Boxed Warning
Complex sleep behaviors:
Complex sleep behaviors, including sleep-walking, sleep-driving, and engaging in other activities while not fully awake, may occur following use of zaleplon. Some of these events may result in serious injuries, including death. Discontinue zaleplon immediately if a patient experiences a complex sleep behavior.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
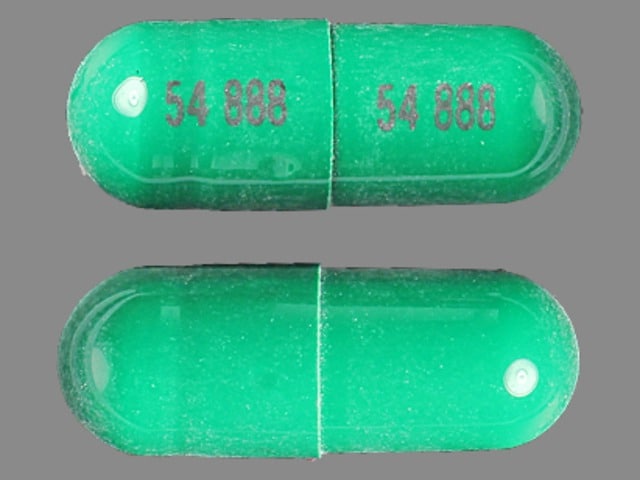
Capsule, Oral:
Sonata: 5 mg [DSC], 10 mg [DSC] [contains tartrazine (fd&c yellow #5)]
Generic: 5 mg, 10 mg
Pharmacology
Mechanism of Action
Zaleplon is unrelated to benzodiazepines, barbiturates, or other hypnotics. However, it interacts with the benzodiazepine GABA receptor complex. Nonclinical studies have shown that it binds selectively to the brain omega-1 receptor situated on the alpha subunit of the GABA-A receptor complex.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and almost complete; high-fat meal delays absorption
Distribution
Vd: ~1.4 L/kg
Metabolism
Extensive, primarily via aldehyde oxidase to form 5-oxo-zaleplon and, to a lesser extent, by CYP3A4 to desethylzaleplon; all metabolites are pharmacologically inactive
Excretion
Urine (~70% primarily metabolites, <1% as unchanged drug); feces (~17%)
Clearance: Plasma: Oral: 3 L/hour/kg
Onset of Action
Rapid
Time to Peak
Serum: ~1 hour
Half-Life Elimination
~1 hour
Protein Binding
~45% to 75%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Oral Cl was reduced 70% and 87% in compensated and decompensated cirrhotic patients, respectively.
Special Populations: Race
Cmax and AUC were increased 37% and 64%, respectively in Asian populations.
Use: Labeled Indications
Insomnia: Short-term treatment of insomnia (ie, up to 30 days).
Contraindications
Hypersensitivity to zaleplon or any component of the formulation; patients who have experienced complex sleep behaviors after taking zaleplon.
Dosage and Administration
Dosing: Adult
Insomnia: Oral: Usual dosage 10 mg immediately before bedtime (range: 5 to 20 mg); 5 mg may be sufficient for certain low weight patients (maximum dose: 20 mg/day). Has been used for up to 5 weeks of treatment in controlled trial setting.
Debilitated patients: Oral: Usual dosage 5 mg immediately before bedtime (maximum dose: 10 mg/day)
Concomitant therapy: 5 mg initially should be given to patients concomitantly taking cimetidine.
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Administration
Oral: Administer immediately before bedtime or when the patient is in bed and cannot fall asleep. Do not take with, or immediately following, a high-fat meal (may delay onset).
Dietary Considerations
Avoid taking with or after a heavy, high-fat meal; reduces absorption.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Zaleplon Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetidine: May increase the serum concentration of Zaleplon. Management: The initial dose of zaleplon should be limited to 5 mg in patients taking cimetidine. Monitor patients for increased zaleplon effects/toxicities (ie, sedation, CNS depression) when these agents are combined. Consider therapy modification
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Zaleplon. Management: Consider the use of an alternative hypnotic that is not metabolized by CYP3A4 in patients receiving strong CYP3A4 inducers. If zalephon is combined with a strong CYP3A4 inducer, monitor for decreased effectiveness of zaleplon. Consider therapy modification
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the sedative effect of Hypnotics (Nonbenzodiazepine). Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: Hypnotics (Nonbenzodiazepine) may enhance the CNS depressant effect of Sodium Oxybate. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%: Central nervous system: Headache (42%)
1% to 10%:
Cardiovascular: Chest pain (≥1%), peripheral edema (≤1%)
Central nervous system: Dizziness (9%), drowsiness (5% to 6%), amnesia (2% to 4%), paresthesia (3%), altered sense of smell (2%), depersonalization (2%), hypoesthesia (2%), malaise (2%), hyperacusis (1% to 2%), abnormality in thinking (≥1%), anxiety (≥1%), depression (≥1%), migraine (≥1%), nervousness (≥1%), hallucination (1%), hypertonia (1%), vertigo (1%)
Dermatologic: Pruritus (≥1%), skin rash (≥1%), skin photosensitivity (1%)
Gastrointestinal: Nausea (8%), abdominal pain (6%), anorexia (2%), constipation (≥1%), dysgeusia (≥1%), dyspepsia (≥1%), xerostomia (≥1%), colitis (1%)
Genitourinary: Dysmenorrhea (3% to 4%)
Neuromuscular & skeletal: Asthenia (7%), tremor (2%), arthralgia (≥1%), arthritis (≥1%), back pain (≥1%), myalgia (≥1%)
Ophthalmic: Eye pain (3% to 4%), visual disturbance (2%), conjunctivitis (≥1%)
Otic: Otalgia (≤1%)
Respiratory: Bronchitis (≥1%), epistaxis (1%)
Miscellaneous: Fever (≥1%)
<1%: Abnormal gait, abnormal hepatic function tests, abnormal uterine bleeding, accommodation disturbance, acne vulgaris, ageusia, agitation, albuminuria, alopecia, anaphylaxis, anemia, angina pectoris, apathy, aphthous stomatitis, apnea, arthropathy, asthma, ataxia, bigeminy, biliary colic, bladder pain, blepharitis, blepharoptosis, bruxism, bundle branch block, bursitis, cataract, central nervous system stimulation, cerebral ischemia, cheilitis, chills, cholelithiasis, confusion, conjunctival hyperemia (subconjunctival hemorrhage), contact dermatitis, corneal erosion, cyanosis, cystitis, deafness, decreased libido, delusions, diabetes mellitus, diaphoresis, diplopia, dry eye syndrome, duodenal ulcer, dysarthria, dysphagia, dyspnea, dystonia, dysuria, ecchymoses, eczema, edema, emotional lability, enteritis, eosinophilia, eructation, esophageal achalasia, esophagitis, euphoria, facial edema, facial paralysis, flatulence, gastritis, gastroenteritis, gingival hemorrhage, gingivitis, glaucoma, glossitis, goiter, gout, hangover effect, heavy menstrual bleeding, hematuria, hemorrhage (eye), hiccups, hostility, hyperbilirubinemia, hypercholesterolemia, hyperesthesia, hyperglycemia, hyperkinetic muscle activity, hyperreflexia, hypertension, hyperuricemia, hyperventilation, hypoglycemia, hypokinesia, hyporeflexia, hypotension, hypothyroidism, hypotonia, impaired consciousness, impotence, increased appetite, increased bronchial secretions, increased serum alanine aminotransferase, increased serum aspartate aminotransferase, increased thirst, insomnia, intestinal obstruction, irregular menses, ketosis, labyrinthitis, laryngitis, leukocytosis, leukorrhea, lymphadenopathy, lymphocytosis, maculopapular rash, mastalgia, melanosis, melena, menopause, menstrual disease, myasthenia, myoclonus, myositis, neck stiffness, nephrolithiasis, neuralgia, neuropathy, nightmares, nystagmus disorder, oral mucosa ulcer, oral paresthesia, orthostatic hypotension, osteoporosis, palpitations, paradoxical central nervous system stimulation, peptic ulcer, pericardial effusion, photophobia, pleural effusion, pneumonia, psoriasis, psychomotor retardation, pulmonary embolism, purpuric disease, pustular rash, rectal hemorrhage, renal pain, reduced urine flow, retinal detachment, sialorrhea, sinus bradycardia, skin discoloration, skin hypertrophy, slurred speech, snoring, stomatitis, stupor, substernal pain, syncope, tachycardia, tenosynovitis, thrombophlebitis, tinnitus, tongue discoloration, tongue edema, trismus, urethritis, urinary frequency, urinary incontinence, urinary retention, urinary urgency, urticaria, vaginal hemorrhage, vaginitis, vasodilatation, ventricular premature contractions, ventricular tachycardia, visual field defect, voice disorder, watery eyes, weight gain, weight loss, xeroderma
Frequency not defined:
Central nervous system: Central nervous system depression, complex sleep-related disorder
Hypersensitivity: Angioedema, hypersensitivity condition
Postmarketing: Anaphylaxis, nightmares, nonimmune anaphylaxis
Warnings/Precautions
Concerns related to adverse effects:
- Abnormal thinking/behavioral changes: Hypnotics/sedatives have been associated with abnormal thinking and behavior changes including decreased inhibition, aggression, bizarre behavior, agitation, hallucinations, and depersonalization. Amnesia and other neuropsychiatric symptoms may occur unpredictably and may indicate previously unrecognized psychiatric disorders; evaluate appropriately.
- CNS depression: May cause CNS depression impairing physical and mental capabilities; caution patients about performing tasks that require mental alertness (eg, operating machinery, driving). The risk of next-day psychomotor impairment is increased if patient is unable to stay in bed for a full night of sleep (7 to 8 hours), if a higher-than-recommended dose is taken, and/or if coadministered with other CNS depressants or other drugs that increase the blood levels of zaleplon. Dose adjustment may be necessary if taking concomitant CNS depressants; use with other sedative-hypnotics at bedtime or in the middle of the night is not recommended.
- Complex sleep behaviors: [US Boxed Warning]: Complex sleep behaviors, including sleep-walking, sleep-driving, and engaging in other activities while not fully awake, may occur following the use of zaleplon. Some of these events may result in serious injuries, including death. Other complex sleep behaviors (eg, preparing and eating food, making phone calls, having sex) while asleep have also been reported. Patients usually do not remember these events. May occur with first use and at recommended dosages with or without the use of alcohol or other CNS depressants. Discontinue immediately if a patient experiences a complex sleep behavior; use is contraindicated in patients who have experienced these events.
- Hypersensitivity reactions: Hypersensitivity reactions, including anaphylaxis, as well as angioedema, have been reported. Do not rechallenge patient if such reactions occur.
Disease-related concerns:
- Depression: Use with caution in patients with depression; worsening of depression, including suicide or suicidal ideation, has been reported with the use of hypnotics. Intentional overdose may be an issue in this population. The minimum dose that will effectively treat the individual patient should be used. Prescriptions should be written for the smallest quantity consistent with good patient care.
- Drug abuse: Use with caution in patients with a history of drug dependence, benzodiazepine abuse, or benzodiazepine-like hypnotic abuse.
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage adjustment recommended in mild to moderate impairment. Use is not recommended in patients with severe impairment.
- Respiratory disease: Use with caution in patients with respiratory compromise, chronic obstructive pulmonary disease, or sleep apnea.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated patients: Use with caution in debilitated patients; increased risk of impaired cognitive and/or motor performance. Dosage adjustment recommended; monitor closely.
- Elderly: Increased risk of impaired cognitive and/or motor performance and falls; monitor closely.
Dosage form specific issues:
- Tartrazine (FDC yellow #5): Capsules contain tartrazine; avoid in patients with sensitivity; reactions may be more frequently seen in patients with aspirin hypersensitivity; use caution in patients with asthma.
Other warnings/precautions:
- Appropriate use: Symptomatic treatment of insomnia should be initiated only after careful evaluation of potential causes of sleep disturbance. Failure of sleep disturbance to resolve after 7 to 10 days may indicate psychiatric and/or medical illness.
- Rapid onset: Because of the rapid onset of action, administer immediately prior to bedtime or after the patient has gone to bed and is having difficulty falling asleep.
- Withdrawal: Abrupt discontinuation or rapid dose decreases may lead to withdrawal symptoms.
Monitoring Parameters
Daytime alertness; fall risk; respiratory rate (patients with compromised respiration); behavior changes; tolerance, abuse, and dependence; reevaluate if insomnia persists after 30 days of use.
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies. A small study of pregnant women did not show an increased risk of teratogenic effects when used early in pregnancy (Wikner 2011). Use during pregnancy is not recommended by the manufacturer.
Patient Education
What is this drug used for?
- It is used to treat sleep problems.
Frequently reported side effects of this drug
- Headache
- Dizziness
- Abdominal pain
- Day fatigue
- Loss of strength or energy
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Confusion
- Sensing things that seem real but are not
- Trouble with memory
- Numbness or tingling feeling
- Change in balance
- Engaging in activities and not remembering
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.