Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Excedrin Tension Headache: Acetaminophen 500 mg and caffeine 65 mg [contains benzoic acid, brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #6 (sunset yellow)]
Excedrin Tension Headache: Acetaminophen 500 mg and caffeine 65 mg [DSC] [contains benzoic acid, fd&c blue #1 aluminum lake, fd&c red #40, fd&c yellow #10 aluminum lake]
Excedrin Tension Headache: Acetaminophen 500 mg and caffeine 65 mg [aspirin free; contains benzoic acid, fd&c blue #1 aluminum lake, fd&c red #40]
Excedrin Tension Headache: Acetaminophen 500 mg and caffeine 65 mg [DSC] [aspirin free; contains fd&c blue #2 aluminum lake, fd&c yellow #6 aluminum lake]
Pharmacology
Mechanism of Action
Acetaminophen: Although not fully elucidated, the analgesic effects are believed to be due to activation of descending serotonergic inhibitory pathways in the CNS. Interactions with other nociceptive systems may be involved as well (Smith 2009). Antipyresis is produced from inhibition of the hypothalamic heat-regulating center.
Caffeine: Blocks adenosine receptors (mainly A1 and A2A subtypes), induces calcium mobilization from the sarcoplasmic reticulum and inhibits calcium reuptake, increases levels of cyclic AMP by inhibiting phosphodiesterase (Cappelletti 2015).
Use: Labeled Indications
Pain: For the temporary relief of pain caused by headache or muscle aches
Contraindications
OTC labeling: When used for self-medication, do not use with other drugs containing acetaminophen or if you are allergic to acetaminophen, aspirin, or any other pain reliever.
Dosage and Administration
Dosing: Adult
Pain: Oral: Acetaminophen 1 g/caffeine 130 mg every 6 hours as needed (maximum: acetaminophen 3 g/caffeine 390 mg per 24 hours)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Pain: Children ≥12 years and Adolescents: Refer to adult dosing.
Dietary Considerations
Limit the use of caffeine-containing beverages or foods.
Storage
Store at 20°C to 25°C (68°F to 77°F).
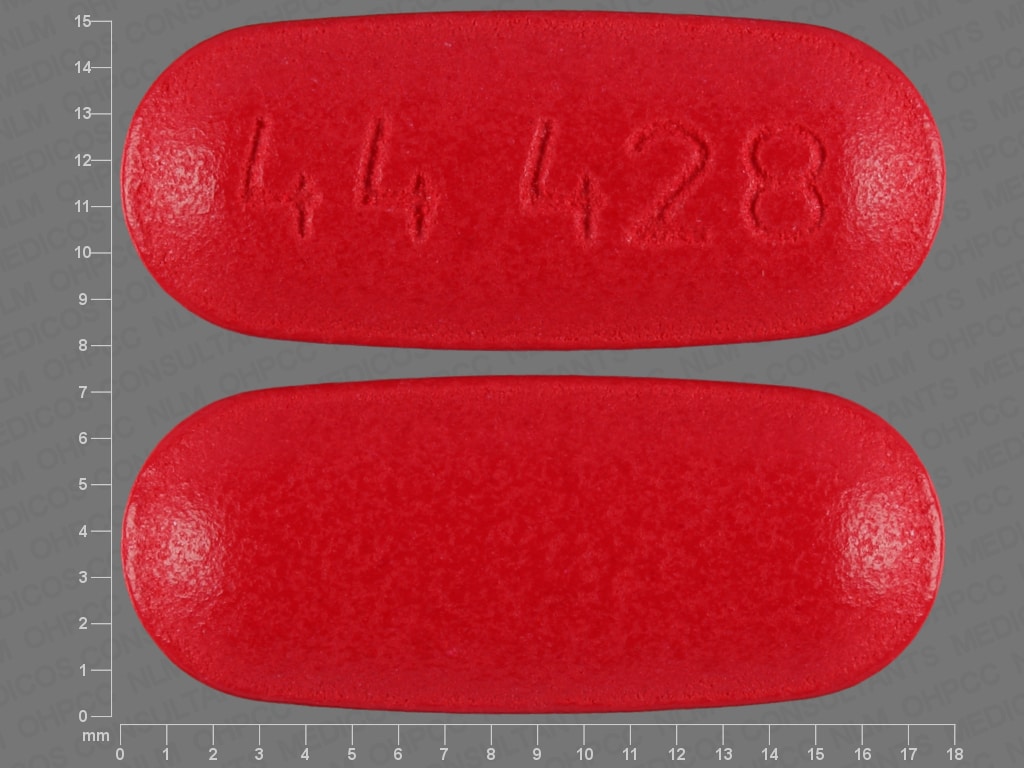
Acetaminophen and Caffeine Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Adenosine: Caffeine and Caffeine Containing Products may diminish the therapeutic effect of Adenosine. Management: Monitor for decreased effect of adenosine if patient is receiving caffeine. Discontinue caffeine in advance of scheduled diagnostic use of adenosine whenever possible. Consider therapy modification
Alcohol (Ethyl): May enhance the hepatotoxic effect of Acetaminophen. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Barbiturates: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Exceptions: Amobarbital; Butabarbital; Butalbital; Methohexital; PENTobarbital; Secobarbital; Thiopental. Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
Bromperidol: Caffeine and Caffeine Containing Products may decrease the absorption of Bromperidol. Monitor therapy
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Busulfan: Acetaminophen may increase the serum concentration of Busulfan. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
CarBAMazepine: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Dasatinib: Acetaminophen may enhance the hepatotoxic effect of Dasatinib. Dasatinib may increase the serum concentration of Acetaminophen. Consider therapy modification
Doxofylline: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Doxofylline. Avoid combination
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Flucloxacillin: May enhance the adverse/toxic effect of Acetaminophen. Specifically, the risk for high anion gap metabolic acidosis may be increased. Monitor therapy
Formoterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Formoterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Formoterol. Monitor therapy
Fosphenytoin-Phenytoin: May decrease the serum concentration of Acetaminophen. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of the toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Imatinib: Acetaminophen may enhance the hepatotoxic effect of Imatinib. Monitor therapy
Indacaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Indacaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Indacaterol. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Isoniazid: May enhance the adverse/toxic effect of Acetaminophen. Monitor therapy
LamoTRIgine: Acetaminophen may decrease the serum concentration of LamoTRIgine. Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lithium: Caffeine and Caffeine Containing Products may decrease the serum concentration of Lithium. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
MetyraPONE: May increase the serum concentration of Acetaminophen. More importantly, by inhibiting the conjugative metabolism of acetaminophen, metyrapone may shift the metabolism towards the oxidative route that produces a hepatotoxic metabolite. Monitor therapy
Mipomersen: Acetaminophen may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Norfloxacin: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Olodaterol: Caffeine and Caffeine Containing Products may enhance the adverse/toxic effect of Olodaterol. Caffeine and Caffeine Containing Products may enhance the hypokalemic effect of Olodaterol. Monitor therapy
Phenylephrine (Systemic): Acetaminophen may increase the serum concentration of Phenylephrine (Systemic). Monitor therapy
Pipemidic Acid: May increase the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probenecid: May increase the serum concentration of Acetaminophen. Probenecid may also limit the formation of at least one major non-toxic metabolite, possibly increasing the potential for formation of the toxic NAPQI metabolite. Consider therapy modification
Regadenoson: Caffeine and Caffeine Containing Products may diminish the vasodilatory effect of Regadenoson. Management: Avoiding using caffeine or other methylxanthine containing products (e.g., theophylline) for at least 12 hours prior to the administration of regadenoson. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
SORAfenib: Acetaminophen may enhance the hepatotoxic effect of SORAfenib. SORAfenib may increase the serum concentration of Acetaminophen. Consider therapy modification
Stiripentol: May increase the serum concentration of Caffeine and Caffeine Containing Products. Avoid combination
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tobacco (Smoked): May decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Acetaminophen may enhance the anticoagulant effect of Vitamin K Antagonists. This appears most likely with daily acetaminophen doses exceeding 1.3 or 2 g/day for multiple consecutive days. Monitor therapy
Test Interactions
See individual agents.
Adverse Reactions
See individual agents.
Warnings/Precautions
Concerns related to adverse effects:
- Hepatotoxicity: Acetaminophen has been associated with severe liver damage. Hepatotoxicity is usually associated with excessive intake and often involves more than one product that contains acetaminophen. Do not exceed more than 6 tablets in 24 hours and do not combine with other products that contain acetaminophen.
- Skin reactions: Serious and potentially fatal skin reactions, including acute generalized exanthematous pustulosis (AGEP), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) have occurred rarely with acetaminophen use. Discontinue therapy at the first appearance of skin rash (FDA 2013).
Disease-related concerns:
- Ethanol use: Use with caution with concomitant alcohol use; consuming ≥3 alcoholic drinks/day may increase the risk of liver damage.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Caffeine: Contains an amount of caffeine similar to one cup of coffee; limit the use of caffeine-containing beverages or foods during therapy.
- Dosage limit: Limit acetaminophen dose from all sources (prescription, OTC, combination products) and all routes of administration (IV, oral, rectal) to <4 g/day (adults).
- Self-medication (OTC use): When used for self-medication, patients should be instructed to contact health care provider if symptoms get worse or new symptoms appear, redness or swelling is present in the painful area, fever lasts >3 days, or pain lasts longer than 10 days.
Pregnancy
Pregnancy Considerations
See individual agents.
Patient Education
What is this drug used for?
- It is used to ease pain.
Frequently reported side effects of this drug
- Anxiety
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Fast heartbeat
- Unable to pass urine
- Change in amount of urine passed
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.