What is peripheral arterial disease?
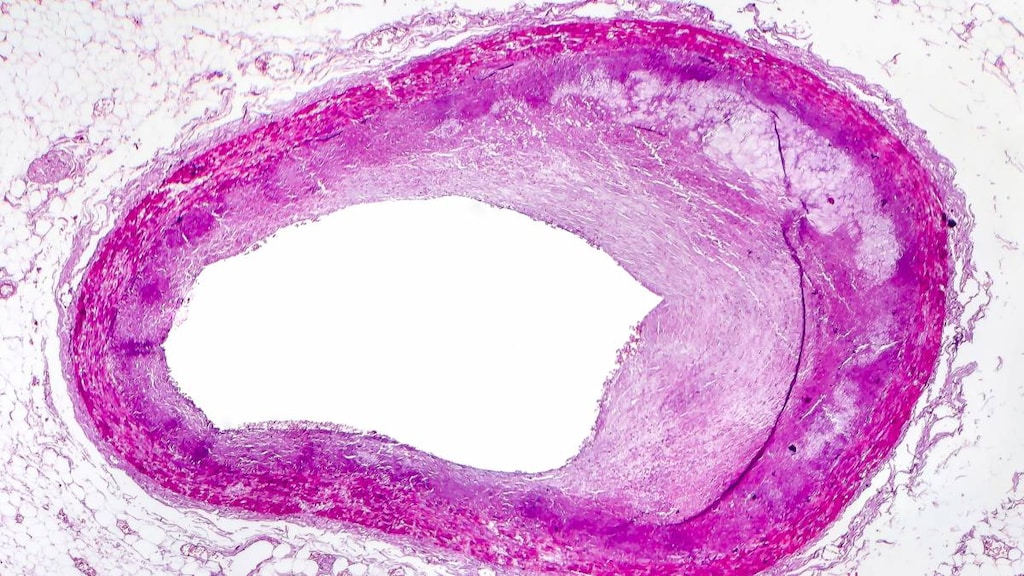
Peripheral arterial disease is a common disorder of the blood vessels in which plaque builds up in the arteries that carry blood to your brain, heart, other organs, and limbs, reducing blood flow and therefore oxygen delivery to these areas.
Peripheral arterial disease may also be called peripheral artery disease or PAD.
What causes peripheral arterial disease?
Peripheral arterial disease is usually caused by atherosclerosis which is a process during which fats and other substances in the blood (such as calcium, dead cells, and platelets) form a fatty deposit called a plaque, narrowing and hardening the artery and restricting blood flow.
Other less common causes of peripheral arterial disease include inflammation of the blood vessels, limb injury, deformities, or a history of radiation exposure.
The condition usually affects most arteries throughout the body, including the heart. When it affects the arteries supplying blood to the legs, it is called peripheral arterial disease.
People more at risk of peripheral arterial disease include those:
- Over the age of 65
- Over the age of 50 with a history of diabetes or smoking
- Under the age of 50 who are obese or have high blood pressure
- High cholesterol
- A family history of peripheral arterial disease, heart disease, or stroke
- High levels of homocysteine, which is a component of protein that helps build and maintain tissue.
What are the symptoms of peripheral arterial disease?
Symptoms of Peripheral Arterial Disease reflect the decrease in blood flow and therefore the lack of oxygen delivery to affected areas of your body. People with mild disease may have no symptoms but others may experience:
- Leg pain or cramping while walking (this is called claudication) or doing other types of physical activity such as climbing stairs, but this tends to disappear with rest. The location of the pain depends on the artery affected but calf pain is the most common location. The severity of the pain varies from mild discomfort to debilitating pain. Pain can be so severe it restricts people from doing any physical activity
- Discoloration of the legs
- Erectile dysfunction in men
- Hair loss or a slowing of hair growth on the feet and legs
- Numbness or weakness in the legs
- One side of the lower leg or foot feels colder than the other
- Poor healing of wounds or cuts on your legs, feet, or toes
- A shiny look to the legs
- Slower toenail growth
- A weak pulse or no pulse in the legs or feet.
As the condition progresses, pain may occur during rest or when lying down and be intense enough to disrupt sleep. If left untreated, infections or skin injuries may progress and cause tissue death (gangrene), sometimes requiring amputation of the affected limb. A person’s risk of having a stroke or a heart attack is also increased.
How is peripheral arterial disease diagnosed?
See a doctor if you develop leg pain, numbness or other problems when walking. Your doctor will perform a physical examination, listen to the pulses in your feet and legs, and conduct further tests if necessary, before making a diagnosis.
How is peripheral arterial disease treated?
Lifestyle changes, such as stopping smoking, exercising, and eating a healthy diet will help reduce the risk of peripheral arterial disease from developing. Treating conditions, such as diabetes, high cholesterol, and high blood pressure also lowers risk.
Because the condition is likely to be a sign of more widespread accumulation of fatty deposits in the arteries, treatments aim to treat the whole body, not just the areas with symptoms and may include:
- Cholesterol-lowering drugs
- Anti-platelet agents
- Anticoagulants
- Surgery, such as bypass grafting, angioplasty, and stent placement
- Atherectomy, which is a procedure that removes plaque buildup from an artery.




