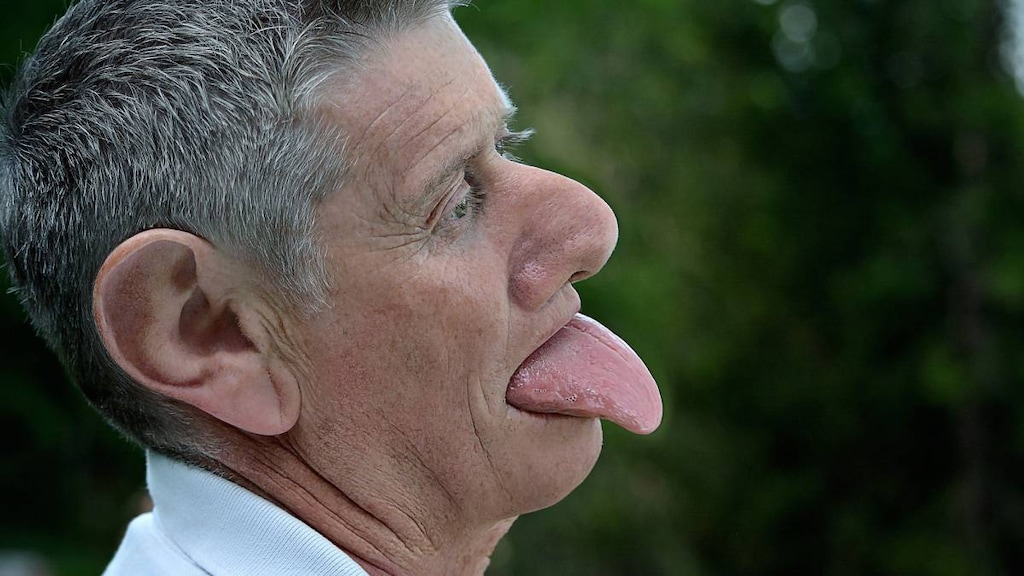
Tardive dyskinesia (TD) is a side effect most often caused by antipsychotic medications. Symptoms include uncontrollable, repetitive facial movements, such as fast blinking of the eyes, smacking of the lips, sticking out the tongue, and grimacing. Antipsychotics are a type of medicine that is used to treat mental health conditions such as schizophrenia.
What causes tardive dyskinesia?
Most cases of TD are caused by antipsychotics, usually following long-term use, although occasionally it develops soon after initiation if dosages are high.
Antipsychotics are thought to work by affecting different neurotransmitters in the brain, such as dopamine, which plays a vital role in emotional wellbeing and in controlling our movements. Tardive dyskinesia was historically thought to develop because antipsychotics block dopamine receptors inhibiting the release of dopamine. However, it is now believed that other neurotransmitters, such as acetylcholine and serotonin are also involved because tardive dyskinesia can develop with other medications that have less of an effect on dopamine.
Generally, the incidence of TD is higher with older (first-generation) antipsychotics, although newer, atypical antipsychotics can also cause TD. Rates of TD of over 30% have been reported with the following older antipsychotics:
- Chlorpromazine
- Haloperidol
- Fluphenazine
- Perphenazine.
Rates of around 13% have been reported with the following newer (second-generation) antipsychotics:
- Aripiprazole
- Lurasidone
- Olanzapine
- Paliperidone
- Quetiapine
- Risperidone
- Ziprasidone.
Other medications that have been associated with TD include:
- Antidepressants, such as amitriptyline, clomipramine, doxepin, and trazodone (more common in elderly patients), selective serotonin reuptake inhibitors (SSRIs; such as fluoxetine or sertraline), monoamine oxidase inhibitors (MAOI; such as selegiline, rasagiline, and phenelzine)
- Antiparkinsons’ agents
- Anxiolytics such as benzodiazepines and barbiturates
- Hydroxyzine
- Metoclopramide (risk is increased with more than 12 weeks usage)
- Lithium, especially in combination with antipsychotics
- Prochlorperazine
- Procyclidine (TD induced by this drug may be reversible)
- Rarely, carbamazepine and lamotrigine, decongestants, or chloroquine.
Stimulants, such as caffeine, nicotine, ginseng, amphetamines can exacerbate or precipitate TD.
Other factors that also increase a person’s risk include:
- Older age (over 55)
- Diabetes
- Being female, particularly postmenopausal
- Having dementia or prior head trauma
- African, African American, or Asian-American descent
- Having an alcohol or a substance-use disorder.
What are the symptoms of tardive dyskinesia?
Symptoms can range from a slight tremor to uncontrollable movements of the whole body. They usually come on gradually and usually appear while taking a medication, although can appear months or even years after stopping the drug. Symptoms may include:
- Facial grimacing or frowning
- Repetitive tongue thrusting
- Pursing or smacking the lips
- Chewing or chomping
- Grunting
- Excessive blinking
- Wriggling of the fingers
- Flapping of the arms
- Thrusting of the pelvis
- Swaying
- Tapping of the feet.
Seek treatment early if you develop symptoms of TD.
How is tardive dyskinesia diagnosed?
Your doctor will ask you questions about your medication history and perform a physical examination.
For a diagnosis of TD, according to the DSM-V criteria, the symptoms have to persist for at least a month after the medication is discontinued.
Your doctor may also conduct other tests to rule out other conditions, such as cerebral palsy, Parkinson’s disease, or Huntington’s disease.
How is tardive dyskinesia treated?
Seek treatment early if you develop symptoms of TD.
Valbenazine (Ingrezza) and Deutetrabenazine (Austedo) may be used for the treatment of TD.
Treatment may also include:
- Withdrawal of the medication (this should be done slowly and only on a doctor’s advice)
- Supplements of antioxidants or branched-chain amino acids (BCAA)
- Cholinergic agents
- Clozapine, quetiapine, or olanzapine
- Clonazepam
- Propranolol
- Amantadine
- Gingko Biloba.
In most people TD is irreversible and persists for long after the medication is stopped. Stopping the medication may, therefore, not be recommended by some doctors as this may cause further complications.




