Boxed Warning
Hepatotoxicity:
This product contains acetaminophen. Severe liver damage may occur if a person takes: more than 4,000 mg of acetaminophen in 24 hours; with other drugs containing acetaminophen; with 3 or more alcoholic drinks every day while using this product.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
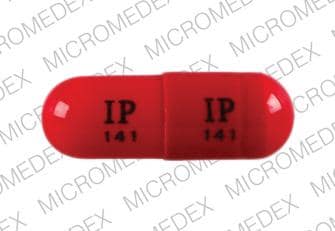
Capsule, Oral:
Nodolor: Acetaminophen 325 mg, isometheptene mucate 65 mg, and dichloralphenazone 100 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Generic: Acetaminophen 325 mg, isometheptene mucate 65 mg, and dichloralphenazone 100 mg [DSC]
Pharmacology
Mechanism of Action
Acetaminophen: Although not fully elucidated, the analgesic effects are believed to be due to activation of descending serotonergic inhibitory pathways in the CNS. Interactions with other nociceptive systems may be involved as well (Smith 2009). Antipyresis is produced from inhibition of the hypothalamic heat-regulating center.
Dichloralphenazone: Prodrug, converted to chloral hydrate (sedative) and antipyrine (analgesic/antipyretic) that reduces patient’s emotional response to painful stimuli
Isometheptene: A sympathomimetic that reduces stimuli leading to vascular headaches via constriction of dilated cranial and cerebral arterioles
Use: Labeled Indications
Headache: Relief of tension headache and vascular headache (potentially effective for relief of migraine headache).
Contraindications
Hypersensitivity to isometheptene, dichloralphenazone, acetaminophen, or any component of the formulation; cardiovascular or cerebrovascular insufficiency (eg, recent MI, stroke); glaucoma; severe renal disease; hypertension; organic heart disease; peripheral vascular disease; hepatic disease; concomitant monoamine oxidase inhibitor (MAOI) therapy
Dosage and Administration
Dosing: Adult
Migraine headache: Oral: Two capsules to start, followed by 1 capsule every hour until relief is obtained (maximum: 5 capsules/12 hours)
Tension headache: Oral: 1 to 2 capsules every 4 hours (maximum: 8 capsules/day)
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Administer without regard to food.
Storage
Store at 15°C to 30°C (59°F to 86°F).
Acetaminophen, Isometheptene, and Dichloralphenazone Images
Drug Interactions
Alcohol (Ethyl): May enhance the hepatotoxic effect of Acetaminophen. Monitor therapy
Alpha1-Blockers: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Barbiturates: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Exceptions: Amobarbital; Butabarbital; Butalbital; Methohexital; PENTobarbital; Secobarbital; Thiopental. Monitor therapy
Busulfan: Acetaminophen may increase the serum concentration of Busulfan. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
CarBAMazepine: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Monitor therapy
Chloroprocaine: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Dasatinib: Acetaminophen may enhance the hepatotoxic effect of Dasatinib. Dasatinib may increase the serum concentration of Acetaminophen. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Ergot Derivatives: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. Avoid combination
Flucloxacillin: May enhance the adverse/toxic effect of Acetaminophen. Specifically, the risk for high anion gap metabolic acidosis may be increased. Monitor therapy
Fosphenytoin-Phenytoin: May decrease the serum concentration of Acetaminophen. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of the toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Imatinib: Acetaminophen may enhance the hepatotoxic effect of Imatinib. Monitor therapy
Isoniazid: May enhance the adverse/toxic effect of Acetaminophen. Monitor therapy
LamoTRIgine: Acetaminophen may decrease the serum concentration of LamoTRIgine. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
MetyraPONE: May increase the serum concentration of Acetaminophen. More importantly, by inhibiting the conjugative metabolism of acetaminophen, metyrapone may shift the metabolism towards the oxidative route that produces a hepatotoxic metabolite. Monitor therapy
Mipomersen: Acetaminophen may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the adverse/toxic effect of Isometheptene. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Phenylephrine (Systemic): Acetaminophen may increase the serum concentration of Phenylephrine (Systemic). Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probenecid: May increase the serum concentration of Acetaminophen. Probenecid may also limit the formation of at least one major non-toxic metabolite, possibly increasing the potential for formation of the toxic NAPQI metabolite. Consider therapy modification
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the tachycardic effect of Alpha-/Beta-Agonists. Serotonin/Norepinephrine Reuptake Inhibitors may enhance the vasopressor effect of Alpha-/Beta-Agonists. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
SORAfenib: Acetaminophen may enhance the hepatotoxic effect of SORAfenib. SORAfenib may increase the serum concentration of Acetaminophen. Consider therapy modification
Spironolactone: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the vasopressor effect of Alpha-/Beta-Agonists. Management: Avoid, if possible, the use of alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Acetaminophen may enhance the anticoagulant effect of Vitamin K Antagonists. This appears most likely with daily acetaminophen doses exceeding 1.3 or 2 g/day for multiple consecutive days. Monitor therapy
Test Interactions
Acetaminophen may cause false urine glucose, urine catecholamine, and urinary 5-hydroxyindoleacetic acid test results.
Adverse Reactions
Frequency not defined.
Central nervous system: Dizziness (transient)
Dermatologic: Skin rash
Warnings/Precautions
Concerns related to adverse events:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Hepatotoxicity: [U.S. Boxed Warning]: Acetaminophen may cause severe hepatotoxicity, potentially requiring liver transplant or resulting in death; hepatotoxicity is usually associated with excessive acetaminophen intake (>4 g/day). Risk is increased with alcohol use (eg, ≥3 drinks per day), preexisting liver disease, and intake of more than one source of acetaminophen-containing medications. Chronic daily dosing in adults has also resulted in liver damage in some patients.
- Hypersensitivity: Hypersensitivity and anaphylactic reactions have been reported with acetaminophen use; discontinue immediately if symptoms of allergic or hypersensitivity reactions occur.
- Skin reactions: Rarely, acetaminophen may cause serious and potentially fatal skin reactions such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). Discontinue treatment if severe skin reactions develop.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Disease-related concerns:
- Cardiovascular disease: Use is contraindicated in cardiovascular or cerebrovascular insufficiency (eg, recent MI, stroke), hypertension, organic heart disease, and peripheral vascular disease.
- G6PD deficiency: Use with caution in patients with known G6PD deficiency; rare reports of hemolysis have occurred with acetaminophen use.
- Hepatic impairment: Use is contraindicated in patients with hepatic disease.
- Renal impairment: Use is contraindicated in patients with severe renal disease.
Other warning/precautions:
- Dosage limit: Limit acetaminophen dose from all sources (prescription, OTC) ≤4 g/day (adults).
Monitoring Parameters
Relief of pain
Patient Education
What is this drug used for?
- It is used to treat headaches.
Frequently reported side effects of this drug
- Dizziness
- Fatigue
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.