Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Extended Release 24 Hour, Oral, as hydrochloride:
Uroxatral: 10 mg [contains hydrogenated castor oil]
Generic: 10 mg
Pharmacology
Mechanism of Action
An antagonist of alpha1-adrenoreceptors in the lower urinary tract. Smooth muscle tone is mediated by the sympathetic nervous stimulation of alpha1-adrenoreceptors, which are abundant in the prostate, prostatic capsule, prostatic urethra, and bladder neck. Blockade of these adrenoreceptors can cause smooth muscles in the bladder neck and prostate to relax, resulting in an improvement in urine flow rate and a reduction in BPH symptoms.
Pharmacokinetics/Pharmacodynamics
Absorption
Decreased 50% under fasting conditions
Distribution
Vd: 3.2 L/kg
Metabolism
Hepatic, primarily via CYP3A4; metabolism includes oxidation, O-demethylation, and N-dealkylation; forms metabolites (inactive)
Excretion
Feces (69%); urine (24%; 11% as unchanged drug)
Time to Peak
Plasma: 8 hours following a meal
Half-Life Elimination
10 hours
Protein Binding
82% to 90%
Use in Specific Populations
Special Populations: Renal Function Impairment
Mean Cmax and AUC values were increased ~50% in patients with mild, moderate, or severe renal impairment.
Special Populations: Hepatic Function Impairment
In patients with moderate or severe hepatic impairment, clearance is decreased and plasma concentrations are increased 3- to 4-fold.
Special Populations: Elderly
Plasma concentrations in patients ≥75 years were ~35% greater than in those <65 years.
Use: Labeled Indications
Benign prostatic hyperplasia: Treatment of signs and symptoms of benign prostatic hyperplasia (BPH)
Use: Off Label
Facilitation of expulsion of ureteral stonesb
Data from two randomized unblinded active-controlled studies and one randomized placebo-controlled study in patients with symptomatic, uncomplicated distal ureteral stones ≤1 cm size supports the use of alfuzosin in the facilitation of ureteral stone expulsion Agrawal 2009, Ahmed 2010, Gurbuz 2011. Additional trials may be necessary to further define the role of alfuzosin in the management of distal ureteral stones.
Contraindications
Hypersensitivity to alfuzosin or any component of the formulation; moderate or severe hepatic impairment (Child-Pugh class B and C); concurrent use with potent CYP3A4 inhibitors (eg, itraconazole, ketoconazole, ritonavir)
Canadian labeling: Additional contraindications (not in US labeling): Concurrent use with other alpha1-blockers
Dosage and Administration
Dosing: Adult
Benign prostatic hyperplasia (BPH): Oral: 10 mg once daily
Ureteral stones, expulsion (off-label use): Oral: 10 mg once daily, discontinue after successful expulsion (average time to expulsion 1-2 weeks) (Agrawal, 2009; Ahmed, 2010; Gurbuz, 2011). Note: Patients with stones >10 mm were excluded from studies.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer immediately following a meal at the same time each day. Swallow tablet whole; do not crush or chew.
Dietary Considerations
Take immediately following a meal.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
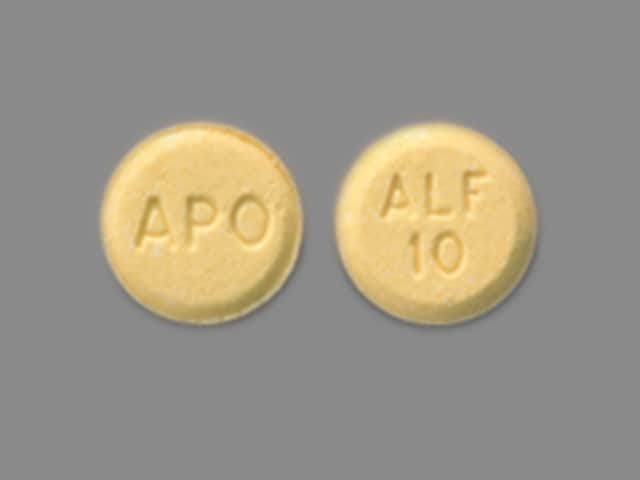
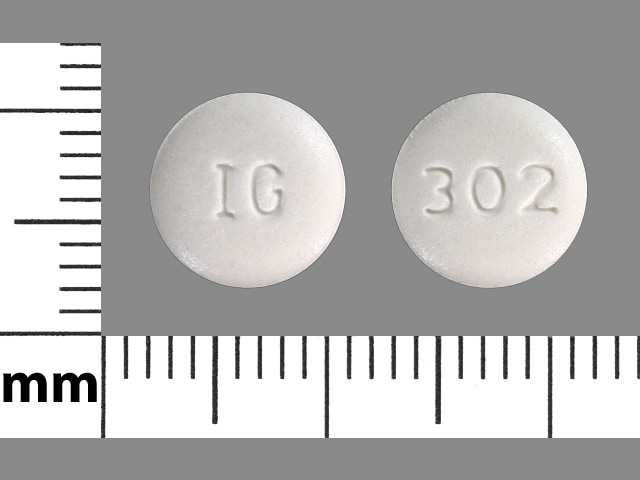
Alfuzosin Images
Drug Interactions
Alpha-/Beta-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Agonists: Alpha1-Blockers may diminish the vasoconstricting effect of Alpha1-Agonists. Similarly, Alpha1-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
Alpha1-Blockers: May enhance the antihypertensive effect of other Alpha1-Blockers. Avoid combination
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Beta-Blockers: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Blood Pressure Lowering Agents: Alfuzosin may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Alfuzosin. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Alpha1-Blockers. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nitroglycerin: Alfuzosin may enhance the hypotensive effect of Nitroglycerin. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Phosphodiesterase 5 Inhibitors: Alpha1-Blockers (Uroselective) may enhance the hypotensive effect of Phosphodiesterase 5 Inhibitors. Monitor therapy
Protease Inhibitors: May increase the serum concentration of Alfuzosin. Avoid combination
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Rilmenidine: Alpha1-Blockers may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
1% to 10%:
Central nervous system: Dizziness (6%), fatigue (3%), headache (3%), pain (1% to 2%)
Gastrointestinal: Abdominal pain (1% to 2%), constipation (1% to 2%), dyspepsia (1% to 2%), nausea (1% to 2%)
Genitourinary: Impotence (1% to 2%)
Respiratory: Upper respiratory tract infection (3%), bronchitis (1% to 2%), pharyngitis (1% to 2%), sinusitis (1% to 2%)
<1%, postmarketing, and/or case reports: Angina pectoris (pre-existing CAD), angioedema, atrial fibrillation, chest pain, diarrhea, edema, flushing, hepatic injury (including cholestatic), hypotension, intraoperative floppy iris syndrome (with cataract surgery), jaundice, orthostatic hypotension, priapism, pruritus, rhinitis, skin rash, syncope, systolic hypotension, tachycardia, thrombocytopenia, toxic epidermal necrolysis, urticaria, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Angina: Discontinue if symptoms of angina occur or worsen.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Floppy iris syndrome: Intraoperative floppy iris syndrome has been observed in cataract surgery patients who were on or were previously treated with alpha1-blockers; there appears to be no benefit in discontinuing alpha1-blocker therapy prior to surgery. May require modifications to surgical technique.
- Orthostatic hypotension/syncope: May cause orthostatic hypotension and syncope within a few hours following administration; anticipate a similar effect if therapy is interrupted for a few days, if dosage is rapidly increased, or if another antihypertensive drug, PDE-5 inhibitors, or nitrates is introduced. Use with caution in patients with symptomatic orthostatic hypotension.
- Priapism: Priapism has been associated with use (rarely); seek immediate medical assistance for erections lasting longer than 4 hours.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with histories of tachyarrhythmia or with certain cardiovascular conditions, such as myocardial ischemia.
- Hepatic impairment: Use with caution in patients with mild hepatic impairment; contraindicated in moderate-to-severe impairment.
- Prostate cancer: Rule out prostatic carcinoma before beginning therapy (many symptoms of BPH and prostate cancer are similar).
- QT prolongation: Alfuzosin has been shown to prolong the QT interval alone (minimal) and with other drugs with comparable effects on the QT interval (additive). Use with caution in patients with known QT prolongation (congenital or acquired).
- Renal impairment: Use with caution in patients with severe renal impairment (CrCl <30 mL/minute).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warning/precautions:
- Limitation of use: Not intended for use as an antihypertensive drug.
Monitoring Parameters
Urine flow, blood pressure, PSA
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- In men, it is used to treat the signs of an enlarged prostate.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Chest pain
- Erection that lasts more than 4 hours
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.