Boxed Warning
Fetal toxicity:
When pregnancy is detected, discontinue irbesartan as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Avapro: 75 mg, 150 mg, 300 mg
Generic: 75 mg, 150 mg, 300 mg
Pharmacology
Mechanism of Action
Irbesartan is an angiotensin receptor antagonist. Angiotensin II acts as a vasoconstrictor. In addition to causing direct vasoconstriction, angiotensin II also stimulates the release of aldosterone. Once aldosterone is released, sodium as well as water are reabsorbed. The end result is an elevation in blood pressure. Irbesartan binds to the AT1 angiotensin II receptor. This binding prevents angiotensin II from binding to the receptor thereby blocking the vasoconstriction and the aldosterone secreting effects of angiotensin II.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and complete
Distribution
Vd: 53 to 93 L
Metabolism
Hepatic, via glucuronide conjugation and oxidation; oxidation occurs primarily by cytochrome P450 isoenzyme CYP2C9
Excretion
Feces (80%); urine (20%)
Onset of Action
Peak levels in 1 to 2 hours
Maximum effect: 3-6 hours postdose; with chronic dosing maximum effect: ~2 weeks
Time to Peak
Serum: 1.5 to 2 hours
Duration of Action
>24 hours
Half-Life Elimination
Terminal: 11 to 15 hours
Protein Binding
Plasma: 90%, primarily to albumin and alpha-1 acid glycoprotein
Use in Specific Populations
Special Populations: Race
In healthy black patients, AUC values were approximately 25% greater than white patients.
Use: Labeled Indications
Diabetic nephropathy: Treatment of diabetic nephropathy with an elevated serum creatinine and proteinuria (>300 mg/day) in patients with type 2 diabetes and hypertension
Hypertension: Management of hypertension
Guideline recommendations: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults recommends if monotherapy is warranted, in the absence of comorbidities (eg, cerebrovascular disease, chronic kidney disease, diabetes, heart failure, ischemic heart disease, etc.), that thiazide-like diuretics or dihydropyridine calcium channel blockers may be preferred options due to improved cardiovascular endpoints (eg, prevention of heart failure and stroke). ACE inhibitors and ARBs are also acceptable for monotherapy. Combination therapy may be required to achieve blood pressure goals and is initially preferred in patients at high risk (stage 2 hypertension or atherosclerotic cardiovascular disease [ASCVD] risk ≥10%) (ACC/AHA [Whelton 2017]).
Use: Off Label
Acute coronary syndrome (secondary prevention of cardiovascular events)yes
Based on the American Heart Association/American College of Cardiology (AHA/ACC) guidelines for the management of patients with non-ST-elevation acute coronary syndromes (NSTE-ACS) and the American College of Cardiology Foundation/American Heart Association (ACC/AHA) guidelines for the management of patients with STE-ACS, an ARB is recommended and effective in patients with NSTE-ACS or STE-ACS who have indications for but are intolerant of ACE inhibitors; this includes patients with heart failure, MI, or anterior MI who have a left ventricular ejection fraction (LVEF) ≤40%. In post-STE-ACS patients, initiate within the first 24 hours.
Stable coronary artery diseaseyes
Based on the American College of Cardiology/American Heart Association guideline for the diagnosis and management of patients with stable ischemic heart disease, an ACE inhibitor or ARB should be prescribed in all patients with stable ischemic heart disease who also have hypertension, diabetes mellitus, LVEF <40%, or CKD unless contraindicated.
Contraindications
Hypersensitivity to irbesartan or any component of the formulation; concomitant use with aliskiren in patients with diabetes mellitus
Documentation of allergenic cross-reactivity for angiotensin receptor blockers is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Concomitant use with aliskiren in patients with moderate to severe renal impairment (GFR <60 mL/minute/1.73 m2); concomitant use with ACE inhibitors in patients with diabetic nephropathy; hereditary galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption; pregnancy; breastfeeding
Dosage and Administration
Dosing: Adult
Hypertension: Oral: 150 mg once daily; titrate as needed based on patient response up to 300 mg once daily (ACC/AHA [Whelton 2017]); maximum dose: 300 mg/day. Note: Starting dose in volume-depleted patients should be 75 mg.
Diabetic nephropathy: Oral: 300 mg once daily
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Hypertension: Limited data available (AAP [Flynn 2017]; NHLBI 2011; Sakarcan 2001): Note: Use a lower starting dose of 50% of the recommended initial dose in volume- and salt-depleted patients.
Children ≥6 years: Oral: Initial: 75 mg once daily; may be titrated to a maximum dose of 150 mg once daily
Adolescents: Oral: Initial: 150 mg once daily; may be titrated to a maximum dose of 300 mg once daily
Proteinuria reduction in children with chronic kidney disease: Limited data available: Children ≥4 years and Adolescents: Oral: Studies utilized a fixed dosage based on weight categories (see the following); initial doses were approximately 2 mg/kg once daily; doses were increased after 3 to 5 weeks and again after 8 to 12 weeks if needed, according to specific blood pressure criteria; median final dose in the largest study (n=44; median age: 10 years): 4 mg/kg once daily (Franscini 2002; Gartenmann 2003; von Vigier 2000)
10 to 20 kg: Initial: 37.5 mg once daily
21 to 40 kg: Initial: 75 mg once daily
>40 kg: Initial: 150 mg once daily
Administration
Oral: Administer with or without food.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
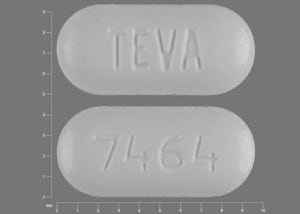
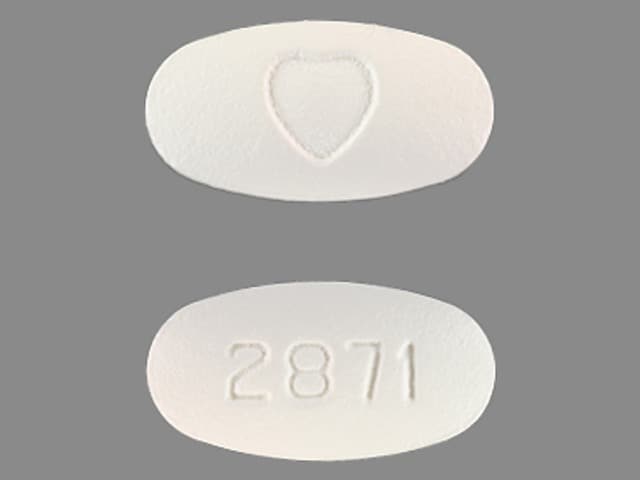
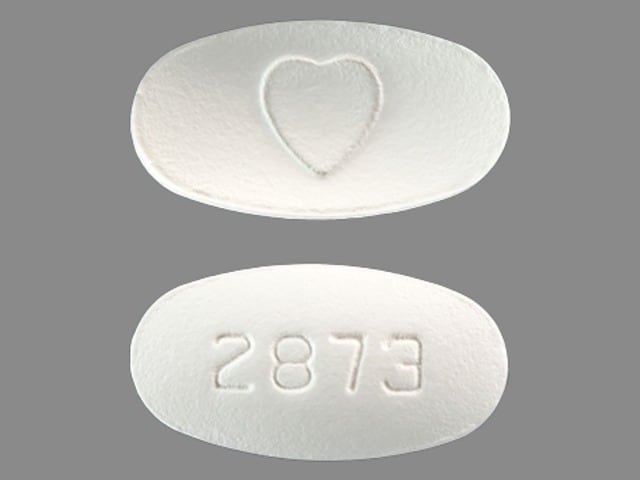
Irbesartan Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Aliskiren: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the hypotensive effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the nephrotoxic effect of Angiotensin II Receptor Blockers. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II: Receptor Blockers may diminish the therapeutic effect of Angiotensin II. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Angiotensin II Receptor Blockers may enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Angiotensin II Receptor Blockers may increase the serum concentration of Angiotensin-Converting Enzyme Inhibitors. Management: In US labeling, use of telmisartan and ramipril is not recommended. It is not clear if any other combination of an ACE inhibitor and an ARB would be any safer. Consider alternatives to the combination when possible. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
CycloSPORINE (Systemic): Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of CycloSPORINE (Systemic). Monitor therapy
Dapoxetine: May enhance the orthostatic hypotensive effect of Angiotensin II Receptor Blockers. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Drospirenone: Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Drospirenone. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eplerenone: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Heparin: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lithium: Angiotensin II Receptor Blockers may increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an angiotensin II receptor antagonist. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Angiotensin II Receptor Blockers may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents. Specifically, the combination may result in a significant decrease in renal function. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Angiotensin II Receptor Blockers. The combination of these two agents may also significantly decrease glomerular filtration and renal function. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Potassium-Sparing Diuretics: Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Ranolazine: May enhance the adverse/toxic effect of Angiotensin II Receptor Blockers. Monitor therapy
Sodium Phosphates: Angiotensin II Receptor Blockers may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with ARBs, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, maintain adequate hydration and monitor renal function closely. Consider therapy modification
Tacrolimus (Systemic): Angiotensin II Receptor Blockers may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Tolvaptan: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Trimethoprim: May enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Unless otherwise indicated, incidences are reported for patients with hypertension.
>10%: Endocrine & metabolic: Hyperkalemia (diabetic nephropathy: 19%)
1% to 10%:
Cardiovascular: Orthostatic dizziness (diabetic nephropathy: 5%), orthostatic hypotension (diabetic nephropathy: 5%)
Central nervous system: Dizziness (diabetic nephropathy: 10%), fatigue (4%)
Gastrointestinal: Diarrhea (3%), dyspepsia (≤2%), heartburn (≤2%)
<1%, postmarketing, and/or case reports: Anaphylactic shock, anaphylaxis, anemia (case report; Simonetti 2007), angioedema, facial edema, hepatitis, increased creatine phosphokinase, increased liver enzymes, jaundice, lip edema, pharyngeal edema, thrombocytopenia, tinnitus, tongue edema, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Angioedema: Angioedema has been reported rarely with some angiotensin II receptor antagonists (ARBs) and may occur at any time during treatment (especially following first dose). It may involve the head and neck (potentially compromising airway) or the intestine (presenting with abdominal pain). Patients with idiopathic or hereditary angioedema or previous angioedema associated with ACE-inhibitor therapy may be at an increased risk. Prolonged frequent monitoring may be required, especially if tongue, glottis, or larynx are involved, as they are associated with airway obstruction. Patients with a history of airway surgery may have a higher risk of airway obstruction. Discontinue therapy immediately if angioedema occurs. Aggressive early management is critical. Intramuscular (IM) administration of epinephrine may be necessary. Do not readminister to patients who have had angioedema with ARBs.
- Hyperkalemia: May occur; risk factors include renal dysfunction, diabetes mellitus, concomitant use of potassium-sparing diuretics, potassium supplements and/or potassium containing salts. Use cautiously, if at all, with these agents and monitor potassium closely.
- Hypotension: Symptomatic hypotension may occur upon initiation in patients who are salt- or volume-depleted (eg, those treated with high-dose diuretics); correct volume depletion prior to administration. This transient hypotensive response is not a contraindication to further treatment with irbesartan.
- Renal function deterioration: May be associated with deterioration of renal function and/or increases in serum creatinine, particularly in patients with low renal blood flow (eg, renal artery stenosis, chronic kidney disease, severe heart failure, volume depletion) whose glomerular filtration rate (GFR) is dependent on efferent arteriolar vasoconstriction by angiotensin II; deterioration may result in oliguria, acute renal failure, and progressive azotemia. Small increases in serum creatinine may occur following initiation; consider discontinuation only in patients with progressive and/or significant deterioration in renal function.
Disease-related concerns:
- Aortic/mitral stenosis: Use with caution in patients with significant aortic/mitral stenosis.
- Ascites: Avoid use in patients with ascites due to cirrhosis or refractory ascites; if use cannot be avoided in patients with ascites due to cirrhosis, monitor blood pressure and renal function carefully to avoid rapid development of renal failure (AASLD [Runyon 2012]).
- Renal artery stenosis: Use with caution in patients with unstented unilateral/bilateral renal artery stenosis. When unstented bilateral renal artery stenosis is present, use is generally avoided due to the elevated risk of deterioration in renal function unless possible benefits outweigh risks.
- Renal impairment: Use with caution with preexisting renal insufficiency.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pregnancy: [US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
- Surgical patients: In patients on chronic angiotensin receptor blocker (ARB) therapy, intraoperative hypotension may occur with induction and maintenance of general anesthesia; however, discontinuation of therapy prior to surgery is controversial. If continued preoperatively, avoidance of hypotensive agents during surgery is prudent (Hillis 2011). Based on current research and clinical guidelines in patients undergoing noncardiac surgery, continuing angiotensin-receptor blockers (ARB) is reasonable in the perioperative period. If ARBs are held before surgery, it is reasonable to restart postoperatively as soon as clinically feasible (ACC/AHA [Fleisher 2014]).
Monitoring Parameters
Blood pressure; electrolytes, serum creatinine, BUN, urinalysis
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year atherosclerotic cardiovascular disease (ASCVD) risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
[US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. When pregnancy is detected, discontinue as soon as possible. The use of drugs which act on the renin-angiotensin system are associated with oligohydramnios. Oligohydramnios, due to decreased fetal renal function, may lead to fetal lung hypoplasia and skeletal malformations. Oligohydramnios may not appear until after irreversible fetal injury has occurred. Use in pregnancy is also associated with anuria, hypotension, renal failure, skull hypoplasia, and death in the fetus/neonate. The exposed fetus should be monitored for fetal growth, amniotic fluid volume, and organ formation. Infants exposed in utero should be monitored for hyperkalemia, hypotension, and oliguria (exchange transfusions or dialysis may be needed). These adverse events are generally associated with maternal use in the second and third trimesters.
Chronic maternal hypertension itself is also associated with adverse events in the fetus/infant. The risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death may be increased with chronic hypertension in pregnancy. Actual risks may be related to duration and severity of maternal hypertension (ACOG 203 2019).
The use of angiotensin II receptor blockers is generally not recommended to treat chronic hypertension in pregnant women and should generally be avoided in women planning a pregnancy (ACOG 203 2019).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to protect kidney function in diabetic patients who have protein loss.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling.
- Severe dizziness
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.