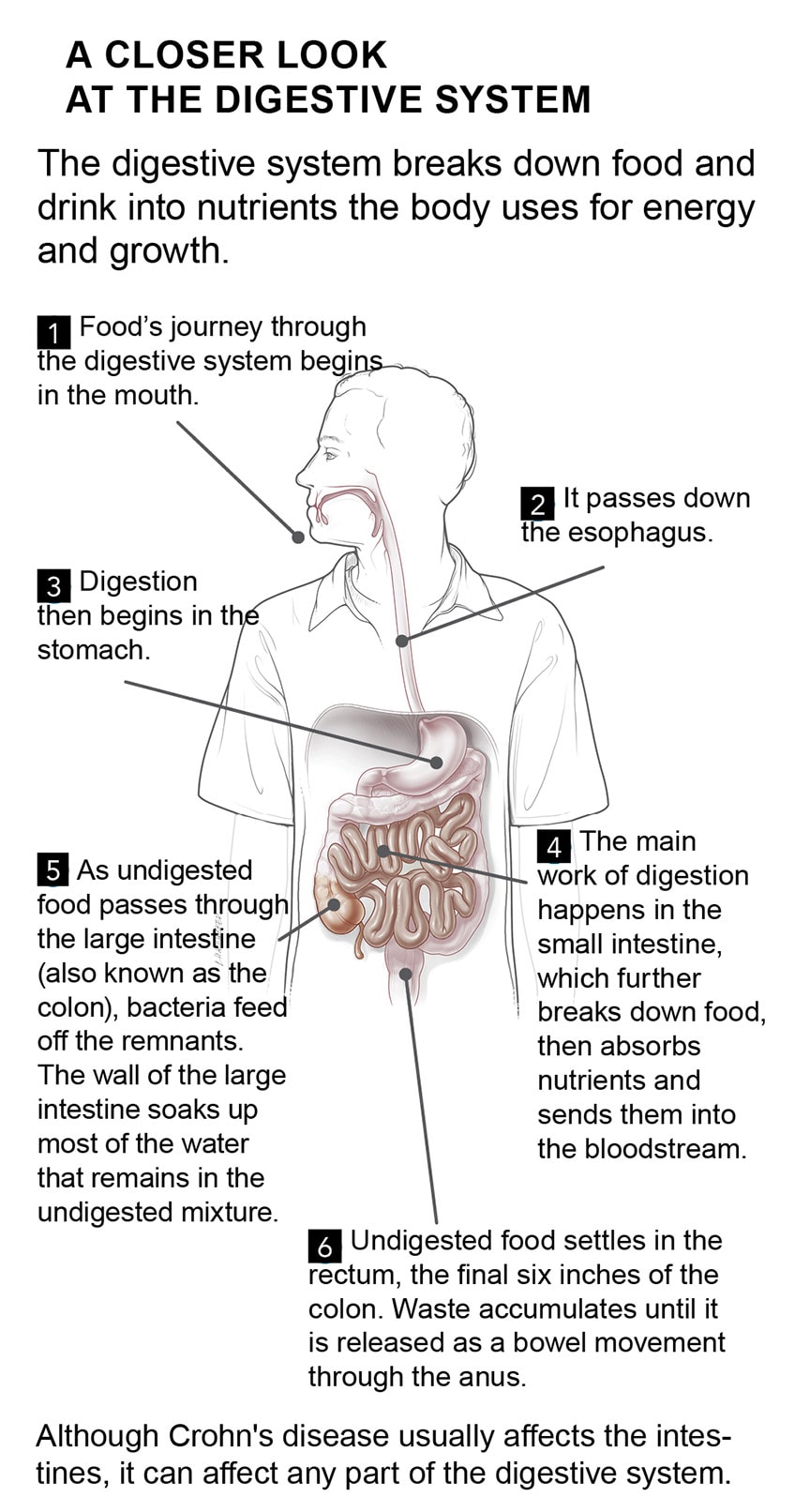
Crohn’s disease is an inflammatory bowel disease. It causes damage in the digestive tract, most often in the small and large intestines. People with Crohn’s disease experience diarrhea, abdominal pain, weight loss, and fatigue.
Crohn’s disease may cause only occasional symptoms. Or the symptoms may be constant. Medications can usually control the inflammation. But sometimes surgery is required.
What is Crohn’s disease?
In Crohn’s disease, inflammation injures the intestines.
No one knows for sure why some people develop Crohn’s disease. Normally, our immune system identifies and attacks infections and other health threats. But in people with Crohn’s disease, the immune system misfires and attacks the lining of the digestive tract, creating inflammation and damage.
The inflammation most often injures the final section of the small intestine, called the ileum, and the beginning of the large intestine. However, the disease can affect any part of the digestive tract, including the mouth.
The inside lining and deeper layers of the intestinal wall become swollen and irritated. The lining thickens or wears away in spots. This creates open sores (ulcers), cracks, small tears (fissures), and pockets of pus. Fistulas often form as well. These are abnormal, tunnel-like connections between the intestine and skin, or between organs in the digestive tract.
People with Crohn’s disease may also develop inflammation in other areas, such as the eyes and joints.
Symptoms of Crohn’s disease
Crohn’s disease causes lifelong symptoms.
Some people with Crohn’s disease experience flares, or periods when symptoms suddenly get worse, followed by periods of remission, when they have no symptoms. Other people have constant symptoms.
The most common symptoms include:
- abdominal pain, usually at or below the navel, that is typically worse after meals
- diarrhea that may contain blood
- weight loss
- weakness or fatigue
Other symptoms can include:
- sores around the anus
- drainage of pus or mucus from the anus
- pain when you have a bowel movement
- painful mouth sores
- loss of appetite
- joint pain or soreness
- back pain
- eye inflammation, which can cause pain or vision changes in one or both eyes
- fever
- red, tender bumps under the skin
Complications of Crohn’s disease
Crohn’s disease can cause serious problems.
Bowel obstruction
Thickening of the intestinal wall can partially or completely block the passage of food or stool. Bowel obstruction causes vomiting or severe abdominal pain.
Complete bowel obstruction is life-threatening.
Bowel obstruction often requires a hospital stay and possibly surgery to open the blockage.
Malnutrition
Damaged intestines cannot digest and absorb enough nutrients to stay healthy.
Eat a well-balanced, nutritious diet when possible.
Some people need to get fluids through a vein (IV) or fluids and nutrients through a feeding tube connected to the stomach.
Fistulas
Fistulas are abnormal passageways between the intestine and skin, or between organs in the digestive tract. Fistulas can heal with medication and changes in diet. Some people need surgery to repair fistulas.
Ulcers
These open sores can develop anywhere in the gastrointestinal tract. Treatment for Crohn’s usually heals ulcers.
Inflammation throughout the body
Crohn’s disease can cause inflammation in the joints, eyes, and skin. Inflammation is treated with medications.
Anal fissures
Small tears in the anus may cause itching, pain, or bleeding. Warm baths and medical treatment can speed healing.
How is Crohn’s disease diagnosed?
There is no single test for Crohn's disease.
Diagnosing Crohn’s disease may take time, sometimes many months.
The symptoms can be very similar to an infection or irritable bowel syndrome. Your doctor may need to do several tests to rule out other conditions that cause similar symptoms.
Some tests are often, but not always, abnormal in people with Crohn's disease.
Blood tests
These tests can show a high white blood cell count, signs of inflammation, or anemia, a reduced number of red blood cells.
Autoantibody tests
These may support a Crohn's disease diagnosis rather than another type of inflammatory bowel disease.
Stool tests
These can detect the presence of white blood cells produced by inflamed intestines and can make sure there is no infection causing the symptoms. They are also called feces or bowel movement tests.
Imaging tests
Imaging tests let doctors get a close look at the gastrointestinal tract.
You may need one or more of the following tests to see whether your symptoms are caused by Crohn's disease or some other condition.
- CT scan of the abdomen. In this test, a CT scanner takes pictures of your abdomen after you drink a barium solution that shows up on the scan. This test can reveal areas of abnormally thick or narrowed intestine. It also can highlight ulcers and fistulas.
- Colonoscopy. In this test, a small tube with an attached camera and light is inserted into your rectum and large intestine. It allows the doctor to view the inside of your large intestine and the end of your small intestine (the ileum).
- MR enterography. This test uses a special dye and magnetic resonance imaging (MRI) to take pictures of the intestines.
- Wireless capsule endoscopy. You swallow a pill-sized video camera. It sends pictures of your small intestine wirelessly.
Biopsy
A biopsy is most helpful to confirm Crohn’s disease and rule out other conditions. In a biopsy, the doctor removes a small sample of tissue from the lining of the intestine for examination in a laboratory.
Treatment Overview
Helping yourself feel better
Lifestyle changes can help improve symptoms.
Modify your diet
It may help to eat smaller meals throughout the day rather than three large meals.
To identify foods that worsen your symptoms, record what you eat over several weeks, and how you feel afterwards. You may notice a pattern. For example, you may notice more symptoms from carbonated beverages; high-fiber foods like popcorn, vegetable skins, and nuts; and gas-causing foods, like beans and broccoli.
You may need to take a protein and calorie supplement or a daily multivitamin supplement.
Avoid NSAID drugs
Do not take nonsteroidal anti- inflammatory drugs (NSAIDs), like aspirin, ibuprofen, and naproxen, for pain or discomfort. They can worsen Crohn’s disease.
Stop smoking
Don’t smoke. Smoking can make Crohn’s disease flare up and increase the risk of needing surgery. Ask your doctor if you need help to quit.
Medications to treat Crohn’s disease
Medications cannot cure Crohn’s disease. But they can help stop or ease symptoms. Most drugs for Crohn’s disease work by reducing inflammation in the intestines.
- Aminosalicylates are anti-inflammatory drugs that suppress inflammation in the intestine and joints.
- Corticosteroids quiet down the immune system and decrease inflammation.
- Immunomodulators dampen immune system activity. This reduces inflammation in the digestive tract and also helps stop symptoms.
- Biologic therapies target a protein made by the immune system. They decrease inflammation in the intestine and can also stop symptoms.
Your doctor may also prescribe:
- acetaminophen for mild pain
- antibiotics, to prevent or treat infections and fistulas
- medication to slow or stop severe diarrhea
Bowel rest
When symptoms of Crohn’s disease become severe, you may need to rest your bowels for several days to several weeks. Bowel rest gives your intestines a chance to heal. During bowel rest, your doctor will likely advise a liquid diet containing easily absorbed nutrients. Sometimes bowel rest means not taking anything by mouth. In that case, you will get nutrition through a vein.
Surgical treatments for Crohn’s
Surgery can relieve obstruction and remove areas of inflammation that do not respond to medication.
It can improve symptoms and help you return to normal activities.
Surgery may be an option if you have:
- a fistula
- a bowel obstruction
- symptoms in one area of the bowel that cannot be controlled with medications
The type of surgery you have will depend on your symptoms and where in your digestive tract they are located. Variations on the following procedures are usually done in people with Crohn's disease.
Small bowel resection
This is a procedure to remove part of the small intestine:
- There is a blockage or severe disease in the small intestine
- The surgeon removes the diseased or blocked section
- The surgeon reconnects the healthy ends of the small intestine
Large bowel resection
This surgery removes part of the large intestine:
- There is a blockage, a fistula, or severe disease in the colon
- The surgeon removes the diseased or blocked section
- The surgeon reconnects the healthy ends of the large intestine
Dietary supplements
Dietary supplements may offset some effects of Crohn’s disease.
Vitamins and minerals
Crohn’s disease increases your risk for vitamin and mineral deficiencies because it affects the small intestine, where vitamins and minerals are absorbed. Deficiencies can also be a side effect of medication or surgery. Your doctor may recommend supplements such as:
- Vitamin B12: Low levels can cause anemia, in which the body makes too few red blood cells.
- Vitamin D and calcium: Both are essential for bone health.
- Iron: Iron deficiency can cause anemia.
Probiotics
Probiotics are live bacteria. They help restore the balance of “good” bacteria in the intestines. Probiotics may help improve symptoms of Crohn’s disease. They are found in many cultured and fermented foods, such as yogurt, miso, sauerkraut, and soy beverages. They can also be taken as dietary supplements. Talk with your doctor before starting a probiotic.
What else could it be?
Other conditions can cause symptoms similar to those of Crohn's disease.
Irritable bowel syndrome (IBS)
Often, people with Crohn’s disease are first diagnosed with IBS. The main symptoms of IBS are cramping, abdominal pain, bloating, and altered bowel habits. People with IBS can experience either diarrhea or constipation, or alternate between the two.
Diverticulitis
Diverticula are small, finger-like pouches that extend off the inner lining of the colon. Diverticulitis occurs when a diverticulum becomes inflamed or infected. Abdominal pain is often accompanied by chills, fever, and an elevated white blood cell count.
Ulcerative colitis
Ulcerative colitis is an inflammatory bowel disease. It causes inflammation of the lining of the colon. It can cause lower abdominal pain, diarrhea, fever, weight loss, and an elevated white blood cell count.
Celiac disease
When people with celiac disease eat foods that have gluten, their immune system attacks and damages the small intestine. This can cause abdominal pain, bloating, diarrhea, vomiting, weight loss, and fatigue.
Crohn’s disease and colorectal cancer
Crohn’s disease increases your risk of colorectal cancer.
Colorectal tumors often begin as polyps. These are small growths on the inside of the large intestine.
The risk of colorectal cancer increases based on:
- how much of your colon is affected by Crohn’s disease
- how long you have had Crohn’s disease affecting your colon
- whether you have had persistent fistulas
People with Crohn’s disease should have more frequent tests for colorectal cancer than people who are not at increased risk. The best screening test for colorectal cancer is a colonoscopy.
Biopsies can be taken during a colonoscopy to check for precancerous changes. Polyps can also be removed during the procedure, reducing the chance that they will become cancerous. Ask your doctor how often you should be checked for colorectal cancer.
If you’re experiencing diarrhea, abdominal pain, weight loss, and fatigue, it may be time to check with your doctor about Crohn’s disease. The symptoms may be constant or intermittent. For most, medications can control the inflammation, but for others, surgery is the answer. Work closely with your doctor to determine the best course of action for you.
Talk with your doctor
Whether this is your first visit or a follow-up, ask your doctor:
- What symptoms should I be on the lookout for?
- What medications, if any, should I take when I am symptom-free?
- What medications should I take when my symptoms get worse?
- Will I need to have surgery?
- Would eliminating certain foods from my diet help relieve my symptoms?
- Should I take any dietary supplements?
- When and how often should I get checked for colorectal cancer?
Tell your doctor if:
- You have had any new symptoms
- Your symptoms have improved or worsened since your last visit
- You think your medications are causing any side effects