Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Albenza: 200 mg [contains saccharin sodium]
Generic: 200 mg
Pharmacology
Mechanism of Action
Active metabolite, albendazole sulfoxide, causes selective degeneration of cytoplasmic microtubules in intestinal and tegmental cells of intestinal helminths and larvae; glycogen is depleted, glucose uptake and cholinesterase secretion are impaired, and desecratory substances accumulate intracellulary. ATP production decreases causing energy depletion, immobilization, and worm death.
Pharmacokinetics/Pharmacodynamics
Absorption
Poor from the GI tract; may increase up to 5 times when administered with a fatty meal
Distribution
Widely distributed throughout the body including urine, bile, liver, cyst wall, cyst fluid, and CSF
Metabolism
Hepatic; extensive first-pass effect; pathways include rapid sulfoxidation to active metabolite (albendazole sulfoxide [major]), hydrolysis, and oxidation
Excretion
Urine (<1% as active metabolite); feces
Time to Peak
Serum: 2 to 5 hours for the metabolite
Half-Life Elimination
8 to 12 hours (albendazole sulfoxide)
Protein Binding
70%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Systemic availability, rate of absorption, and the elimination half-life of albendazole sulfoxide are increased in patients with extrahepatic obstruction.
Use: Labeled Indications
Hydatid disease: Treatment of cystic hydatid disease of the liver, lung, and peritoneum caused by the larval form of the dog tapeworm, Echinococcus granulosus.
Neurocysticercosis, parenchymal: Treatment of parenchymal neurocysticercosis due to active lesions caused by larval forms of the pork tapeworm, Taenia solium.
Use: Off Label
Microsporidiosis in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, albendazole is an effective and recommended agent in the management of intestinal or disseminated microsporidiosis (caused by microsporidia other than Enterocytozoon bieneusi and Vittaforma corneae) and for disseminated microsporidiosis (caused by Trachipleistophora or Anncaliia) in adolescent and adult HIV-infected patients.
Additional off-label uses:
Albendazole has activity against Ascaris lumbricoides (roundworm); Ancylostoma caninum; Ancylostoma duodenale and Necator americanus (hookworms); Cutaneous larva migrans; Enterobius vermicularis (pinworm); Giardia duodenalis (giardiasis); Gnathostoma spinigerum; Gongylonema sp; Mansonella perstans (filariasis); Oesophagostomum bifurcum; Opisthorchis sinensis (liver fluke); Trichinella spiralis (Trichinellosis); visceral larva migrans (toxocariasis); liver fluke Clonorchis sinensis; Giardia lamblia; Echinococcus multilocularis
Microsporidiosis (not limited to HIV-infected patients): Disseminated microsporidiosis (E. hellem, E. cuniculi, E. intestinalis, Pleistophora sp, Trachipleistophora sp, Brachiola vesicularum); Intestinal microsporidiosis (Encephalitozoon intestinalis); Ocular microsporidiosis (E. hellem, E. cuniculi, Vittaforma corneae)
Contraindications
Hypersensitivity to albendazole, benzimidazoles, or any component of the formulation
Dosage and Administration
Dosing: Adult
Neurocysticercosis, parenchymal: Oral:
Manufacturer’s labeling:
<60 kg: 15 mg/kg/day in 2 divided doses (maximum: 800 mg/day) for 8 to 30 days
≥60 kg: 800 mg/day in 2 divided doses for 8 to 30 days
Alternate recommendations (off-label dose): 15 mg/kg/day in 2 divided doses (maximum: 1200 mg/day) for 10 to 14 days; may be repeated if persistent viable lesions on 6-month follow-up imaging. Note: Concomitant therapy with praziquantel is recommended if >2 viable cysts present (Garcia 2014; IDSA/ASTMH [White 2018]). Initiate adjunctive corticosteroid therapy prior to initiation of albendazole. Antiparasitic therapy should not be initiated in patients with untreated hydrocephalus, calcified lesions, or cysticercal encephalitis; consult an infectious diseases specialist for specific treatment recommendations (IDSA/ASTMH [White 2018]).
Hydatid: Oral:
<60 kg: 15 mg/kg/day in 2 divided doses (maximum: 800 mg/day)
≥60 kg: 800 mg/day in 2 divided doses
Note: Administer dose for three 28-day cycles with a 14-day drug-free interval in between each cycle.
Ancylostoma caninum, Ascaris lumbricoides (roundworm), Ancylostoma duodenale (hookworm), and Necator americanus (hookworm) (off-label use): Oral: 400 mg as a single dose (Parasitic Infections 2013)
Clonorchis sinensis (Chinese liver fluke) or Opisthorchis viverrini (Southeast Asian liver fluke) (off-label use): Oral: 10 mg/kg/day for 7 days (Parasitic Infections 2013)
Cutaneous larva migrans (off-label use): Oral: 400 mg once daily for 3 days (Parasitic Infections 2013)
Echinococcus granulosus (tapeworm) (off-label use): Oral: 15 mg/kg/day (maximum: 800 mg/day) in 2 divided doses for 1 to 6 months (Parasitic Infections 2013)
Enterobius vermicularis (pinworm) (off-label use): Oral: 400 mg as a single dose; repeat in 2 weeks (Parasitic Infections 2013)
Giardia duodenalis (giardiasis) (off-label use): Oral: 400 mg once daily for 5 days (Parasitic Infections 2013)
Gnathostoma spinigerum (off-label use): Oral: 800 mg/day in 2 divided doses for 21 days (Parasitic Infections 2013)
Gongylonemiasis (off-label use): Oral: 400 mg once daily for 3 days (Parasitic Infections 2013)
Microsporidiosis:
Immunocompetent patients:
Disseminated (off-label use): 800 mg/day in 2 divided doses (Parasitic Infections 2013)
Intestinal (E. intestinalis) (off-label use): 800 mg/day in 2 divided doses for 21 days (Parasitic Infections 2013)
Ocular (off-label use): 800 mg/day in 2 divided doses, in combination with topical fumagillin (Parasitic Infections 2013)
Immunocompromised (HIV-positive) patients
Disseminated or intestinal infection (other than Enterocytozoon bieneusi or V. corneae) (off-label use): 800 mg/day in 2 divided doses; continue until CD4 count >200 cells/mm3 for >6 months after initiation of antiretroviral therapy (DHHS [OI Adults 2015])
Ocular (off-label use): 800 mg/day in 2 divided doses, in combination with topical fumagillin; continue until resolution of ocular symptoms and until CD4 count >200 cells/mm3 for >6 months after initiation of antiretroviral therapy (DHHS [OI Adults 2015])
Oesophagostomum bifurcum (off-label use): Oral: 400 mg as a single dose (Ziem 2004)
Trichinella spiralis (Trichinellosis) (off-label use): Oral: 800 mg/day in 2 divided doses for 8 to 14 days plus corticosteroids for severe symptoms (Parasitic Infections 2013)
Visceral larva migrans (toxocariasis) (off-label use): Oral: 800 mg/day in 2 divided doses for 5 days (Parasitic Infections 2013)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Neurocysticercosis (Taenia solium, pork tapeworm): Children and Adolescents: Note: Patients should receive concurrent corticosteroid for the first week of albendazole therapy and anticonvulsant therapy as required.
<60 kg: Oral: 7.5 mg/kg/dose twice daily for 8 to 30 days; maximum dose: 400 mg/dose
≥60 kg: Oral: 400 mg twice daily for 8 to 30 days
Hydatid disease (Echinococcus granulosus, dog tapeworm): Children and Adolescents (WHO 2010):
<60 kg: Oral: 7.5 mg/kg/dose twice daily; maximum dose: 400 mg/dose; 28-day cycle followed by a 14-day albendazole-free interval, for a total of 3 cycles
≥60 kg: Oral: 400 mg twice daily; 28-day cycle followed by a 14-day albendazole-free interval, for a total of 3 cycles
Ancyclostoma caninum (Eosinophilic enterocolitis):Limited data available: Children and Adolescents: Oral: 400 mg as a single dose (Medical Letter [Parasitic infections 2013])
Ancylostoma duodenale or Necator americanus (hookworms):
Infants ≥3 months: Very limited data available: Oral: 200 mg as a single dose. Dosing based on two cases (patient #1: age: 12 weeks, weight: 4.2 kg; and patient #2: age: 8 months, weight: 5.8 kg) of exclusively breastfed infants who showed clinical improvement after single-dose albendazole therapy (Bhatia 2010)
Children ≤2 years: Limited data available: Oral: 200 mg as a single dose; may repeat in 3 weeks (WHO 2010)
Children >2 years and Adolescents: Limited data available: Oral: 400 mg as a single dose; may repeat in 3 weeks (CDC; Medical Letter [Parasitic infections 2013]; WHO 2010)
Ascariasis (intestinal roundworm): Limited data available:
Children ≤2 years: Oral: 200 mg as a single dose; may repeat in 3 weeks (WHO 2010)
Children >2 years and Adolescents: Oral: 400 mg as a single dose; may repeat in 3 weeks (CDC; Medical Letter [Parasitic infections 2013]; WHO 2010)
Baylisascaris procyonis (raccoon roundworm), postexposure prophylaxis and treatment: Limited data available: Children and Adolescents: Oral: Frequently reported dose: 40 mg/kg/day (range: 20 to 50 mg/kg/day) in a single or two divided doses or 400 mg twice daily. Initiate as soon as possible after potential exposure (ideally within 3 days) to prevent clinical disease in any child at risk (eg, ingestion of raccoon stool or contaminated soil). Duration for prophylaxis is at least 10 days. Reported treatment duration is usually 4 weeks (Gavin 2002; Graeff-Teixeira 2016; Hajek 2009; Murray 2004; Pai 2007; Park 2000; Peters 2012).
Capillariasis: Limited data available: Children and Adolescents: Oral: 400 mg once daily for at least 10 days (CDC; Medical Letter [Parasitic infections 2013]; Sawamura 1999)
Clonorchis sinensis (Chinese liver fluke): Limited data available: Children and Adolescents: Oral: 10 mg/kg/dose once daily for 7 days (CDC; Medical Letter [Parasitic infections 2013]
Cutaneous larva migrans (dog and cat hookworm):
Infants ≥8 months and Children ≤10 kg: Very limited data available: Oral: 200 mg once daily for 3 days. Dosing based on four cases (ages 8, 11, 12, and 13 months) of infants who showed clinical improvement after therapy. There was complete resolution of infection in two of these infants; one infant had initial improvement, then recurrence requiring a second course of therapy and eventually alternate therapy, and another infant had resolution of symptoms followed by appearance of a similar lesion at a different location 3 months later, received a second course, and had rapid resolution of all symptoms (Black 2010).
Children weighing >10 kg and Adolescents: Limited data available: Oral: 400 mg once daily for 3 days (Medical Letter [Parasitic infections 2013]; WHO 2010); some patients may only need a single dose (WHO 2010)
Enterobiasis (pinworm): Limited data available:
Children ≤2 years: Oral: 200 mg as a single dose; may repeat in 3 weeks (WHO 2010)
Children >2 years and Adolescents: Oral: 400 mg as a single dose; may repeat in 2 to 3 weeks (Medical Letter [Parasitic infections 2013]; WHO 2010)
Filariasis (Wuchereria Bancroft);microfilaria, reduction or suppression or community eradication programs: Limited data available. Administer in combination with either ivermectin or diethylcarbamazine. Note: Does not kill all the adult worms (Medical Letter [Parasitic infections 2013]; WHO 2010).
Children ≤10 kg: Oral: 200 mg once annually for 5 years
Children >10 kg and Adolescents: Oral: 400 mg once annually for 5 years
Giardiasis (Giardia duodenalis): Limited data available: Children ≥2 years and Adolescents: Oral: 10 mg/kg/day once daily for 5 days; maximum dose: 400 mg/dose or 400 mg once daily for 5 days (Escobedo 2016, Medical Letter [Parasitic infections 2013]; Yereli 2004)
Microsporidia infection (except Enterocytozoon sp. and V. corneae): Limited data available: Children and Adolescents: Oral: 7.5 mg/kg/dose twice daily; maximum dose: 400 mg/dose (HHS [pediatric 2016]; Medical Letter [Parasitic infections 2013]) in HIV-exposed/-positive, continue until resolution of signs and symptoms and sustained immune reconstitution (>6 months at CDC immunologic category 1 or 2) after ART initiation (HHS [pediatric 2016])
Strongyloidiasis (Strongyloides stercoralis): Limited data available:
Children ≤10 kg: Oral: 200 mg once daily for 3 days; may repeat course in 3 weeks (WHO 2010)
Children >10 kg and Adolescents:
CDC recommendations: Oral: 400 mg twice daily for 7 days (CDC)
WHO recommendations: Oral: 400 mg once daily for 3 days; may repeat course in 3 weeks (WHO 2010)
Trichinellosis (Trichinosis): Limited data available:
CDC recommendations: Children and Adolescents: Oral: 400 mg twice daily for 8 to 14 days (CDC; Medical Letter [Parasitic infections 2013])
WHO recommendations: Children >10 kg and Adolescents: Oral: 400 mg once daily for 8 to 14 days (WHO 2010)
Trichuriasis (whipworm): Limited data available: Children >2 years and Adolescents: Oral: 400 mg once daily for 3 days (Medical Letter [Parasitic infections 2013]; WHO 2010); mild cases may be treated with a single dose of 200 to 400 mg; may repeat course in 3 weeks (WHO 2010)
Toxocariasis (ocular larva migrans, visceral larva migrans): Limited data available:
CDC recommendations: Children and Adolescents: Oral: 400 mg twice daily for 5 days (CDC; Medical Letter [Parasitic infections 2013])
WHO recommendation: Children and Adolescents: Oral: 10 mg/kg/dose once daily for 5 days; maximum dose: 400 mg/dose (WHO 2010)
Administration
Oral: Administer with a high-fat meal if treating a systemic infection (to increase absorption). Administration on an empty stomach may be appropriate for treating an intraluminal infection with no systemic involvement (Lange 1988). If patients have difficulty swallowing, tablets may be crushed or chewed, then swallowed with a drink of water.
Storage
Store between 20°C and 25°C (68°F to 77°F)
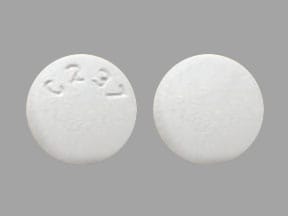
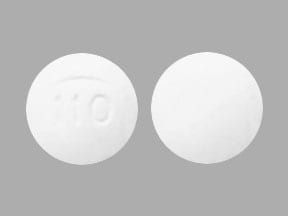
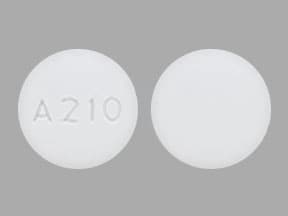
Albendazole Images
Drug Interactions
CarBAMazepine: May decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Grapefruit Juice: May increase serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
PHENobarbital: May decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Phenytoin: May decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Ritonavir: May decrease the serum concentration of Albendazole. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Headache (neurocysticercosis: 11%; hydatid: 1%)
Hepatic: Increased liver enzymes (hydatid: 16%; neurocysticercosis: <1%)
1% to 10%:
Central nervous system: Increased intracranial pressure (≤2%), dizziness (≤1%), vertigo (≤1%), meningism (1%)
Dermatologic: Alopecia (<1% to 2%)
Gastrointestinal: Abdominal pain (≤6%), nausea and vomiting (4% to 6%)
Miscellaneous: Fever (≤1%)
<1%, postmarketing, and/or case reports: Acute hepatic failure, acute renal failure, agranulocytosis, aplastic anemia, erythema multiforme, granulocytopenia, hepatitis, hypersensitivity reaction, leukopenia, neutropenia, pancytopenia, skin rash, Stevens-Johnson syndrome, thrombocytopenia, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Agranulocytosis, aplastic anemia, granulocytopenia, leukopenia, and pancytopenia have occurred leading to fatalities (rare); use with caution in patients with hepatic impairment (more susceptible to hematologic toxicity). Discontinue therapy in all patients who develop clinically significant decreases in blood cell counts.
- Transaminase elevations: Reversible elevations in hepatic enzymes have been reported. Patients with abnormal LFTs and hepatic echinococcosis are at an increased risk of hepatotoxicity. Discontinue therapy if LFT elevations are >2 times the upper limit of normal; may consider restarting treatment (with frequent monitoring of LFTs) when hepatic enzymes return to pretreatment values. Discontinue therapy if hepatic enzymes are significantly increased.
Disease-related concerns:
- Neurocysticercosis: Appropriate use: Antiparasitic therapy may worsen symptoms of neurocysticercosis by inducing an inflammatory response; adjunctive corticosteroid therapy should be started before initiation of albendazole. Antiparasitic therapy should not be initiated in patients with untreated hydrocephalus, calcified lesions, or cysticercal encephalitis. Perform funduscopic exam prior to initiation of antiparasitic therapy to exclude intraocular cysticerci; antiparasitic therapy may lead to blindness in some cases with unsuspected intraocular parasites (IDSA/ASTMH [White 2018]).
Monitoring Parameters
LFTs and CBC with differential at start of each 28-day cycle and every 2 weeks during therapy (more frequent monitoring for patients with liver disease); pregnancy test
Patients with neurocysticercosis: Ophthalmic exam for retinal lesions prior to therapy initiation; MRI every 6 months after completing therapy until resolution of cystic lesion (IDSA/ASTMH [White 2018])
Pregnancy
Pregnancy Considerations
Information following first trimester use of albendazole is limited (Gyorkos 2019). Most pregnancy outcome information is available from studies using a single dose of albendazole administered to women during the second or third trimester (Gyorkos 2019; Mofid 2017; Salam 2015). However, case reports are also available following longer term treatment of hydatid disease (Auer 1994; Bhattacharyya 2013; Pallua 2010).
Untreated soil-transmitted helminth infections during pregnancy are associated with adverse maternal outcomes (eg, maternal iron deficiency anemia, impaired nutrient absorption) (WHO 2017).
Use during the first trimester of pregnancy is not recommended (HHS [OI Adults]; IDSA/ASTMH [White 2018]; WHO 1996; WHO 2017). Pregnant patients with neurocysticercosis should be treated for symptoms (eg, increased intracranial pressure, seizures) the same as nonpregnant patients; however, antihelminthic therapy with albendazole can be deferred until after delivery (IDSA/ASTMH [White 2018]). Albendazole should not be used for the treatment of microsporidiosis in HIV-infected pregnant patients during the first trimester; use later in pregnancy may be considered when the benefits outweigh potential risks (HHS [OI Adults]; White 2018). The WHO also recommends treatment of soil-transmitted helminthiases (such as hookworm) in pregnant patients after the first trimester (WHO 1996). Pregnant women arriving as refugees from specific countries should not be given albendazole for the presumptive treatment of intestinal parasites prior to arrival in the United States (CDC 2019).
Evaluate pregnancy status prior to use in females of reproductive potential. Effective contraception is recommended during chronic therapy (Persichino 2018) and for 3 days after the last dose (per the manufacturer).
The WHO recommends preventive therapy with a benzimidazole, such as albendazole, in females of reproductive potential who live in areas where the baseline prevalence of soil-transmitted helminth infections is ≥20% (WHO 2017).
Patient Education
What is this drug used for?
- It is used to treat infections caused by worms.
Frequently reported side effects of this drug
- Headache
- Abdominal pain
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.