Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Aerosol Solution, Translingual:
NitroMist: 400 mcg/spray (4.1 g, 8.5 g) [contains menthol]
Generic: 400 mcg/spray (4.1 g [DSC], 8.5 g [DSC])
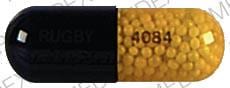
Capsule Extended Release, Oral:
Nitro-Time: 2.5 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Nitro-Time: 6.5 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Nitro-Time: 9 mg [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Generic: 2.5 mg [DSC], 6.5 mg [DSC], 9 mg [DSC]
Ointment, Rectal:
Rectiv: 0.4% (30 g) [contains propylene glycol]
Ointment, Transdermal:
Nitro-Bid: 2% (1 g, 30 g, 60 g)
Packet, Sublingual:
GoNitro: 400 mcg (1 ea, 36 ea)
Patch 24 Hour, Transdermal:
Minitran: 0.1 mg/hr (30 ea); 0.2 mg/hr (30 ea); 0.4 mg/hr (30 ea); 0.6 mg/hr (30 ea)
Nitro-Dur: 0.1 mg/hr (1 ea, 30 ea, 100 ea); 0.2 mg/hr (1 ea, 30 ea, 100 ea); 0.3 mg/hr (1 ea, 30 ea, 100 ea); 0.4 mg/hr (1 ea, 30 ea, 100 ea); 0.6 mg/hr (1 ea, 30 ea, 100 ea); 0.8 mg/hr (1 ea, 30 ea, 100 ea)
Generic: 0.1 mg/hr (1 ea, 30 ea, 4350 ea); 0.2 mg/hr (1 ea, 30 ea, 4350 ea); 0.4 mg/hr (1 ea, 30 ea, 4350 ea); 0.6 mg/hr (1 ea, 30 ea, 4350 ea)
Solution, Intravenous:
Nitronal: 1 mg/mL (25 mL [DSC], 50 mL [DSC])
Generic: 25 mg (250 mL); 50 mg (250 mL, 500 mL [DSC]); 100 mg (250 mL); 200 mg (500 mL [DSC]); 5 mg/mL (10 mL)
Solution, Translingual:
Nitrolingual: 0.4 mg/spray (4.9 g, 12 g) [contains alcohol, usp]
Generic: 0.4 mg/spray (4.9 g, 12 g)
Tablet Sublingual, Sublingual:
Nitrostat: 0.3 mg, 0.4 mg, 0.6 mg
Generic: 0.3 mg, 0.4 mg, 0.6 mg
Pharmacology
Mechanism of Action
Nitroglycerin forms free radical nitric oxide. In smooth muscle, nitric oxide activates guanylate cyclase which increases guanosine 3’5’ monophosphate (cGMP) leading to dephosphorylation of myosin light chains and smooth muscle relaxation. Produces a vasodilator effect on the peripheral veins and arteries with more prominent effects on the veins. Primarily reduces cardiac oxygen demand by decreasing preload (left ventricular end-diastolic pressure); may modestly reduce afterload; dilates coronary arteries and improves collateral flow to ischemic regions. For use in rectal fissures, intra-anal administration results in decreased sphincter tone and intra-anal pressure.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~3 L/kg
Metabolism
Extensive first-pass effect; metabolized hepatically to glycerol di- and mononitrate metabolites via liver reductase enzyme; subsequent metabolism to glycerol and organic nitrate; nonhepatic metabolism via red blood cells and vascular walls also occurs
Excretion
Urine (as inactive metabolites)
Onset of Action
Sublingual tablet: 1 to 3 minutes; Translingual spray: Similar to sublingual tablet; Extended release: ~60 minutes; Topical: 15 to 30 minutes; Transdermal: ~30 minutes; IV: Immediate
Peak effect: Sublingual powder: 7 minutes; Sublingual tablet: 5 minutes; Translingual spray: 4 to 15 minutes; Extended release: 2.5 to 4 hours; Topical: ~60 minutes; Transdermal: 120 minutes; IV: Immediate
Duration of Action
Sublingual tablet: At least 25 minutes; Translingual spray: Similar to sublingual tablet; Extended release: 4 to 8 hours (Gibbons 2003); Topical: 7 hours; Transdermal: 10 to 12 hours; IV: 3 to 5 minutes
Half-Life Elimination
~1 to 4 minutes
Protein Binding
60%
Use: Labeled Indications
Treatment or prevention of angina pectoris
Intravenous (IV) administration: Treatment or prevention of angina pectoris; acute decompensated heart failure (especially when associated with acute myocardial infarction); perioperative hypertension (especially during cardiovascular surgery); induction of intraoperative hypotension
Intra-anal administration (Rectiv ointment): Treatment of moderate-to-severe pain associated with chronic anal fissure
Use: Off Label
Esophageal spastic disordersc
Data from a limited number of patients studied suggest that nitroglycerin may be beneficial for the treatment of esophageal spastic disorders Swamy 1977. Additional data may be necessary to further define the role of nitroglycerin in this condition.
Gastroesophageal variceal hemorrhagebyes
Based on older controlled trials and updated American Association for the Study of Liver Diseases guidelines on the management of portal hypertensive bleeding in cirrhosis, the addition of nitroglycerin to vasopressin therapy may effectively control acute variceal bleeding and improve safety; however, significant systemic adverse effects associated with the combination limit the clinical use of vasopressin over other splanchnic vasoconstrictors
Sympathomimetic vasopressor extravasation injury (alternative to phentolamine)c
Clinical experience suggests the utility of topical nitroglycerin in the management of sympathomimetic vasopressor extravasations Hurst 2004, Reynolds 2014. Additional data may be necessary to further define the role of topical nitroglycerin in this condition.
Uterine relaxation (for uterine inversion)cyes
Data from a limited number of patients studied (case reports) suggest that IV nitroglycerin may be beneficial for uterine relaxation when uterine inversion occurs following childbirth Altabef 1992, Bayhi 1992, Dayan 1996.
Based on the American College of Obstetricians and Gynecologists guidelines for the treatment of postpartum hemorrhage, IV nitroglycerin is an option when uterine relaxation is needed in the management of uterine inversion ACOG 183 2017.
Contraindications
Hypersensitivity to nitroglycerin, other nitrates or nitrites, or any component of the formulation (includes adhesives for transdermal product); concurrent use with phosphodiesterase-5 (PDE-5) inhibitors (avanafil, sildenafil, tadalafil, or vardenafil); concurrent use with soluble guanylate cyclase (sGC) stimulators (eg, riociguat).
Additional contraindications for IV product: Hypersensitivity to corn or corn products (solutions containing dextrose); constrictive pericarditis; increased intracranial pressure; pericardial tamponade; restrictive cardiomyopathy; uncorrected hypovolemia
Additional contraindications for sublingual product and rectal ointment: Acute circulatory failure or shock (sublingual tablets and powder); early myocardial infarction (sublingual tablet only; see Note); increased intracranial pressure; severe anemia
Additional contraindications for translingual product: Increased intracranial pressure; severe anemia; acute circulatory failure or shock (Nitrolingual only)
Canadian labeling: Additional contraindications for translingual product (not in US labeling): Closed angle glaucoma; myocardial infarction; heart failure (aortic or mitral stenosis, constrictive pericarditis or hypertrophic obstructive cardiomyopathy).
Canadian labeling: Additional contraindications for transdermal patch (not in US labeling): Acute circulatory failure associated with marked hypotension (shock and states of collapse); orthostatic hypotension; myocardial insufficiency due to obstruction (eg, presence of aortic or mitral stenosis or of constrictive pericarditis); increased intracranial pressure; increased intraocular pressure; severe anemia.
Note: According to the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines of the management of ST-elevation myocardial infarction (STEMI) and the ACC/AHA guidelines for the management of patients with non-ST-elevation acute coronary syndromes (NSTE-ACS), avoid nitrates in the following conditions: Hypotension (SBP <90 mm Hg or ≥30 mm Hg below baseline), marked bradycardia or tachycardia, and right ventricular infarction (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]). Sublingual nitroglycerin may be used as initial treatment of ongoing chest pain in patients who may have STEMI or NSTE-ACS (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Dosage and Administration
Dosing: Adult
Note: Nitronal IV solution has been discontinued in the US for more than 1 year.
Note: Hemodynamic and antianginal tolerance often develop within 24 to 48 hours of continuous nitrate administration. Nitrate-free interval (10 to 12 hours/day) is recommended to avoid tolerance development; gradually decrease dose in patients receiving nitroglycerin for prolonged period to avoid withdrawal reaction.
Acute decompensated heart failure (off-label dose): IV: Initial: 10 to 20 mcg/minute, with subsequent titration (eg, 10 to 20 mcg/minute every 5 to 15 minutes) up to 200 mcg/minute (Coons 2011; Mebazaa 2016) or 0.3 to 0.5 mcg/kg/minute with titration (if SBP ≥90 mm Hg) in increments of 20 mcg/minute every 1 to 3 minutes up to 400 mcg/minute (Levy 2007). Patients who do not respond hemodynamically with doses of ~200 mcg/minute should be considered non-responders (Coons 2011).
Angina/coronary artery disease:
Oral: Initial: 2.5 to 6.5 mg 3 to 4 times daily; may titrate up to 26 mg 4 times daily
IV:
Initial: 10 mcg/minute, with subsequent titration to desired blood pressure effect (ACCF/AHA [O'Gara 2013])
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 5 mcg/minute, increase by 5 mcg/minute every 3 to 5 minutes to 20 mcg/minute. If no response at 20 mcg/minute, may increase by 10 to 20 mcg/minute every 3 to 5 minutes (generally accepted maximum dose: 400 mcg/minute)
Sublingual powder (0.4 mg/packet):
0.4 mg every 5 minutes up to 3 doses. Patients should be advised to take 1 dose promptly in response to chest pain. If pain is unrelieved or worsened 3 to 5 minutes after 1 dose, the patient or caregiver should call 9-1-1 immediately (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 1 to 2 packets under tongue every 5 minutes as needed for maximum of 3 packets in 15 minutes; may also use prophylactically 5 to 10 minutes prior to activities which may provoke an angina attack
Sublingual tablet:
0.3 to 0.4 mg every 5 minutes up to 3 doses. Patients should be advised to take 1 dose promptly in response to chest pain. If pain is unrelieved or worsened 3 to 5 minutes after 1 dose, the patient or caregiver should call 9-1-1 immediately (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 0.3 to 0.6 mg every 5 minutes for maximum of 3 tablets in 15 minutes; may also use prophylactically 5 to 10 minutes prior to activities which may provoke an attack.
Topical 2% ointment: 1/2” upon rising and 1/2” 6 hours later; if necessary, the dose may be doubled to 1” and subsequently doubled again to 2” if response is inadequate. Doses of 1/2” to 2” were used in clinical trials. Recommended maximum: 2 doses/day; include a nitrate free-interval ~10 to 12 hours/day.
Topical patch, transdermal: 0.2 to 0.4 mg/hour initially and titrate to doses of 0.4 to 0.8 mg/hour. Tolerance is minimized by using a patch-on period of 12 to 14 hours/day and patch-off period of 10 to 12 hours/day.
Translingual 0.4 mg/spray:
0.4 mg every 5 minutes up to 3 doses. Patients should be advised to take 1 dose promptly in response to chest pain. If pain is unrelieved or worsened 3 to 5 minutes after 1 dose, the patient or caregiver should call 9-1-1 immediately (ACC/AHA [Amsterdam 2014]; ACCF/AHA [O'Gara 2013]).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 1 to 2 sprays onto or under tongue approximately every 5 minutes for maximum of 3 sprays in 15 minutes; may also be used prophylactically 5 to 10 minutes prior to activities which may provoke an angina attack
Anal fissure, chronic (0.4% ointment): Intra-anal: 1 inch (equals 1.5 mg of nitroglycerin) every 12 hours for up to 3 weeks
Esophageal spastic disorders (off-label use): Sublingual: 0.3 to 0.6 mg (Swamy 1977). Additional data may be necessary to further define the role of nitroglycerin in this condition.
Gastroesophageal variceal hemorrhage (off-label use): IV infusion: Initial: 40 mcg/minute, increase by 40 mcg/minute every 15 minutes if systolic blood pressure is >90 to 100 mm Hg, up to a maximum of 400 mcg/minute (Garcia-Tsao 2007; Gimson 1986; Westaby 1989). Coadminister with vasopressin and use at the highest effective dose for a maximum of 24 hours to minimize the development of adverse effects (Garcia-Tsao 2007).
Sympathomimetic vasopressor extravasation injury (alternative to phentolamine) (off-label use; based on limited data): Topical 2% ointment: Apply a 1-inch strip to site of ischemia; may repeat every 8 hours if needed (Reynolds 2014). Additional data may be necessary to further define the role of topical nitroglycerin in this condition.
Uterine relaxation (for uterine inversion) (off-label use; based on limited data): IV: 50 mcg to relax the uterus when uterine inversion occurs following delivery; dose may be repeated if needed. Maximum total dose: 200 mcg (Altabef 1992; Bayhi 1992; Dayan 1996).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Nitronal IV solution has been discontinued in the US for more than 1 year.
Note: Continuous IV infusion dosing units vary by age (mcg/kg/minute or mcg/minute); extra precautions should be taken. Tolerance to the hemodynamic and antianginal effects can develop within 24 to 48 hours of continuous use. Nitrate-free interval (10 to 12 hours/day) is recommended to avoid tolerance development; gradually decrease dose in patients receiving nitroglycerin for prolonged periods to avoid withdrawal reaction.
Heart failure; cardiogenic shock: Limited data available:
Infants and Children: Continuous IV infusion: Initial: 0.25 to 0.5 mcg/kg/minute; titrate by 1 mcg/kg/minute every 15 to 20 minutes as needed; faster titration may be necessary in some patients; in adolescents, titration every 3 to 5 minutes has been suggested; usual dose range: 1 to 5 mcg/kg/minute; usual maximum dose: 10 mcg/kg/minute (AHA [Chameides 2011]; Artman 1987; Ilbawi 1985; Park 2014); doses up to 20 mcg/kg/minute may be used (Friedman 1985)
Adolescents: Continuous IV infusion: Initial: 5 to 10 mcg/minute; titrate every 3 to 5 minutes as needed to maximum rate of 200 mcg/minute (AHA [Chameides 2011]; Park 2014)
Extravasation (sympathomimetic vasopressors), treatment (alternative to phentolamine): Very limited data available; dosing based on experience in neonatal patients; optimal dosing has not been established: Infants, Children, and Adolescents: Topical: 2% ointment: 4 mm/kg applied as a thin ribbon to the affected areas; after 8 hours if no improvement, the dose may be repeated at the affected site (Wong 1992). The maximum reported dose is application of a 1-inch strip to the affected site in a neonate (Denkler 1989); however, this is greater than the usual initial adult dose (1/2 inch) for angina; hypotension may occur; carefully monitor blood pressure (Reynolds 2014). Note: Minimal data available from clinical trials/case reports; however, use has been described in reviews of extravasation treatment (Reynolds 2014; Treadwell 2012).
Reconstitution
Nitronal (glyceryl trinitrate) 1 mg/mL (temporarily available in the US):
To prepare a 100 mcg/mL solution: Withdraw 25 mL D5W from a 250 mL bottle of D5W and replace volume with 25 mg (25 mL) of Nitronal.
To prepare a 200 mcg/mL solution: Withdraw 50 mL D5W from a 250 mL bottle of D5W and replace volume with 50 mg (50 mL) of Nitronal.
Administration
IV: Prepare in glass bottles, EXCEL or PAB containers. Adsorption occurs to soft plastic (eg, PVC); use administration sets intended for nitroglycerin. Avoid in-line IV filters that adsorb nitroglycerin. Administer via infusion pump.
Intra-anal ointment: Using a finger covering (eg, plastic wrap, surgical glove, finger cot), place finger beside 1 inch measuring guide on the box and squeeze ointment the length of the measuring line directly onto covered finger. Insert ointment into the anal canal using the covered finger up to first finger joint (do not insert further than the first finger joint) and apply ointment around the side of the anal canal. If intra-anal application is too painful, may apply the ointment to the outside of the anus. Wash hands following application.
Extended release capsule: Swallow whole. Do not chew, break, or crush. Administer with a full glass of water.
Sublingual powder: Empty the contents of packet under the tongue, close mouth, and breathe normally. Allow powder to dissolve without swallowing. Do not rinse or spit for 5 minutes after dosing.
Sublingual tablet: Do not chew, crush, or swallow sublingual tablet. Place under tongue and allow to dissolve. Alternately, may be placed in the buccal pouch. May take small sip of water prior to placing tablet under the tongue to aid dissolution.
Topical ointment: Wash hands prior to and after use. Application site should be clean, dry, and hair-free. Apply to chest or back with the applicator or dose-measuring paper. Spread in a thin layer over a 2.25 x 3.5 inch area. Do not rub into skin. Tape applicator into place.
Sympathomimetic vasopressors extravasation injury (alternative to phentolamine) (off-label use): Stop vesicant infusion immediately and disconnect IV line (leave needle/cannula in place); gently aspirate extravasated solution from the IV line (do NOT flush the line); remove needle/cannula; elevate extremity. Apply nitroglycerin ointment as a thin ribbon to site of ischemia (Reynolds 2014; Wong 1992). May also apply dry warm compresses (Hurst 2004; Reynolds 2014).
Topical patch, transdermal: Application site should be clean, dry and hair-free. Remove patch after 12 to 14 hours. Rotate patch sites. Dispose of any used of unused patches by folding adhesive ends together, replace in pouch or sealed container and discard properly in trash, away from children and pets.
Translingual spray: Do not shake container. Prior to initial use, the pump must be primed by spraying 5 times (Nitrolingual) or 10 times (Nitromist) into the air. Priming sprays should be directed away from patient and others. Release spray onto or under tongue. Close mouth immediately after administration; do not inhale spray. Do not expectorate or rinse the mouth for 5 to 10 minutes following administration. Content of the container should be checked periodically; when the container is held upright, the end of the pump should be covered by the fluid in the bottle or the remaining sprays will not deliver the intended dose. If pump is unused for 6 weeks, a single priming spray (Nitrolingual) or 2 priming sprays (Nitromist) should be completed. If pump is unused for 3 months, re-prime with up to 5 sprays (Nitrolingual).
Storage
Extended-release capsules: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
IV solution: Store nitroglycerin premixed with dextrose at 25°C (77°F); brief exposure up to 40°C (104°F) does not adversely affect the product. Protect from light until time of use. Avoid excessive heat; protect from freezing. Nitroglycerin diluted in D5W or NS in glass containers is physically and chemically stable for 48 hours at room temperature and 7 days under refrigeration. In D5W or NS in EXCEL/PAB containers it is physically and chemically stable for 24 hours at room temperature.
Sublingual powder: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 5°C to 40°C (41°F to 104°F).
Sublingual tablets: Store at 20°C to 25°C (68°F to 77°F) in original glass container.
Transdermal patch: Store at 15°C to 30°C (59°F to 86°F)
Translingual spray: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Do not forcefully open or burn container after use. Do not spray toward flames.
Nitroglycerin Images
Drug Interactions
Alcohol (Ethyl): May enhance the vasodilatory effect of Vasodilators (Organic Nitrates). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Nitroglycerin. Monitor therapy
Alteplase: Nitroglycerin may decrease the serum concentration of Alteplase. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Anticholinergic Agents: May decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Apomorphine: Nitroglycerin may enhance the hypotensive effect of Apomorphine. Management: Patients taking apomorphine should lie down before and after taking sublingual nitroglycerin. Monitor blood pressure for hypotension and orthostatic hypotension when these agents are combined. Consider therapy modification
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Dapoxetine: May enhance the orthostatic hypotensive effect of Vasodilators (Organic Nitrates). Monitor therapy
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Ergot Derivatives: May diminish the vasodilatory effect of Nitroglycerin. This is of particular concern in patients being treated for angina. Nitroglycerin may increase the serum concentration of Ergot Derivatives. Exceptions: Nicergoline. Avoid combination
Heparin: Nitroglycerin may diminish the anticoagulant effect of Heparin. Nitroglycerin may decrease the serum concentration of Heparin. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Vasodilators (Organic Nitrates). Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the vasodilatory effect of Vasodilators (Organic Nitrates). Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Rilmenidine: Vasodilators (Organic Nitrates) may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Riociguat: Vasodilators (Organic Nitrates) may enhance the hypotensive effect of Riociguat. Avoid combination
Rosiglitazone: Vasodilators (Organic Nitrates) may enhance the adverse/toxic effect of Rosiglitazone. Specifically, a greater risk of ischemia and other adverse effects has been associated with this combination in some pooled analyses. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Test Interactions
IV formulation: Due to propylene glycol content, triglyceride assays dependent on glycerol oxidase may be falsely elevated.
Adverse Reactions
>10%: Central nervous system: Headache (patch, ointment: 50% to 64%; sublingual powder, lingual spray: >2%)
1% to 10%:
Cardiovascular: Hypotension (≤4%), syncope (≤4%), peripheral edema (lingual spray: ≤2%)
Central nervous system: Dizziness (>2% to 6%), paresthesia (>2%)
Gastrointestinal: Abdominal pain (lingual spray: ≤2%)
Neuromuscular & skeletal: Weakness (all sublingual forms: ≤2%)
Respiratory: Dyspnea (≤2%), pharyngitis (lingual spray: ≤2%), rhinitis (lingual spray: ≤2%)
Frequency not defined:
Cardiovascular: Bradycardia, exacerbation of angina pectoris, flushing, orthostatic hypotension
Dermatologic: Diaphoresis
Gastrointestinal: Vomiting
Miscellaneous: Drug tolerance
<1%, postmarketing, and/or case reports: Anaphylactoid reaction, application site irritation (patch), circulatory shock, contact dermatitis (ointment, patch), drowsiness, exfoliative dermatitis, fixed drug eruption (ointment, patch), hypersensitivity reaction, hypoxemia (transient), lactic acidosis (Smith 2019), methemoglobinemia, nausea, pallor, palpitations, rebound hypertension, restlessness, skin rash, tachycardia, vertigo, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Headache: Dose-related headaches may occur, especially during initial dosing.
- Hypotension/bradycardia: Severe hypotension and shock may occur (even with small doses); paradoxical bradycardia and increased angina pectoris may accompany hypotension. Orthostatic hypotension may also occur; ethanol may accentuate this. Use with caution in volume depletion, preexisting hypotension, constrictive pericarditis, aortic or mitral stenosis, and extreme caution with inferior wall MI and suspected right ventricular involvement. According to the ACCF/AHA, avoid use in patients with severe hypotension (SBP <90 mm Hg or ≥30 mm Hg below baseline), marked bradycardia or tachycardia, and right ventricular MI (ACCF/AHA [O'Gara 2013]).
- Increased intracranial pressure: Nitroglycerin may precipitate or aggravate increased intracranial pressure and subsequently may worsen clinical outcomes in patients with neurologic injury (eg, intracranial hemorrhage, traumatic brain injury) (Rangel-Castilla 2008). Some products are contraindicated in patients with increased intracranial pressure.
Disease-related concerns:
- Hypertrophic cardiomyopathy (HCM): Avoid use in patients with HCM with outflow tract obstruction; nitrates may reduce preload, exacerbating obstruction and cause hypotension or syncope and/or worsening of heart failure (ACCF/AHA [Gersh, 2011]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Intra-anal ointment: Use caution when treating rectal anal fissures with nitroglycerin in patients with suspected or known significant cardiovascular disorders (eg, cardiomyopathies, heart failure, acute MI); intra-anal nitroglycerin administration may decrease systolic blood pressure and decrease arterial vascular resistance.
- Long-acting agents: Avoid use of long-acting agents in acute MI or acute HF; cannot easily reverse effects if adverse events develop.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
- Transdermal patches: May contain conducting metal (eg, aluminum); remove patch prior to MRI.
Other warnings/precautions:
- Tolerance: May occur; cross tolerance to other nitro compounds have been reported. Appropriate dosing is needed to minimize tolerance development.
Monitoring Parameters
Blood pressure, heart rate; consult individual institutional policies and procedures
Pregnancy
Pregnancy Considerations
Nitroglycerin crosses the placenta (David 2000).
Following a single maternal IV bolus dose of nitroglycerin at the time of incision prior to cesarean delivery, concentrations in the umbilical cord at birth were significantly lower than the maternal plasma (~1 minute after dosing); a wide variation in maternal plasma concentrations was observed (David 2000). Following application of a transdermal patch 0.4 mg/hour to pregnant women 20 to 36 weeks gestation, concentrations of nitroglycerin were low but detectable in the fetal serum ~1 to 4 hours after the patch was applied (fetal/maternal ratio: 0.23) (Bustard 2003).
Intravenous nitroglycerin is recommended in pregnant females when preeclampsia is associated with pulmonary edema (ESC [Regitz-Zagrosek 2018]). Nitroglycerin may be beneficial in cases of uterine inversion following delivery when immediate relaxation of the uterus is needed (ACOG 183 2017). Additional data may be necessary to further define the role of nitroglycerin use in other conditions requiring uterine relaxation, such as external cephalic version, retained placenta, or preterm labor (Abdel-Aleem 2015; Axemo 1998; Caponas 2001; Cluver 2015; Duckitt 2014).
Patient Education
What is this drug used for?
Rectal:
- It is used to treat anal pain.
Injection:
- It is used to treat high blood pressure.
- It is used to treat heart failure (weak heart).
- It is used to treat chest pain or pressure.
All other products:
- It is used to treat chest pain or pressure.
- It is used to prevent chest pain or pressure.
All products:
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Burning or tingling of mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Persistent headache
- Fast heartbeat
- Slow heartbeat
- Flushing
- Blurred vision
- Dry mouth
- Sweating a lot
- Pale skin
- Severe nausea
- Severe vomiting
- Abnormal heartbeat
- Agitation
- Severe loss of strength and energy
- Chest pain
- Severe skin irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.