Boxed Warning
Neuropsychiatric disorders:
Mefloquine should not be prescribed for prophylaxis in patients with major psychiatric disorders. During prophylactic use, if psychiatric or neurologic symptoms occur, the drug should be discontinued and an alternative medication should be substituted.
Neuropsychiatric effects:
Mefloquine may cause neuropsychiatric adverse reactions that can persist after mefloquine has been discontinued.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
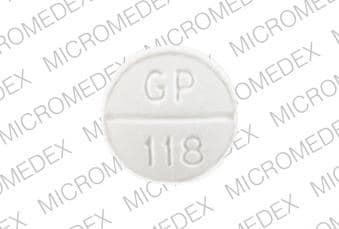
Tablet, Oral, as hydrochloride:
Generic: 250 mg
Pharmacology
Mechanism of Action
Mefloquine is a quinoline-methanol compound structurally similar to quinine; mefloquine's effectiveness in the treatment and prophylaxis of malaria is due to the destruction of the asexual blood forms of the malarial pathogens that affect humans, Plasmodium falciparum, P. vivax
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Distributes into tissues, erythrocytes, blood, urine, CSF
Vd: Children 4 to 10 years: Mean: ~18 to 19 L/kg (Price 1999); Adults: ~20 L/kg
Metabolism
Extensively hepatic primarily by CYP3A4 to 2,8-bis-trifluoromethyl-4-quinoline carboxylic acid (inactive) and other metabolites
Excretion
Primarily bile and feces; urine (9% of total dose as unchanged drug, 4% of total dose as primary metabolite)
Time to Peak
Plasma: ~17 hours (range: 6 to 24 hours)
Half-Life Elimination
Children 4 to 10 years: Mean range: 11.6 to 13.6 days (range: 6.5 to 33 days) (Price 1999); Adults: ~3 weeks (range: 2 to 4 weeks); may be decreased during infection (2 weeks) (WHO 2010)
Protein Binding
~98%
Use: Labeled Indications
Acute malaria infections: Treatment of mild to moderate acute malaria caused by mefloquine-susceptible strains of Plasmodium falciparum (both chloroquine-susceptible and -resistant strains) or by Plasmodium vivax.
Prophylaxis of malaria: Prophylaxis of P. falciparum and P. vivax malaria infections, including prophylaxis of chloroquine-resistant strains of P. falciparum.
Note: Due to geographical resistance and cross-resistance, consult current CDC guidelines.
Use: Off Label
Treatment of uncomplicated, chloroquine-resistant P. vivax malariayes
Based on the World Health Organization (WHO) Guidelines for the Treatment of Malaria and the Center for Disease Control and Prevention (CDC) Treatment of Malaria guidelines, mefloquine given for the treatment of uncomplicated, chloroquine-resistant P. vivax malaria is effective and recommended in the management of this condition.
Contraindications
Hypersensitivity to mefloquine, related compounds (eg, quinine and quinidine), or any component of the formulation; prophylactic use in patients with a history of seizures or psychiatric disorder (including active or recent history of depression, generalized anxiety disorder, psychosis, schizophrenia, or other major psychiatric disorders)
Documentation of allergenic cross-reactivity for quinine derivatives is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Malaria: Oral (dose expressed as mg of mefloquine hydrochloride):
Mild-to-moderate, treatment: 1,250 mg (5 tablets) as a single dose. Note: If clinical improvement is not seen within 48 to 72 hours, an alternative therapy should be used for re-treatment.
Uncomplicated, treatment (off-label dose): 750 mg (3 tablets) as initial dose, followed 6 to 12 hours later by 500 mg (2 tablets) (CDC 2013b)
Uncomplicated, chloroquine-resistant P. vivax malaria treatment (off-label use): 750 mg (3 tablets) as initial dose, followed 6 to 12 hours later by 500 mg (2 tablets) with concomitant primaquine (CDC 2013b)
Chemoprophylaxis: 250 mg weekly starting 1 week (CDC 2014: ≥2 weeks) before arrival in endemic area, continuing weekly during travel and for 4 weeks after leaving endemic area. Note: Prophylaxis may begin 2 to 3 weeks prior to travel to ensure tolerance.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dose is expressed in terms of the salt, mefloquine hydrochloride. Due to geographical resistance and cross-resistance, consult current CDC or WHO guidelines as appropriate.
Malaria, treatment; chloroquine-resistant (independent of HIV status): Note: Therapy is recommended as a last-line option due to higher rate of severe neuropsychiatric reactions; consider other treatment regimens first (CDC 2013):
CDC Guidelines (CDC 2013; HHS [pediatric OI 2017]): Infants, Children, and Adolescents: Oral: 15 mg/kg once (maximum dose: 750 mg/dose) followed in 6 to 12 hours with 10 mg/kg once (maximum dose: 500 mg/dose); use in combination with other anti-malarial agents (refer to local resistance patterns and guidelines); if clinical improvement is not seen within 48 to 72 hours, an alternative therapy should be used for retreatment
Malaria; chemoprophylaxis (independent of HIV status): Note: Begin ≥2 weeks before arrival in endemic area, administer on the same day each week, and continue weekly during travel and for 4 weeks after leaving endemic area (CDC 2018). Infants, Children, and Adolescents:
Weight-based dosing: Oral: 5 mg/kg/dose once weekly; maximum dose: 250 mg/dose (CDC 2018; HHS [pediatric OI 2017])
Fixed dosing (CDC 2018): Oral:
>9 to 19 kg: 62.5 mg (1/4 of 250 mg tablet) once weekly
>19 to 30 kg: 125 mg (1/2 of 250 mg tablet) once weekly
>30 to 45 kg: 187.5 mg (3/4 of a 250 mg tablet) once weekly
>45 kg: 250 mg once weekly
Administration
Administer with food and with at least 240 mL of water. When used for malaria prophylaxis, dose should be taken once weekly on the same day each week. If vomiting occurs within 30 minutes after the dose, an additional full dose should be given; if it occurs within 30 to 60 minutes after dose, an additional half-dose should be given. Tablets may be crushed and suspended in a small amount of water, milk, or another beverage for persons unable to swallow tablets.
Dietary Considerations
Take with food and with at least 240 mL of water.
Storage
Store at 20°C to 25°C (68°F to 77°F).
Mefloquine Images
Drug Interactions
Aminoquinolines (Antimalarial): May enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Mefloquine may increase the serum concentration of Aminoquinolines (Antimalarial). Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of an aminoquinoline antimalarial when possible. Avoid combination
Amodiaquine: May enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for vision problems may be increased. Monitor therapy
Anticonvulsants: Mefloquine may diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Antipsychotic Agents (Phenothiazines): Antimalarial Agents may increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Artemether: May enhance the adverse/toxic effect of Antimalarial Agents. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Celiprolol: Mefloquine may enhance the bradycardic effect of Celiprolol. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Systemic): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Dapsone (Topical): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Topical). Specifically, the risk of hemolytic reactions may be increased. Management: Closely monitor for signs/symptoms of hemolytic reactions with concomitant use of topical dapsone and antimalarial agents. Patients with glucose-6-phosphate dehydrogenase deficiency may be at particularly high risk for adverse hematologic effects. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Halofantrine: Mefloquine may enhance the QTc-prolonging effect of Halofantrine. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: Antimalarial Agents may enhance the adverse/toxic effect of Lumefantrine. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNIDine: May enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of quinidine when possible. Avoid combination
QuiNINE: May enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Mefloquine may increase the serum concentration of QuiNINE. Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of quinine when possible. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
>10%: Central nervous system: Abnormal dreams (14%; Tickell-Painter 2017), insomnia (13%; Tickell-Painter 2017)
1% to 10%: Gastrointestinal: Vomiting (3%)
<1%, postmarketing, and/or case reports: Abdominal pain, abnormal sensory symptoms, abnormal T waves on ECG, aggressive behavior, agitation, agranulocytosis, alopecia, anaphylaxis, anorexia, aplastic anemia, arthralgia, asthenia, ataxia, atrioventricular block, auditory impairment, bradycardia, burning sensation, cardiac arrhythmia, cardiac conduction disturbance (transient), chest pain, chills, confusion, decreased hematocrit, depression, diarrhea, dizziness, drowsiness, dyspepsia, dyspnea, ECG changes, edema, emotional disturbance, emotional lability, encephalopathy, equilibrium disturbance, erythema, erythema multiforme, extrasystoles, fatigue, fever, first degree atrioventricular block, flushing, hallucination, headache, hepatic disease, hepatic failure, hyperhidrosis, hypersensitivity reaction, hypertension, hypotension, increased serum transaminases, insomnia, leukocytosis, leukopenia, loose stools, malaise, memory impairment, muscle cramps, myalgia, myasthenia, nausea, pain, palpitations, panic attack, paranoia, paresthesia, pneumonitis (possibly allergic), polyneuropathy, prolonged Q-T interval on ECG, pruritus, psychotic reaction, restlessness, seizure, sensorimotor neuropathy, sinus arrhythmia, sinus bradycardia, skin rash, Stevens-Johnson syndrome, suicidal ideation (causal relationship not established), syncope, tachycardia, telogen effluvium, thrombocytopenia, tinnitus, tremor, urticaria, vertigo, vestibular disturbance, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- Agranulocytosis/aplastic anemia: Agranulocytosis and aplastic anemia have been reported.
- Altered cardiac conduction: Mefloquine may cause alterations in the ECG including sinus bradycardia, sinus arrhythmia, first-degree AV block, QT-interval prolongation, and abnormal T waves. Use caution or avoid concomitant use of agents known to cause QT-interval prolongation (eg, halofantrine, quinine, quinidine).
- Hypersensitivity reactions: Hypersensitivity reactions have occurred.
- Neuropsychiatric effects: [US Boxed Warning]: May cause neuropsychiatric adverse effects that can persist after mefloquine has been discontinued. During prophylactic use, if symptoms occur, discontinue therapy and substitute an alternative medication. Symptoms may develop early in the course of therapy. Due to the difficulty in identifying these symptoms in infants and children, monitor closely especially in pediatric patients. Psychiatric symptoms may include anxiety, paranoia, depression, hallucinations, and psychosis. Suicidal ideation and suicide have also been reported. Neurologic symptoms of dizziness or vertigo, tinnitus, and loss of balance may also occur and have been reported to be permanent in some cases. During prophylactic use, the occurrence of psychiatric symptoms such as acute anxiety, depression, restlessness, or confusion may be a prodrome to more serious neuropsychiatric adverse reactions. Use caution in activities requiring alertness and fine motor coordination (eg, driving, piloting planes, operating machinery) with neurologic symptoms.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with significant cardiac disease; ECG changes (eg, sinus bradycardia, sinus arrhythmia, first-degree AV block, QT-interval prolongation, abnormal T waves) have been reported.
- Hepatic impairment: Use with caution in patients with hepatic impairment; elimination may be prolonged.
- Neuropsychiatric disorders: [US Boxed Warning]: Do not prescribe for prophylaxis in patients with major psychiatric disorders including patients with active depression, a recent history of depression, generalized anxiety disorder, psychosis, schizophrenia; use is contraindicated in these patients. Use with caution in patients with a previous history of depression.
- Ocular effects: Eye disorders (including optic neuropathy and retinal disorders) have been reported during treatment. If visual symptoms develop during treatment, prompt ophthalmologic evaluation is warranted; discontinuation of therapy may be necessary.
- Plasmodium falciparum infections: Appropriate use: In cases of life-threatening, serious, or overwhelming malaria infections due to Plasmodium falciparum, patients should be treated with intravenous antimalarial drug. Mefloquine may be given orally to complete the course.
- Plasmodium vivax infections: Appropriate use: In cases of acute Plasmodium vivax infection treated with mefloquine, patients should subsequently be treated with an 8-aminoquinoline derivative (eg, primaquine) to avoid relapse.
- Seizure disorder: When using for treatment, use with caution in patients with a history of seizures; may increase risk of seizures. Prophylactic use is contraindicated in patients with seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Early vomiting leading to treatment failure in children has been reported in some studies; consider alternate therapy if a second dose is not tolerated.
Other warnings/precautions:
- Appropriate use: Not recommended for the treatment of malaria acquired in Southeast Asia due to drug resistance (CDC 2013b).
- Prolonged use: If mefloquine is to be used for a prolonged period, liver function tests, evaluations for neuropsychiatric effects, and ophthalmic examinations should be performed periodically.
Monitoring Parameters
When use is prolonged, periodic liver function tests, evaluations for neuropsychiatric effects, and ocular examinations
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Mefloquine crosses the placenta; however, clinical experience with mefloquine has not shown an increased risk of adverse effects in pregnant women. Malaria infection in pregnant women may be more severe than in nonpregnant women and may increase the risk of adverse pregnancy outcomes. CDC treatment guidelines are available for the use of mefloquine in the treatment of malaria during pregnancy (CDC 2013b).
Nonpregnant women of childbearing potential are advised to use contraception and avoid pregnancy during mefloquine therapy and for 3 months thereafter.
Patient Education
What is this drug used for?
- It is used to treat or prevent malaria.
Frequently reported side effects of this drug
- Headache
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Lack of appetite
- Loss of strength and energy
- Muscle pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Aplastic anemia like fever, sore throat, mouth sores, infections, bruising, or purple skin splotches
- Severe dizziness
- Passing out
- Agitation
- Change in balance
- Noise or ringing in the ears
- Anxiety
- Paranoia
- Depression
- Seizures
- Confusion
- Mood changes
- Behavioral changes
- Hallucination
- Abnormal heartbeat
- Slow heartbeat
- Chest pain
- Fast heartbeat
- Vision changes
- Eye pain
- Severe eye irritation
- Trouble sleeping
- Thoughts of suicide
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.