Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Provigil: 100 mg
Provigil: 200 mg [scored]
Generic: 100 mg, 200 mg
Pharmacology
Mechanism of Action
The exact mechanism of action is unclear. Modafinil has been shown to significantly increase dopamine in the brain by blocking dopamine transporters; however, has a lower affinity for dopamine receptors compared to amphetamines (Volkow 2009). EEG studies have shown modafinil increases high-frequency alpha waves while decreasing both delta and theta wave activity, effects consistent with generalized increases in mental alertness (James 2011). Studies also have demonstrated decreased GABA-mediated neurotransmission through increased turnover of serotonin and enhanced activity of 5-HT2 receptors and that an intact central alpha-adrenergic system is required for modafinil's activity (Kumar 2008; Schwartz 2008).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 0.9 L/kg
Metabolism
Hepatic; multiple pathways including CYP3A4
Excretion
Urine (80% as metabolites, <10% as unchanged drug); feces (1%)
Time to Peak
Serum: 2 to 4 hours; may be delayed ~1 hour with food.
Half-Life Elimination
Effective half-life: 15 hours
Protein Binding
~60%, primarily to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
In severe, chronic renal failure (CrCl ≤20 mL/minute), exposure to modafinil acid (inactive metabolite) was increased 9-fold.
Special Populations: Hepatic Function Impairment
In patients with cirrhosis of the liver, clearance is decreased ~60% and steady-state concentrations are doubled.
Special Populations: Elderly
Oral clearance decreased approximately 20% in patients with a mean age of 63 years of age.
Use: Labeled Indications
Narcolepsy: To improve wakefulness in adult patients with excessive sleepiness associated with narcolepsy.
Obstructive sleep apnea: To improve wakefulness in adult patients with obstructive sleep apnea (OSA)
Shift work sleep disorder: To improve wakefulness in adult patients with shift work sleep disorder (SWSD)
Use: Off Label
Fatigue (cancer-related)byes
Data from a large randomized phase III study support the use of modafinil for the management of severe cancer-related fatigue in adults receiving active cancer treatment Jean-Pierre 2010.
Based on the American Society of Clinical Oncology (ASCO) guidelines for screening, assessment, and management of fatigue in adult survivors of cancer, modafinil may be used to manage fatigue in adult patients with advanced disease or in patients receiving active cancer treatment.
Major depressive disorder (antidepressant augmentation)cyes
Data from a meta-analysis (including 4 double-blind, randomized, placebo-controlled trials in patients with major depressive disorder) suggest that modafinil augmentation of antidepressants may be beneficial for the treatment major depressive disorder characterized by excessive fatigue and sleepiness Abolfazli 2011, DeBattista 2003, Dunlop 2007, Fava 2005, Goss 2013. Additional data may be necessary to further define the role of modafinil in this condition.
Based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the treatment of major depressive disorder, modafinil given as an adjunct to antidepressant therapy is suggested as a third-line option for patients with a non-response or incomplete antidepressant response for the treatment of residual symptoms of fatigue and sleepiness in depression CANMAT [Kennedy 2009].
Multiple sclerosis-related fatiguebyes
Use of modafinil in the treatment of MS-related fatigue has been evaluated in controlled and noncontrolled settings demonstrating conflicting results. Most placebo-controlled trials and meta-analyses indicate no benefit, although some studies suggest that lower dosages (200 mg daily) are more effective than higher dosages (400 mg daily). American Academy of Sleep Medicine guidelines and German Multiple Sclerosis Society guidelines state that modafinil may be effective in patients who do not respond to initial therapy. However, these recommendations are based on conflicting data of moderate quality and conflicting expert opinion.
Contraindications
Known hypersensitivity to modafinil, armodafinil, or any component of the formulation.
Canadian labeling: Additional contraindications (not in the US labeling): Patients in agitated states or with severe anxiety; pregnancy; females who may become pregnant.
Dosage and Administration
Dosing: Adult
Narcolepsy, obstructive sleep apnea (OSA): Oral: Initial: 200 mg as a single daily dose in the morning. Note: Doses up to 400 mg once daily have been well tolerated, but there is no consistent evidence that this dose confers additional benefit.
Shift work sleep disorder (SWSD): Oral: Initial: 200 mg as a single dose ~1 hour prior to start of work shift
Off-label uses:
Fatigue, cancer-related, severe (in patients receiving active treatment) (off-label use): Oral: 100 mg once daily for 3 days (beginning on day 5 of second chemotherapy cycle), followed by 200 mg once daily during active treatment (Jean-Pierre 2010).
Major depressive disorder (antidepressant augmentation) (off-label use): Oral: Initial: 100 mg/day for 3 to 7 days, then increase to 200 mg daily; further adjust dose based on response and tolerability up to 400 mg/day (Abolfazli 2011; DeBattista 2003; Dunlop 2007; Fava 2005). Additional data may be necessary to further define the role of modafinil in this condition.
Multiple sclerosis-related fatigue (off-label use): Oral: 100 mg once daily initially, increased as tolerated to 200 mg once daily or if patient experiences post-noon fatigue, 100 mg twice daily (ie, morning and noon). Higher daily doses (greater than 200 mg) do not appear to be effective (Brown 2010; Moller 2011; Rammohan 2002; Stankoff 2005; Zifko 2002).
Dosing: Geriatric
Consider initiating at lower doses.
Dosing: Pediatric
Attention deficit hyperactivity disorder (ADHD); refractory: Limited data available: Note: Due to reports of serious dermatologic adverse effects and psychiatric events in children, modafinil should only be used if first- and second-line treatments have failed and the benefits outweigh the risks.
Children ≥6 years and Adolescents ≤13 years:
Patient weight <30 kg: Oral: 200 to 340 mg once daily (Biederman 2006)
Patient weight >30 kg: Oral: 300 to 425 mg once daily (Biederman 2006)
Administration
For the treatment of narcolepsy and obstructive sleep apnea/hypopnea syndrome, administer dose in the morning. For the treatment of shift work sleep disorder, administer dose ~1 hour prior to start of work shift.
Storage
Store at 20°C to 25°C (68°F to 77°F).
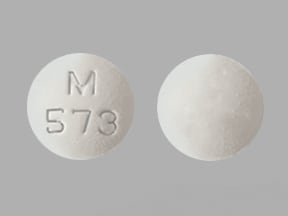
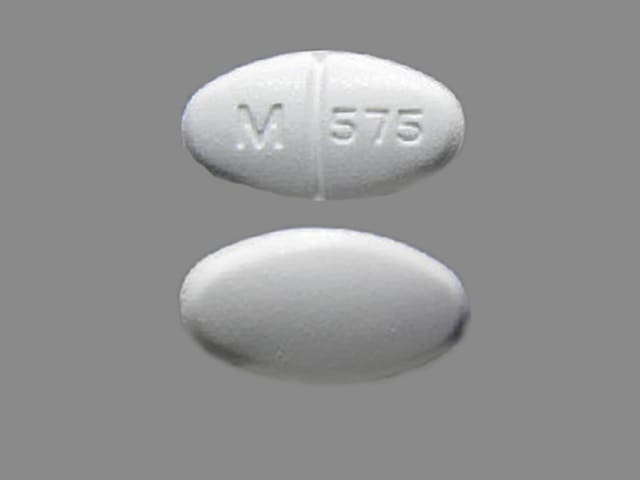
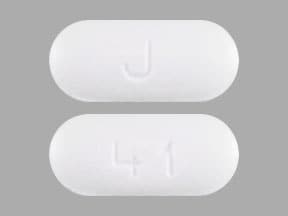
Modafinil Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Abemaciclib. Avoid combination
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Alcohol (Ethyl): May diminish the therapeutic effect of Modafinil. Avoid combination
Antihepaciviral Combination Products: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Asunaprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Asunaprevir. Avoid combination
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Avapritinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Axitinib. Avoid combination
Bedaquiline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bedaquiline. Avoid combination
Benzhydrocodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bosutinib. Avoid combination
Brigatinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inducers when possible. If combined, increase the daily dose of brigatinib in 30 mg increments after 7 days of treatment with the current brigatinib dose, up to maximum of twice the dose. Consider therapy modification
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Clarithromycin: CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Clarithromycin. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and impair its efficacy. Consider therapy modification
CloZAPine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Cobimetinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
CycloSPORINE (Systemic): Modafinil may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Moderate) may decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Exceptions: Apixaban; Rivaroxaban. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Daclatasvir. Management: Increase the daclatasvir dose to 90 mg once daily if used with a moderate CYP3A4 inducer. Consider therapy modification
Dasabuvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Dasabuvir. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Doravirine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Doravirine. Monitor therapy
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Elbasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Monitor therapy
Encorafenib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Encorafenib. Avoid combination
Entrectinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Entrectinib. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Erdafitinib. Management: Dose modifications of erdafitinib may be required. See full monograph for details. Consider therapy modification
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Estriol (Systemic): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Modafinil may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use alternative or concomitant methods of contraception in patients taking modafinil and for one month after modafinil discontinuation. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inducers (Moderate) may decrease the serum concentration of FentaNYL. Monitor therapy
Flibanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Flibanserin. Avoid combination
Glecaprevir and Pibrentasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
Grazoprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Grazoprevir. Avoid combination
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
GuanFACINE: CYP3A4 Inducers (Moderate) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a moderate CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating a moderate CYP3A4 inducer in a patient already taking guanfacine. Consider therapy modification
HYDROcodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ibrutinib. Monitor therapy
Ifosfamide: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Iobenguane Radiopharmaceutical Products: CNS Stimulants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Istradefylline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Istradefylline. Monitor therapy
Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ivacaftor. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lefamulin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: Modafinil may decrease the serum concentration of Letermovir. Avoid combination
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lorlatinib: CYP3A4 Inducers (Moderate) may enhance the hepatotoxic effect of Lorlatinib. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with moderate CYP3A4 inducers. If such a combination must be used, monitor AST, ALT, and bilirubin within 48 hours of starting the combination and at least three times within the first week of combined use. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumateperone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lurasidone. Management: Monitor for decreased lurasidone effects if combined with moderate CYP3A4 inducers and consider increasing the lurasidone dose if coadministered with a moderate CYP3A4 inducer for 7 or more days. Consider therapy modification
Macimorelin: Modafinil may diminish the diagnostic effect of Macimorelin. Monitor therapy
Meperidine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Meperidine. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Mirodenafil. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Naldemedine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Naldemedine. Monitor therapy
Neratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Neratinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of NiMODipine. Monitor therapy
Nisoldipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Olaparib. Avoid combination
Palbociclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Palbociclib. Management: The US label does not provide specific recommendations concerning use with moderate CYP3A4 inducers, but the Canadian label recommends avoiding use of moderate CYP3A4 inducers. Consider therapy modification
Perampanel: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pexidartinib. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pimavanserin. Avoid combination
Pitolisant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pitolisant. Monitor therapy
Pretomanid: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pretomanid. Avoid combination
Ranolazine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ranolazine. Avoid combination
Rolapitant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Rolapitant. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Simeprevir. Avoid combination
Sofosbuvir: Modafinil may decrease the serum concentration of Sofosbuvir. Avoid combination
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sonidegib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Sonidegib. Avoid combination
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tazemetostat: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tazemetostat. Avoid combination
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tezacaftor and Ivacaftor. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ubrogepant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a moderate CYP3A4 inducer. Consider therapy modification
Upadacitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Upadacitinib. Monitor therapy
Velpatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Venetoclax: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Venetoclax. Avoid combination
Voxelotor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and moderate CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zolpidem. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Headache (adults: 34%; children: 20% [Biederman 2005])
Gastrointestinal: Decreased appetite (children: 16% [Biederman 2005]), abdominal pain (children: 12% [Greenhill 2006]), nausea (11%)
1% to 10%:
Cardiovascular: Chest pain (3%), hypertension (3%), palpitations (2%), tachycardia (2%), vasodilation (2%), edema (1%)
Central nervous system: Nervousness (7%), anxiety (5%), dizziness (5%), insomnia (5%), depression (2%), drowsiness (2%), paresthesia (2%), agitation (1%), chills (1%), confusion (1%), emotional lability (1%), hypertonia (1%), vertigo (1%)
Dermatologic: Diaphoresis (1%)
Endocrine & metabolic: Weight loss (children 5% [Greenhill 2006]), increased thirst (1%)
Gastrointestinal: Diarrhea (6%), dyspepsia (5%), xerostomia (4%), anorexia (4%), constipation (2%), dysgeusia (1%), flatulence (1%), oral mucosa ulcer (1%)
Genitourinary: Urine abnormality (1%)
Hematologic & oncologic: Eosinophilia (1%)
Hepatic: Hepatic insufficiency (2%)
Neuromuscular & skeletal: Back pain (6%), dyskinesia (1%), hyperkinesia (1%), tremor (1%)
Ophthalmic: Visual disturbance (1%)
Respiratory: Rhinitis (7%), pharyngitis (4%), asthma (1%), epistaxis (1%)
Frequency not defined:
Endocrine & metabolic: Increased gamma-glutamyl transferase
Hepatic: Increased serum alkaline phosphatase
<1%, postmarketing, and/or case reports: Aggressive behavior, agranulocytosis, anaphylaxis, angioedema, asystole, cerebrovascular accident, delusions, DRESS syndrome, erythema multiforme (pediatric patients), hallucination, hypersensitivity reaction, mania, multiorgan hypersensitivity, psychomotor agitation, psychosis, skin rash, Stevens-Johnson syndrome, suicidal ideation, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May impair the ability to engage in potentially hazardous activities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Dermatologic effects (severe): Serious and life-threatening rashes, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug rash with eosinophilia and systemic symptoms (DRESS) have been reported. Although initially reported in children during clinical trials, postmarketing cases have occurred in both children and adults. Most cases have occurred within the first 5 weeks of therapy; however, rare cases have occurred after long-term use (eg, 3 months). No risk factors have been identified to predict occurrence or severity. Patients should be advised to discontinue at first sign of rash (unless the rash is clearly not drug-related). As a result of these serious dermatologic adverse events, approval for the use of modafinil in children for ADHD was denied by the FDA.
- Hypersensitivity reactions: Rare cases of multiorgan hypersensitivity reactions (with fatality) in association with modafinil use; lone cases of angioedema and anaphylactoid reactions with armodafinil have been reported (angioedema has been noted in postmarketing reports with modafinil). Signs and symptoms are diverse, reflecting the involvement of specific organs; patients typically present with fever and rash associated with organ-system dysfunction. No risk factors have been identified to predict occurrence or severity of multiorgan hypersensitivity reactions. Patients should be advised to report any signs and symptoms related to these effects; discontinuation of therapy is recommended.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiovascular disease; increased blood pressure and heart rate monitoring may be required. Use is not recommended in patients with a history of left ventricular hypertrophy or patients with mitral valve prolapse who have developed mitral valve prolapse syndrome with previous CNS stimulant use. Increased monitoring should be considered in patients with a recent history of myocardial infarction or unstable angina.
- Hepatic impairment: Use with caution in patients with hepatic impairment. Dosage reduction is recommended in patients with severe hepatic impairment.
- Psychiatric disorders: Use with caution in patients with a history of psychosis, depression, or mania. Use may result in emergence of or exacerbation of psychiatric symptoms. Observe for symptoms of aggression, hallucinations, mania, delusions, or suicidal ideation. Consider discontinuing therapy if psychiatric symptoms develop.
- Renal impairment: Use with caution in patients with renal impairment.
- Seizure disorder: Limited information exists regarding the use of modafinil or other stimulants in patients with concomitant ADHD and seizure disorder. Whereas patients with ADHD are at an increased risk for seizure activity compared to the general population, a retrospective study using drug claims data showed that the use of stimulant medications was associated with a lower risk (Cortese 2013; Wiggs 2018). Manufacturers of some stimulants recommend discontinuing therapy if seizures occur.
- Sleep disorders: Appropriate use: The degree of sleepiness should be reassessed frequently; some patients may not return to a normal level of wakefulness. In obstructive sleep apnea, modafinil is indicated as treatment for excessive sleepiness and not for the underlying obstruction. If continuous positive airway pressure (CPAP) is the treatment of choice for a patient, a maximal effort to treat with CPAP for an adequate period of time should be made prior to initiating and during treatment with modafinil for excessive sleepiness.
- Tourette syndrome/tics: Use with caution in patients with Tourette syndrome or other tic disorders. Stimulants may exacerbate tics (motor and phonic) and Tourette syndrome; however, evidence demonstrating increased tics is limited. Evaluate for tics and Tourette syndrome prior to therapy initiation (AACAP [Murphy 2013]; Pliszka 2007).
Special populations:
- Pediatric: Modafinil is not FDA-approved for use in pediatrics for any indication. Serious skin reactions and psychiatric events have been observed in pediatric patients treated with modafinil. The serious nature of these adverse effects resulted in the FDA’s Pediatric Advisory Committee unanimously recommending that a specific warning against the use of modafinil in children be added to the manufacturer's labeling.
Monitoring Parameters
Evaluate levels of sleepiness. Monitor blood pressure and heart rate; increased monitoring in patients with recent MI or unstable angina. Evaluate pregnancy status within 1 week prior to treatment initiation (in females of reproductive potential). Monitor for development of severe skin reactions; development or exacerbation of psychiatric symptoms (eg, agitation, anxiety, depression).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Outcome information following modafinil use in pregnancy is limited (Calvo-Ferrandiz 2018; Haervig 2014). Preliminary data from the Nuvigil/Provigil pregnancy registry suggest an increased risk of major fetal congenital malformations, including congenital cardiac anomalies (Alertec 2019). An increased risk of spontaneous abortion and intrauterine growth restriction has been reported with modafinil.
Evaluate pregnancy status within a week prior to modafinil initiation. Efficacy of steroidal contraceptives (including depot and implantable contraceptives) may be decreased; alternate means of effective contraception should be used during modafinil therapy and for ≥1 month after modafinil is discontinued.
Health care providers are encouraged to register pregnant patients exposed to modafinil, or pregnant females may enroll themselves, by calling (866-404-4106).
Patient Education
What is this drug used for?
- It is used to treat a lot of sleepiness that may happen with sleep apnea, narcolepsy, or shift work problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Anxiety
- Diarrhea
- Trouble sleeping
- Back pain
- Nausea
- Runny nose
- Stuffy nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Dark urine
- Yellow skin
- Change in amount of urine passed
- Unable to pass urine
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Shortness of breath
- Joint pain
- Muscle pain
- Sensing things that seem real but are not
- Behavioral changes
- Confusion
- Severe headache
- Dizziness
- Passing out
- Vision changes
- Chills
- Sore throat
- Swelling of arms or legs
- Bruising
- Bleeding
- Swollen glands
- Severe loss of strength and energy
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.