What is Nexplanon?
Nexplanon is a hormone-releasing birth control implant for use by women to prevent pregnancy for up to 3 years. The implant is a flexible plastic rod about the size of a matchstick that contains a progestin hormone called etonogestrel. It contains a small amount of barium sulfate so that the implant can be seen by X-ray, and may also contain magnesium stearate. Your healthcare provider will insert the implant just under the skin of the inner side of your upper arm. You can use a single Nexplanon implant for up to 3 years. Nexplanon does not contain estrogen.

What if I need birth control for more than 3 years?
The Nexplanon implant must be removed after 3 years. Your healthcare provider can insert a new implant under your skin after taking out the old one if you choose to continue using Nexplanon for birth control.
What if I change my mind about birth control and want to stop using Nexplanon before 3 years?
Your healthcare provider can remove the implant at any time. You may become pregnant as early as the first week after removal of the implant. If you do not want to get pregnant after your healthcare provider removes the Nexplanon implant, you should start another birth control method right away.
How does Nexplanon work?
Nexplanon prevents pregnancy in several ways. The most important way is by stopping the release of an egg from your ovary. Nexplanon also thickens the mucus in your cervix and this change may keep sperm from reaching the egg. Nexplanon also changes the lining of your uterus.
How well does Nexplanon work?
When the Nexplanon implant is placed correctly, your chance of getting pregnant is very low (less than 1 pregnancy per 100 women who use Nexplanon for 1 year). It is not known if Nexplanon is as effective in very overweight women because studies did not include many overweight women.
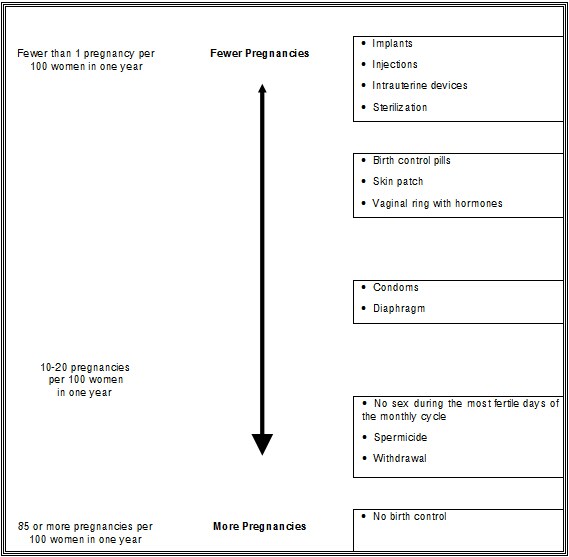
The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.
Who should not use Nexplanon?
Do not use Nexplanon if you:
- Are pregnant or think you may be pregnant
- Have, or have had blood clots, such as blood clots in your legs (deep venous thrombosis), lungs (pulmonary embolism), eyes (total or partial blindness), heart (heart attack), or brain (stroke)
- Have liver disease or a liver tumor
- Have unexplained vaginal bleeding
- Have breast cancer or any other cancer that is sensitive to progestin (a female hormone), now or in the past
- Are allergic to anything in Nexplanon
Tell your healthcare provider if you have or have had any of the conditions listed above. Your healthcare provider can suggest a different method of birth control.
What should I tell my healthcare provider about before using Nexplanon?
Talk to your healthcare provider about using Nexplanon if you:
- Have diabetes
- Have high cholesterol or triglycerides
- Have headaches
- Have gallbladder or kidney problems
- Have a history of depressed mood
- Have high blood pressure
- Have an allergy to numbing medicines (anesthetics) or medicines used to clean your skin (antiseptics). These medicines will be used when the implant is placed into or removed from your arm.
Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins and herbal supplements.
Certain medicines may make Nexplanon less effective, including:
- aprepitant
- barbiturates
- bosentan
- carbamazepine
- felbamate
- griseofulvin
- oxcarbazepine
- phenytoin
- rifampin
- St. John's wort
- topiramate
- HIV medicines
- Hepatitis C Virus medicines
Ask your healthcare provider if you are not sure if your medicine is one listed above.
If you are taking medicines or herbal products that might make Nexplanon less effective, you and your doctor may decide to leave Nexplanon in place; in that case, an additional non-hormonal contraceptive should be used. Because the effect of another medicine on Nexplanon may last up to 28 days after stopping the medicine, it is necessary to use the additional non-hormonal contraceptive for that long.
When you are using Nexplanon, tell all of your healthcare providers that you have Nexplanon in place in your arm.
How is the Nexplanon implant placed and removed?
Your healthcare provider will place and remove the Nexplanon implant in a minor surgical procedure in his or her office. The implant is placed just under the skin on the inner side of your nondominant upper arm.
The timing of insertion is important. Your healthcare provider may:
- Perform a pregnancy test before inserting Nexplanon
- Schedule the insertion at a specific time of your menstrual cycle (for example, within the first 5 days of your regular menstrual bleeding). If the implant is placed after the fifth day of menses, then you should use an additional contraceptive method (such as a condom) for the first 7 days after insertion.
Your healthcare provider will cover the site where Nexplanon was placed with 2 bandages. Leave the top bandage on for 24 hours. Keep the smaller bandage clean, dry, and in place for 3 to 5 days.
Immediately after the Nexplanon implant has been placed, you and your healthcare provider should check that the implant is in your arm by feeling for it.
If you cannot feel the implant immediately after insertion, the implant may not have been inserted, or it may have been inserted deeply. A deep insertion may cause problems with locating and removing the implant. Once the healthcare professional has located the implant, it should be removed.
If at any time you cannot feel the Nexplanon implant, contact your healthcare provider immediately and use a non-hormonal birth control method (such as condoms) until your healthcare provider confirms that the implant is in place. You may need special tests to check that the implant is in place or to help find the implant when it is time to take it out. If the implant cannot be found in the arm after a thorough search, your healthcare professional may use x-rays or other imaging methods on your chest.
Depending on the exact position of the implant, removal may be difficult and may require surgery.
You will be asked to review and sign a consent form prior to inserting the Nexplanon implant. You will also get a User Card to keep at home with your health records. Your healthcare provider will fill out the User Card with the date the implant was inserted and the date the implant is to be removed. Keep track of the date the implant is to be removed. Schedule an appointment with your healthcare provider to remove the implant on or before the removal date.
Be sure to have checkups as advised by your healthcare provider.
When should I call my healthcare provider?
Call your healthcare provider right away if you have:
- Pain in your lower leg that does not go away
- Severe chest pain or heaviness in the chest
- Sudden shortness of breath, sharp chest pain, or coughing blood
- Symptoms of a severe allergic reaction, such as swollen face, tongue or throat; trouble breathing or swallowing
- Sudden severe headache unlike your usual headaches
- Weakness or numbness in your arm, leg, or trouble speaking
- Sudden partial or complete blindness
- Yellowing of your skin or whites of your eyes, especially with fever, tiredness, loss of appetite, dark colored urine, or light-colored bowel movements
- Severe pain, swelling, or tenderness in the lower stomach (abdomen)
- Lump in your breast
- Problems sleeping, lack of energy, tiredness, or you feel very sad
- Heavy menstrual bleeding
What if I become pregnant while using Nexplanon?
You should see your healthcare provider right away if you think that you may be pregnant. It is important to remove the implant and make sure that the pregnancy is not ectopic (occurring outside the womb). Based on experience with other hormonal contraceptives, Nexplanon is not likely to cause birth defects.
Can I use Nexplanon when I am breastfeeding?
If you are breastfeeding your child, you may use Nexplanon if 4 weeks have passed since you had your baby. A small amount of the hormone contained in Nexplanon passes into your breast milk. The health of breast-fed children whose mothers were using the implant has been studied up to 3 years of age in a small number of children. No effects on the growth and development of the children were seen. If you are breastfeeding and want to use Nexplanon, talk with your healthcare provider for more information.
What are the possible side effects of Nexplanon?
The most common side effects of Nexplanon include:
- Changes in Menstrual Bleeding Patterns (menstrual periods). The most common side effect of Nexplanon is a change in your normal menstrual bleeding pattern. In studies, one out of ten women stopped using the implant because of an unfavorable change in their bleeding pattern. You may experience longer or shorter bleeding during your periods or have no bleeding at all. The time between periods may vary, and in between periods you may also have spotting. Tell your healthcare provider right away if:
- You think you may be pregnant
- Your menstrual bleeding is heavy and prolonged
Besides changes in menstrual bleeding patterns, other frequent side effects that caused women to stop using the implant include:
- Mood swings
- Weight gain
- Headache
- Acne
- Depressed mood
Other common side effects include:
- Headache
- Vaginitis (inflammation of the vagina)
- Weight gain
- Acne
- Breast pain
- Viral infections such as sore throats or flu-like symptoms
- Stomach pain
- Painful periods
- Mood swings, nervousness, or depressed mood
- Back pain
- Nausea
- Dizziness
- Pain
- Pain at the site of insertion
Implants have been reported to be found in a blood vessel, including a blood vessel in the lung which can be associated with shortness of breath, cough and/or the coughing up of blood or blood-stained mucus.
This is not a complete list of possible side effects. For more information, ask your healthcare provider for advice about any side effects that concern you. You may report side effects to the FDA at 1-800- FDA-1088.
What are the possible risks of using Nexplanon?
1. Problems with insertion and removal
The implant may not be placed in your arm at all due to a failed insertion. If this happens, you may become pregnant. Immediately after insertion, and with help from your healthcare provider, you should be able to feel the implant under your skin. If you can't feel the implant, tell your healthcare provider.
Location and removal of the implant may be difficult or impossible because the implant is not where it should be. Special procedures, including surgery in the hospital, may be needed to remove the implant. If the implant is not removed, then the effects of Nexplanon will continue for a longer period of time.
Implants have been found in the pulmonary artery (a blood vessel in the lung). If the implant cannot be found in the arm, your healthcare professional may use x-rays or other imaging methods on the chest. If the implant is located in the chest, surgery may be needed.
Other problems related to insertion and removal are:
- Pain, irritation, swelling, or bruising at the insertion site
- Scarring, including a thick scar called a keloid around the insertion site
- Infection
- Scar tissue may form around the implant making it difficult to remove
- The implant may come out by itself. You may become pregnant if the implant comes out by itself. Use a back-up birth control method and call your healthcare provider right away if the implant comes out.
- The need for surgery in the hospital to remove the implant
- Injury to nerves or blood vessels in your arm
- The implant breaks making removal difficult
2. Ectopic Pregnancy
If you become pregnant while using Nexplanon, you have a slightly higher chance that the pregnancy will be ectopic (occurring outside the womb) than do women who do not use birth control. Unusual vaginal bleeding or lower stomach (abdominal) pain may be a sign of ectopic pregnancy. Ectopic pregnancy is a medical emergency that often requires surgery. Ectopic pregnancies can cause serious internal bleeding, infertility, and even death. Call your healthcare provider right away if you think you are pregnant or have unexplained lower stomach (abdominal) pain.
3. Ovarian Cysts
Cysts may develop on the ovaries and usually go away without treatment but sometimes surgery is needed to remove them.
4. Breast Cancer
It is not known whether Nexplanon use changes a woman's risk for breast cancer. If you have breast cancer now, or have had it in the past, do not use Nexplanon because some breast cancers are sensitive to hormones.
5. Serious Blood Clots
Nexplanon may increase your chance of serious blood clots, especially if you have other risk factors such as smoking. It is possible to die from a problem caused by a blood clot, such as a heart attack or a stroke.
Some examples of serious blood clots are blood clots in the:
- Legs (deep vein thrombosis)
- Lungs (pulmonary embolism)
- Brain (stroke)
- Heart (heart attack)
- Eyes (total or partial blindness)
The risk of serious blood clots is increased in women who smoke. If you smoke and want to use Nexplanon, you should quit. Your healthcare provider may be able to help.
Tell your healthcare provider at least 4 weeks before if you are going to have surgery or will need to be on bed rest. You have an increased chance of getting blood clots during surgery or bed rest.
6. Other Risks
A few women who use birth control that contains hormones may get:
- High blood pressure
- Gallbladder problems
- Rare cancerous or noncancerous liver tumors
7. Broken or Bent Implant
If you feel that the implant may have broken or bent while in your arm, contact your healthcare provider.
General information about the safe and effective use of Nexplanon
This Patient Information leaflet contains important information about Nexplanon. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider for information about Nexplanon that is written for healthcare professionals. You may also call 1-800-622-4477 or visit www.NEXPLANON-USA.com.
How should I store Nexplanon?
Store at 25ºC (77ºF); excursions permitted to 15- 30ºC (59-86ºF).
Avoid storing Nexplanon at temperatures above 30ºC (86ºF).
Keep out of sight and reach of children.
What are the ingredients in Nexplanon?
Active ingredient: etonogestrel
Inactive ingredients: barium sulfate, magnesium stearate, ethylene-vinyl acetate copolymer, ethylene-vinyl acetate copolymer.

