Boxed Warning
Life-threatening arrhythmias (tablet):
Amiodarone is intended for use only in patients with indicated life-threatening arrhythmias because its use is accompanied by substantial toxicity.
Pulmonary toxicity (tablet):
Amiodarone can cause pulmonary toxicity (hypersensitivity pneumonitis or interstitial/alveolar pneumonitis) that has resulted in clinically manifest disease at rates as high as 17% in some series of patients. Pulmonary toxicity has been fatal about 10% of the time. Obtain a baseline chest X-ray and pulmonary function tests, including diffusion capacity, when amiodarone therapy is initiated. Repeat history, physical exam, and chest X-ray every 3 to 6 months.
Hepatotoxicity:
Amiodarone can cause hepatotoxicity, which can be fatal. Obtain baseline and periodic liver transaminases and discontinue or reduce dose if the increase exceeds 3 times normal or doubles in a patient with an elevated baseline. Discontinue amiodarone if the patient experiences signs or symptoms of clinical liver injury.
Worsened arrhythmia (tablet):
Amiodarone can exacerbate arrhythmias. Initiate amiodarone in a clinical setting where continuous ECGs and cardiac resuscitation are available.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous, as hydrochloride:
Nexterone: 150 mg/100 mL in Dextrose (100 mL); 360 mg/200 mL in Dextrose (200 mL)
Generic: 150 mg/3 mL (3 mL); 450 mg/9 mL (9 mL); 900 mg/18 mL (18 mL)
Tablet, Oral, as hydrochloride:
Pacerone: 100 mg
Pacerone: 200 mg [scored; contains fd&c red #40, fd&c yellow #6 (sunset yellow)]
Pacerone: 400 mg [scored; contains fd&c yellow #10 aluminum lake]
Generic: 100 mg, 200 mg, 400 mg
Pharmacology
Mechanism of Action
Class III antiarrhythmic agent which inhibits adrenergic stimulation (alpha- and beta-blocking properties), affects sodium, potassium, and calcium channels, prolongs the action potential and refractory period in myocardial tissue; decreases AV conduction and sinus node function
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Slow and variable
Distribution
IV: Rapid redistribution with a decrease to 10% of peak values within 30 to 45 minutes after completion of infusion
IV single dose: Vdss: Mean range: 40 to 84 L/kg
Oral: Vd: 66 L/kg (range: 18 to 148 L/kg)
Metabolism
Hepatic via CYP2C8 and 3A4 to active N-desethylamiodarone metabolite; possible enterohepatic recirculation
Excretion
Feces; urine (<1% as unchanged drug)
Onset of Action
Oral: 2 days to 3 weeks; IV: (electrophysiologic effects) within hours; antiarrhythmic effects: 2 to 3 days to 1 to 3 weeks; mean onset of effect may be shorter in children vs adults and in patients receiving IV loading doses; Peak effect: 1 week to 5 months
Time to Peak
Oral: Serum: 3 to 7 hours
Duration of Action
After discontinuing therapy: Variable, 2 weeks to months: Children: Less than a few weeks; Adults: Several months
Note: Duration after discontinuation may be shorter in children than adults
Half-Life Elimination
Note: Half-life is shortened in children vs adults
Amiodarone:
Single dose: 58 days (range: 15 to 142 days)
Oral chronic therapy: Mean range: 40 to 55 days (range: 26 to 107 days)
IV single dose: Mean range: 9 to 36 days
N-desethylamiodarone (active metabolite): Prolonged in severe left ventricular dysfunction
Single dose: 36 days (range: 14 to 75 days)
Oral chronic therapy: 61 days
IV single dose: Mean range: 9 to 30 days
Protein Binding
>96%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
After a single dose of amiodarone injection in cirrhotic patients, Cmax was significantly lower and average concentration values were seen for desethylamiodarone, but mean amiodarone levels were unchanged.
Special Populations: Elderly
Clearance is lower and half-life is increased.
Use: Labeled Indications
Ventricular arrhythmias: Management of life-threatening recurrent ventricular fibrillation (VF) or recurrent hemodynamically unstable ventricular tachycardia (VT) refractory to other antiarrhythmic agents or in patients intolerant of other agents used for these conditions
Use: Off Label
Atrial fibrillationyes
Based on the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with atrial fibrillation (AF), the use of amiodarone for rate or rhythm control of AF is an effective and recommended treatment option. Due to its adverse effect profile, amiodarone should be reserved for patients in whom other therapies (eg, beta-blockers or nondihydropyridine calcium antagonists) are unsuccessful or contraindicated.
Electrical storm and incessant ventricular tachycardia, hemodynamically stableyes
Based on the AHA/ACC/HRS guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, amiodarone is an effective option in the management of electrical storm and incessant ventricular tachycardia (VT).
Nonsustained ventricular tachycardia, symptomaticyes
Based on the AHA/ACC/HRS guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death and the European Heart Rhythm Association/Heart Rhythm Society/Asia Pacific Heart Rhythm Society expert consensus on ventricular arrhythmias, amiodarone is a treatment option for symptomatic, nonsustained VT. A beta-blocker or nondihydropyridine calcium channel blocker (eg, diltiazem) is recommended prior to starting antiarrhythmic agents for this use.
Pharmacologic conversion of atrial fibrillation to and maintenance of normal sinus rhythmyes
Based on the 2014 AHA/ACC/HRS guideline for the management of patients with AF, the use of amiodarone for pharmacologic conversion of AF to and maintenance of normal sinus rhythm is effective and recommended for this condition.
Prevention of implantable cardioverter defibrillator shocksb
Data from a small double-blind, placebo-controlled, randomized trial and data from a prospective observational trial support the use of amiodarone for preventing implantable cardioverter defibrillator (ICD) shocks in patients who require these devices Connolly 2006, Steinberg 2001. Several meta-analyses also support amiodarone for this condition Ferreira-Gonzalez 2007, Ha 2012, Santangeli 2016.
Prevention of postoperative atrial fibrillation and atrial flutter associated with cardiothoracic surgeryyes
Based on the 2014 AHA/ACC/HRS guideline for the management of patients with AF and the American College of Cardiology Foundation (ACCF)/AHA guideline for coronary artery bypass graft surgery, the use of amiodarone for prevention of postoperative AF associated with cardiothoracic surgery in patients for whom beta-blockers are contraindicated is effective and recommended for this condition. The American College of Chest Physicians has recommended that amiodarone should be considered in patients undergoing cardiac surgery when beta-blockers are contraindicated ACCP [Bradley 2005].
Primary prevention of sudden cardiac death due to ventricular arrhythmiasb
Data from a large meta-analysis Piccini 2009 and data from a large systematic review Claro 2015 support the use of amiodarone for prevention of sudden cardiac arrest due to ventricular arrhythmias, which may be beneficial to patients who are not eligible for or decline implantation of an ICD.
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia)yes
Based on the ACC/AHA/HRS guideline for the management of patients with supraventricular tachycardia, amiodarone may be considered in the ongoing management of symptomatic supraventricular tachycardia (atrioventricular nodal reentrant tachycardia or atrioventricular reentrant tachycardia) or in the acute or ongoing management of focal atrial tachycardia; however, safety risks limit its therapeutic use. In many cases, amiodarone is reserved for use in patients for whom other therapies have failed or are contraindicated (eg, patients with structural or ischemic heart disease).
Sustained monomorphic ventricular tachycardia, hemodynamically stableyes
Based on the AHA/ACC/HRS guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, amiodarone is effective for suppressing monomorphic VT.
Ventricular premature beats, symptomaticyes
Based on the AHA/ACC/HRS guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, amiodarone is effective for suppressing ventricular premature beats. Clinical experts recommend beta-blockers as first-line pharmacologic therapy due to a safer side effect profile Manolis 2019.
Contraindications
Hypersensitivity to amiodarone, iodine, or any component of the formulation; sick sinus syndrome, second- or third-degree atrioventricular block, bradycardia leading to syncope without a functioning pacemaker; cardiogenic shock
Note: The FDA-approved product labeling states amiodarone is contraindicated in patients with iodine hypersensitivity. This does not include most patients with allergic reactions to shellfish or contrast media, which are usually not due to iodine itself (Beall 2007; Brouse 2005; Lakshmanadoss 2012). However, exercise caution in patients with severe allergies to shellfish or contrast media (Brouse 2005).
Canadian labeling (oral formulation): Additional contraindications (not in US labeling): Evidence of hepatitis; pulmonary interstitial abnormalities; thyroid dysfunction
Dosage and Administration
Dosing: Adult
Supraventricular arrhythmias:
Note: Amiodarone is a preferred antiarrhythmic for patients with structural heart disease.
Atrial fibrillation:
Pharmacologic cardioversion (off-label use) (alternative agent):
Note: Although amiodarone may slow ventricular response, the use of amiodarone (both IV and oral) is not particularly effective for cardioversion of atrial fibrillation to normal sinus rhythm as compared to other antiarrhythmics (eg, flecainide). Various IV and oral regimens have been described and may be used clinically. The more common regimens utilized include:
IV: Initial: 150 mg over 10 minutes, then 1 mg/minute for 6 hours, then 0.5 mg/minute for 18 hours. Continue for a total load of up to 10 g; may finish load with oral dosing. Change to oral maintenance dose when clinically indicated (AHA/ACC/HRS [January 2014]).
Oral: 600 to 800 mg daily in divided doses for a total load of up to 10 g, then a maintenance dose of 200 mg once daily (AHA/ACC/HRS [January 2014]) or 400 mg every 8 to 24 hours for a total load of ~6 to 10 g, then a maintenance dose of 100 to 200 mg once daily (Giardina 2019). A maintenance dose of 100 mg once daily is commonly used, especially for elderly patients or patients with low body mass (Zimetbaum 2007). Note: May initiate loading regimen 2 to 6 weeks prior to direct current cardioversion to reduce the risk of recurrence (Giardina 2019).
Maintenance of sinus rhythm (off-label use): Oral: 400 to 600 mg daily in divided doses for 2 to 4 weeks, followed by a maintenance dose of 100 to 200 mg once daily (AHA/ACC/HRS [January 2014]). Some experts recommend 400 mg every 8 to 24 hours for a total load of ~6 to 10 g, then a maintenance dose of 100 to 200 mg once daily (Giardina 2019).
Prevention of postoperative atrial fibrillation and atrial flutter associated with cardiothoracic surgery (off-label use) (alternative agent): Note: Some experts recommend the use of beta-blockers instead of amiodarone; however, in patients who cannot receive beta-blockers, amiodarone may be used. A variety of regimens have been used in clinical trials, including oral and IV regimens:
IV:
Preoperative regimen: 150 mg once, followed by 0.4 mg/kg/hour (~0.5 mg/minute for a 70 kg patient) for 3 days prior to surgery and for 5 days postoperatively (Lee 2000).
Postoperative regimen: Starting at postoperative recovery: 1 g infused over 24 hours for 2 days (Guarnieri 1999).
IV followed by Oral:
Postoperative regimen: IV: Starting 6 hours postoperatively, 1,050 mg IV loading dose over 24 hours, followed by 400 mg orally 3 times daily on postop days 1 through 4 (White 2003).
Oral: 200 mg 3 times daily for 7 days prior to surgery, followed by 200 mg daily until hospital discharge (Daoud 1997).
Rate control (off-label use)(alternative agent):
IV: Initial: 300 mg over 1 hour, then 10 to 50 mg/hour over 24 hours followed by an oral maintenance dose (AHA/ACC/HRS [January 2014]). Some experts recommend 150 mg over at least 10 minutes, followed by 0.5 to 1 mg/minute; may administer repeat boluses of 150 mg IV over at least 10 minutes as needed (Giardina 2019). Mean daily doses >2.1 g/day have been associated with hypotension.
Oral: Note: Long-term oral maintenance therapy with amiodarone may be considered if other rate control options are ineffective or contraindicated.
Usual maintenance dose: 100 to 200 mg once daily (AHA/ACC/HRS [January 2014]).
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia) (off-label use): Note: Amiodarone is usually reserved for use when other therapies have failed or are contraindicated. In general, most patients do not require long-term treatment with antiarrhythmic therapy.
Pharmacologic cardioversion:
IV: 150 mg over 10 minutes, then 1 mg/minute for 6 hours, then 0.5 mg/minute for 18 hours or may change to oral dosing (ACC/AHA/HRS [Page 2015]).
Oral:
Loading dose: 400 to 600 mg daily in divided doses for 2 to 4 weeks; in an inpatient monitoring setting, loading doses up to 1.2 g daily in divided doses may be considered (ACC/AHA/HRS [Page 2015]). Some experts suggest a total oral load of ~6 to 10 g (Giardina 2019).
Maintenance dose: 100 to 200 mg daily (ACC/AHA/HRS [Page 2015]).
Ventricular arrhythmias:
Electrical storm and incessant ventricular tachycardia, hemodynamically stable (off-label use):
Initial dose: IV: 150 mg over 10 minutes (may repeat if necessary), followed by 1 mg/minute IV infusion for 6 hours, followed by 0.5 mg/minute for 18 additional hours or until switched to oral therapy. Note: Coadministration with a beta-blocker (eg, propranolol) is recommended (ACC/AHA/HRS [Al-Khatib 2018]; Chatzidou 2018; Passman 2018).
Maintenance dose: Oral: Initial: 400 mg every 8 to 12 hours for 1 to 2 weeks, followed by 200 to 400 mg once daily (ACC/AHA/HRS [Al-Khatib 2018]). Some experts suggest a total oral load of ~6 to 10 g (Giardina 2019). Also see Switching to oral amiodarone after IV administration.
Nonsustained ventricular tachycardia, symptomatic (off-label use): Note: Consider addition of a beta-blocker or nondihydropyridine calcium channel blocker (eg, diltiazem) before starting antiarrhythmic therapy (EHRA/HRS/APHRS [Pedersen 2014]).
Oral: Initial: 400 mg every 8 to 12 hours for 1 to 2 weeks, followed by 200 to 400 mg once daily (ACC/AHA/HRS [Al-Khatib 2018]). Some experts suggest a total oral load of ~6 to 10 g during the first 1 to 2 weeks of therapy (Giardina 2019). Other experts suggest a more gradual oral loading regimen of 200 mg twice daily for the first 4 weeks, followed by 200 mg once daily (Zimetbaum 2018).
Prevention of implantable cardioverter defibrillator shocks (off-label use): Note: Antiarrhythmic therapy for this indication has not been shown to reduce mortality, but may improve quality of life by reducing frequency of implantable cardioverter defibrillator (ICD) shocks. Amiodarone is the preferred antiarrhythmic for this use (Connolly 2006; Ferreira-González 2007; Ha 2012; Santangeli 2016; Steinberg 2001).
Oral: 400 mg twice daily for 2 weeks, followed by 400 mg once daily for 4 weeks, then 200 mg once daily in combination with a beta-blocker (Connolly 2006) or some experts recommend 400 mg every 8 to 24 hours for a total oral load of ~6 to 10 g, then 200 to 400 mg once daily (Giardina 2019).
Primary prevention of sudden cardiac death due to ventricular arrhythmias (off-label use): Note: Consider addition of a beta-blocker before starting antiarrhythmic therapy. For patients eligible for an ICD with left ventricular dysfunction, but who cannot or refuse to have ICD implantation, amiodarone can be utilized (Piccini 2009).
Oral: Initial: 400 mg every 8 to 24 hours for 1 to 2 weeks for a total load of ~6 to 10 g, then a maintenance dose of 200 to 400 mg once daily (Claro 2015; Giardina 2019).
Secondary prevention of sudden cardiac death due to ventricular arrhythmias (eg, ventricular fibrillation or hemodynamically unstable ventricular tachycardia): Note: ICD implantation is preferred over antiarrhythmic therapy. In patients who do not meet ICD implant criteria, have contraindications, or refuse ICD implantation, antiarrhythmics can be utilized. Beta-blockers are recommended prior to or at the time of antiarrhythmic therapy initiation (ACC/AHA/HRS [Al-Khatib 2018]; Exner 1999; Podrid 2019).
Oral: 400 mg every 8 to 12 hours for 1 to 2 weeks, then a maintenance dose of 200 to 400 mg once daily (ACC/AHA/HRS [Al-Khatib 2018]) or some experts suggest 400 mg every 8 to 24 hours for a total load of ~6 to 10 g, then 200 to 400 mg once daily (Giardina 2019).
Sudden cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia: Unresponsive to cardiopulmonary resuscitation, defibrillation, and epinephrine:
IV push, Intraosseous: Initial: 300 mg rapid bolus; if ventricular fibrillation or pulseless ventricular tachycardia continues after subsequent defibrillation attempt or reoccurs after initially achieving return of spontaneous circulation, administer supplemental dose of 150 mg (AHA [Field 2010]; AHA [Neumar 2010]). Note: In this setting, administering undiluted is preferred (Dager 2006; Hazinski 2015; Skrifvars 2004).
Upon return of spontaneous circulation: IV: 1 mg/minute for 6 hours, then 0.5 mg/minute for 18 hours or until switched to oral therapy (AHA [Neumar 2010]). For maintenance dosing, see Secondary Prevention of Sudden Cardiac Death due to Ventricular Arrhythmias. Also see Switching to Oral Amiodarone after IV Administration.
Note: If amiodarone was not given during resuscitation but return of spontaneous circulation is achieved, some experts recommend empiric antiarrhythmic therapy with amiodarone (Podrid 2019).
Sustained monomorphic ventricular tachycardia, hemodynamically stable (off-label use): IV: Initial: 150 mg over 10 minutes, then 1 mg/minute for 6 hours, followed by 0.5 mg/minute for at least 18 hours or until switched to oral therapy (see Switching to Oral Amiodarone after IV Administration).
Breakthrough hemodynamically stable ventricular tachycardia: IV: 150 mg over 10 minutes (mean daily doses >2.1 g/day have been associated with hypotension).
Maintenance regimen: Oral: 400 mg every 8 to 12 hours for 1 to 2 weeks, then a maintenance dose of 200 to 400 mg once daily (ACC/AHA/HRS [Al-Khatib 2018]). Some experts suggest 400 mg every 8 to 24 hours for a total oral load of ~6 to 10 g, then 200 to 400 mg once daily (Giardina 2019).
Ventricular premature beats, symptomatic (off-label use): Note: For patients who are refractory to beta-blocker or nondihydropyridine calcium channel blocker therapy (eg, diltiazem) and cannot take class Ic antiarrhythmic agents (Manolis 2020).
Oral: 400 mg every 8 to 12 hours for 1 to 2 weeks, then when adequate control is achieved, decrease to 200 to 400 mg once daily; use lowest effective dose to minimize adverse effects (ACC/AHA/HRS [Al-Khatib 2018]). Some experts recommend a total load of ~6 to 10 g, followed by a usual maintenance dose of 200 mg once daily, but sometimes as low as 100 mg once daily (Manolis 2020).
Switching to oral amiodarone after IV administration: Use the following as a guide:
<1-week IV infusion: 400 to 1,200 mg daily in divided doses until loading dose of ~6 to 10 g has been administered, then start maintenance dose of 200 to 400 mg once daily (depending on indication).
1- to 2-week IV infusion: 400 to 800 mg daily in divided doses until loading dose of ~6 to 10 g has been administered, then start maintenance dose of 200 to 400 mg once daily (depending on indication).
>2-week IV infusion: 200 to 400 mg once daily (depending on indication) (Giardina 2019).
Note: Conversion from IV to oral therapy has not been formally evaluated. Some experts recommend a 1- to 2-day overlap when converting from IV to oral therapy, especially when treating ventricular arrhythmias (Ganz 2018).
Switching to IV amiodarone after oral administration: During long-term amiodarone therapy (ie, ≥4 months), the mean plasma-elimination half-life of the active metabolite of amiodarone is ~61 days. Replacement therapy may not be necessary in such patients if oral therapy is discontinued for a period <2 weeks, because any reduction in serum amiodarone concentrations during this period may not be clinically significant.
Dosing: Geriatric
Refer to adult dosing. No specific guidelines available. Dose selection should be cautious, at low end of dosage range, and titration should be slower to evaluate response. Although not supported by clinical evidence, a maintenance dose of 100 mg daily is commonly used, especially for elderly patients or patients with low body mass (Zimetbaum 2007).
Dosing: Pediatric
Perfusing tachycardias: Infants, Children, and Adolescents: IV, Intraosseous: Loading dose: 5 mg/kg (maximum: 300 mg/dose) over 20 to 60 minutes; may repeat twice up to maximum total dose of 15 mg/kg during acute treatment (PALS [Kleinman 2010]).
Ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), shock-refractory: Infants, Children, and Adolescents: IV, Intraosseous: 5 mg/kg (maximum: 300 mg/dose) rapid bolus; may repeat twice up to a maximum total dose of 15 mg/kg during acute treatment (PALS [de Caen 2015]; PALS [Duff 2018]; PALS [Kleinman 2010]).
Tachyarrhythmia, including junctional ectopic tachycardia (JET), paroxysmal supraventricular tachycardia (PSVT): Limited data available: Infants, Children, and Adolescents:
Oral: Loading dose: 10 to 15 mg/kg/day in 1 to 2 divided doses/day for 4 to 14 days or until adequate control of arrhythmia or prominent adverse effects occur; dosage should then be reduced to 5 mg/kg/day given once daily for several weeks; if arrhythmia does not recur, reduce to lowest effective dosage possible; usual daily minimal dose: 2.5 mg/kg/day; maintenance doses may be given for 5 of 7 days/week.
Note: For infants, some have suggested BSA-directed dosing: Loading dose: 600 to 800 mg/1.73 m2/day in 1 to 2 divided doses (equivalent to 347 to 462 mg/m2/day); maintenance dose: 200 to 400 mg/1.73 m2/day once daily (equivalent to 116 to 231 mg/m2/day) (Bucknall 1986; Coumel 1980; Coumel 1983; Paul 1994).
Note: Prolongation of the corrected QT interval was more likely in infants <9 months of age who received higher loading doses (20 mg/kg/day vs 10 mg/kg/day in 2 divided doses) (n=50; mean age: 1 ± 1.5 months) (Etheridge 2001).
IV: Loading dose: 5 mg/kg (maximum: 300 mg/dose) given over 60 minutes; Note: Most studies used bolus infusion time of 60 minutes to avoid hypotension; may repeat initial loading dose to a maximum total initial load: 10 mg/kg; do not exceed total daily bolus of 15 mg/kg/day (Etheridge 2001; Figa 1994; Haas 2008; Raja 1994; Soult 1995).
Note: Dividing the 5 mg/kg loading dose into 1 mg/kg aliquots (each administered over 5 to 10 minutes) has been used; an additional 1 to 5 mg/kg loading dose was given in the same manner, if needed, after 30 minutes (Perry 1996).
Continuous IV infusion (if needed); Note: Reported dosing units for regimens are variable (mcg/kg/minute and mg/kg/day); use caution to ensure appropriate dose and dosing units are used; taper infusion as soon as clinically possible and switch to oral therapy if necessary.
Dosing based on mcg/kg/minute: Initial: 5 mcg/kg/minute; increase incrementally as clinically needed; usual required dose: 10 mcg/kg/minute; range: 5 to 15 mcg/kg/minute; maximum daily dose: 2200 mg/day (Figa 1994; Kovacikova 2009; Lane 2010).
Dosing based on mg/kg/day: Initial: 10 mg/kg/day; increase incrementally as clinically needed; range: 10 to 20 mg/kg/day; maximum daily dose: 2,200 mg/day (Lane 2010; Perry 1996; Raja 1994; Soult 1995).
Reconstitution
Injection must be diluted in D5W before continuous IV infusion use. Dilute to final concentration of 1 to 6 mg/mL. Premixed solutions are available.
Extemporaneously Prepared
5 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 5 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet and Ora-Plus or a 1:1 mixture of Ora-Sweet SF and Ora-Plus adjusted to a pH between 6-7 using a sodium bicarbonate solution (5 g/100 mL of distilled water). Crush five 200 mg tablets in a mortar and reduce to a fine powder. Add small portions of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 200 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 200 mL. Label “shake well” and “protect from light.” Stable for 42 days at room temperature or 91 days refrigerated (preferred) (Nahata 1999; Nahata 2014).
Nahata MC, Morosco RS, Hipple TF. Stability of amiodarone in extemporaneous oral suspensions prepared from commercially available vehicles. Journalof Pediatric Pharmacy Practice. 1999;4(4):186-189.Nahata MC and Pai VB. Pediatric Drug Formulations. 6th ed. Cincinnati, OH: Harvey Whitney Books Co; 2014.
Administration
Oral: Administer consistently with regard to meals. Take in divided doses with meals if GI upset occurs or if taking large daily dose (≥1,000 mg). If GI intolerance occurs with single-dose therapy, use twice daily dosing.
IV: For infusions >1 hour, use concentrations ≤2 mg/mL unless a central venous catheter is used; commercially-prepared premixed solutions in concentrations of 1.5 mg/mL and 1.8 mg/mL are available. Use only volumetric infusion pump; use of drop counting may lead to underdosage. Administer through an IV line located as centrally as possible. For peripheral infusions, an in-line filter has been recommended during administration to reduce the incidence of phlebitis (consult individual institutional policies and procedures). During pulseless VT/VF, administering undiluted is preferred (Dager 2006; Skrifvars 2004). The Handbook of Emergency Cardiovascular Care (Hazinski 2015) and the ACLS guidelines do not make any specific recommendations regarding dilution of amiodarone in this setting.
Adjust administration rate to urgency (give more slowly when perfusing arrhythmia present). Slow the infusion rate if hypotension or bradycardia develops. Infusions >2 hours must be administered in a non-PVC container (eg, glass or polyolefin). PVC tubing is recommended for administration regardless of infusion duration. Incompatible with heparin; flush with saline prior to and following infusion. Note: IV administration at lower flow rates (potentially associated with use in pediatrics) and higher concentrations than recommended may result in leaching of plasticizers (DEHP) from intravenous tubing. DEHP may adversely affect male reproductive tract development. Alternative means of dosing and administration (1 mg/kg aliquots) may need to be considered.
May be a vesicant; ensure proper needle or catheter placement prior to and during IV infusion. Avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave needle/cannula in place); gently aspirate extravasated solution (do NOT flush the line); initiate hyaluronidase antidote for refractory cases (Reynolds 2014); remove needle/cannula; apply dry warm compresses (Reynolds 2014); elevate extremity.
Hyaluronidase: Intradermal: Inject a total of 1 mL (15 units/mL) as 5 separate 0.2 mL injections (using a 25-gauge needle) into area of extravasation (Fox 2017).
Dietary Considerations
Take consistently with regard to meals. Amiodarone is a potential source of large amounts of inorganic iodine; ~3 mg of inorganic iodine per 100 mg of amiodarone is released into the systemic circulation. Recommended daily allowance for iodine in adults is 150 mcg.
Grapefruit juice is not recommended.
Storage
Tablets: Store at 20°C to 25°C (68°F to 77°F); protect from light.
Injection: Store undiluted vials and premixed solutions (Nexterone) at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from light during storage; protect from excessive heat. There is no need to protect solutions from light during administration. When vial contents are admixed in D5W to a final concentration of 1-6 mg/mL, amiodarone is stable for 24 hours in glass or polyolefin bottles and for 2 hours in polyvinyl chloride (PVC) bags; do not use evacuated glass containers as buffer may cause precipitation. Nexterone is available as premixed solutions. Although amiodarone adsorbs to PVC tubing, all clinical studies used PVC tubing and the recommended doses account for adsorption; in adults, PVC tubing is recommended. Discard any unused portions of premixed solutions.
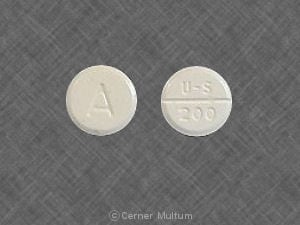
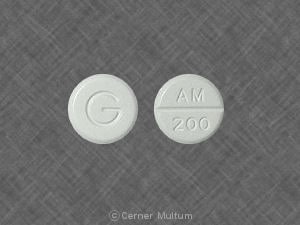
Amiodarone Images
Drug Interactions
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Agalsidase Alfa: Amiodarone may diminish the therapeutic effect of Agalsidase Alfa. Avoid combination
Agalsidase Beta: Amiodarone may diminish the therapeutic effect of Agalsidase Beta. Avoid combination
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP3A4 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Atazanavir: May increase the serum concentration of Amiodarone. Monitor therapy
AtorvaSTATin: Amiodarone may increase the serum concentration of AtorvaSTATin. Monitor therapy
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta-Blockers: Amiodarone may enhance the bradycardic effect of Beta-Blockers. Possibly to the point of cardiac arrest. Amiodarone may increase the serum concentration of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Bile Acid Sequestrants: May decrease the bioavailability of Amiodarone. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers (Nondihydropyridine): May enhance the bradycardic effect of Amiodarone. Sinus arrest has been reported. Monitor therapy
Cardiac Glycosides: Amiodarone may increase the serum concentration of Cardiac Glycosides. Management: Reduce the dose of cardiac glycosides by 30% to 50% or reduce the frequency of administration when initiating concomitant amiodarone therapy. Monitor for increased serum concentrations and toxic effects of cardiac glycosides. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Ceritinib: Amiodarone may enhance the bradycardic effect of Ceritinib. Amiodarone may enhance the QTc-prolonging effect of Ceritinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cimetidine: May increase the serum concentration of Amiodarone. Management: Consider alternatives to cimetidine. If this combination cannot be avoided, monitor for increased amiodarone concentrations/effects with cimetidine initiation/dose increase or decreased concentrations/effects with cimetidine discontinuation/dose decrease. Consider therapy modification
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Clopidogrel: Amiodarone may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Monitor therapy
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Cobicistat: May increase the serum concentration of Amiodarone. Monitor therapy
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Cyclophosphamide: May enhance the adverse/toxic effect of Amiodarone. Specifically, the risk of pulmonary toxicity may be enhanced. Monitor therapy
CycloSPORINE (Systemic): Amiodarone may increase the serum concentration of CycloSPORINE (Systemic). Management: Monitor for increased serum concentrations and/or toxicity of cyclosporine if combined with amiodarone. A reduction in cyclosporine dosage will likely be needed. Consider therapy modification
CYP2C8 Inhibitors (Strong): May increase the serum concentration of Amiodarone. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May enhance the bradycardic effect of Amiodarone. Avoid combination
Darunavir: May increase the serum concentration of Amiodarone. Monitor therapy
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Erythromycin (Systemic): Amiodarone may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of Amiodarone. Erythromycin (Systemic) may increase the serum concentration of Amiodarone. Avoid combination
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Etravirine: May decrease the serum concentration of Amiodarone. Monitor therapy
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of Amiodarone. Avoid combination
Flecainide: Amiodarone may enhance the QTc-prolonging effect of Flecainide. Amiodarone may increase the serum concentration of Flecainide. Management: Decrease flecainide dose by 50%. Monitor for QTc interval prolongation and ventricular arrhythmias, and consider monitoring for elevated flecainide concentrations. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Flibanserin: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Flibanserin. Monitor therapy
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Fosamprenavir: May increase the serum concentration of Amiodarone. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May enhance the QTc-prolonging effect of Amiodarone. Fosphenytoin may decrease the serum concentration of Amiodarone. Amiodarone may increase the serum concentration of Fosphenytoin. Management: Seek alternatives when possible. Monitor patients receiving this combination for QT interval prolongation or changes in cardiac rhythm, and for decreased serum concentrations/effects of amiodarone and increased concentrations/effects of phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gemifloxacin: May enhance the QTc-prolonging effect of Amiodarone. Avoid combination
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Grapefruit Juice: May decrease serum concentrations of the active metabolite(s) of Amiodarone. Grapefruit Juice may increase the serum concentration of Amiodarone. Avoid combination
Halofantrine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Haloperidol: Amiodarone may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Indinavir: May increase the serum concentration of Amiodarone. Avoid combination
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lacosamide: Antiarrhythmic Agents (Class III) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: May enhance the QTc-prolonging effect of QT-prolonging CYP3A4 Substrates. Management: Do not use lefamulin tablets with QT-prolonging CYP3A4 substrates. Lefamulin prescribing information lists this combination as contraindicated. Avoid combination
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of Amiodarone. Avoid combination
Lidocaine (Systemic): Amiodarone may increase the serum concentration of Lidocaine (Systemic). Monitor therapy
Lidocaine (Topical): May enhance the arrhythmogenic effect of Antiarrhythmic Agents (Class III). Antiarrhythmic Agents (Class III) may increase the serum concentration of Lidocaine (Topical). This mechanism specifically applies to amiodarone and dronedarone. Monitor therapy
Lofepramine: May enhance the arrhythmogenic effect of Amiodarone. Avoid combination
Lofexidine: May enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 30 mg/day. Consider therapy modification
Lopinavir: May enhance the QTc-prolonging effect of Amiodarone. Lopinavir may increase the serum concentration of Amiodarone. More specifically, Lopinavir/Ritonavir may increase the serum concentration of Amiodarone. Management: If this combination cannot be avoided, monitor for increased amiodarone serum concentrations and effects as well as for evidence of QT interval prolongation. Avoid combination
Loratadine: Amiodarone may increase the serum concentration of Loratadine. Management: Due to reported QT interval prolongation and Torsades de Pointes with this combination, consider an alternative to loratadine when possible. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lovastatin: Amiodarone may increase the serum concentration of Lovastatin. Management: Consider using a non-interacting statin (pravastatin, pitavastatin) in patients on amiodarone. If combined, limit the adult lovastatin dose to 40 mg daily and monitor for lovastatin toxicities (eg, myalgia, liver function test elevations, rhabdomyolysis). Consider therapy modification
Methadone: Amiodarone may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mipomersen: Amiodarone may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
Nelfinavir: May increase the serum concentration of Amiodarone. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ombitasvir, Paritaprevir, and Ritonavir: May increase the serum concentration of Amiodarone. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May increase the serum concentration of Amiodarone. Management: Canadian labeling recommends avoiding this combination. Monitor therapy
Ondansetron: Amiodarone may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Orlistat: May decrease the serum concentration of Amiodarone. Monitor therapy
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Phenytoin: May decrease the serum concentration of Amiodarone. Amiodarone may increase the serum concentration of Phenytoin. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Posaconazole: May increase the serum concentration of QT-prolonging CYP3A4 Substrates. Such increases may lead to a greater risk for proarrhythmic effects and other similar toxicities. Avoid combination
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Propafenone: Amiodarone may enhance the QTc-prolonging effect of Propafenone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): May enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of Amiodarone. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Erythromycin (Systemic); Nilotinib; Ribociclib. Consider therapy modification
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Ranolazine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ranolazine. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Red Yeast Rice: Amiodarone may increase the serum concentration of Red Yeast Rice. Management: Consider using a non-interacting statin (eg, pravastatin, pitavastatin) in patients on amiodarone. If combined, limit the adult red yeast rice dose to the equivalent of lovastatin 40 mg daily and monitor for toxicities (eg, myalgia, rhabdomyolysis). Consider therapy modification
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
RifAMPin: May decrease serum concentrations of the active metabolite(s) of Amiodarone. Specifically, desethylamiodarone concentrations may decrease. RifAMPin may decrease the serum concentration of Amiodarone. Monitor therapy
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ritonavir: May increase the serum concentration of Amiodarone. Management: Ritonavir US prescribing information lists this combination as contraindicated. Amiodarone use should be avoided with lopinavir/ritonavir, but if the combination must be used, monitor closely for increased amiodarone serum concentrations and effects. Avoid combination
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Saquinavir: May enhance the QTc-prolonging effect of Amiodarone. Saquinavir may increase the serum concentration of Amiodarone. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Simvastatin: Amiodarone may increase the serum concentration of Simvastatin. Management: Consider using a non-interacting statin (pravastatin) in patients on amiodarone. If combined, limit the adult simvastatin dose to 20 mg daily and monitor for evidence of simvastatin toxicities (eg, myalgia, liver function test elevations, rhabdomyolysis). Consider therapy modification
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sodium Iodide I131: Amiodarone may diminish the therapeutic effect of Sodium Iodide I131. Consider therapy modification
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sofosbuvir: May enhance the bradycardic effect of Amiodarone. Avoid combination
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): May enhance the QTc-prolonging effect of Amiodarone. Amiodarone may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Talazoparib: Amiodarone may increase the serum concentration of Talazoparib. Management: If concurrent use cannot be avoided, reduce talazoparib dose to 0.75 mg once daily. After a period of 3 to 5 times the half-life of amiodarone, increase the talazoparib dose to the dose used before initiation of amiodarone. Consider therapy modification
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Thyroid Products: Amiodarone may diminish the therapeutic effect of Thyroid Products. Monitor therapy
Tipranavir: May increase the serum concentration of Amiodarone. Avoid combination
TiZANidine: Amiodarone may increase the serum concentration of TiZANidine. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): Amiodarone may enhance the anticoagulant effect of Vitamin K Antagonists. Amiodarone may increase the serum concentration of Vitamin K Antagonists. Management: Monitor patients extra closely for evidence of increased anticoagulant effects if amiodarone is started. Consider empiric reduction of 30% to 50% in warfarin dose, though no specific guidelines on dose adjustment have been published. Consider therapy modification
Voriconazole: Amiodarone may enhance the QTc-prolonging effect of Voriconazole. Voriconazole may increase the serum concentration of Amiodarone. Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Hypotension (intravenous: 20%; oral: <1%; refractory in rare cases)
Endocrine & metabolic: Phospholipidemia (pulmonary phospholipidosis; oral: 50%; intravenous: <1%)
Gastrointestinal: Nausea (oral: 10% to 33%; intravenous: 4%), vomiting (10% to 33%; intravenous: <2%)
Ophthalmic: Epithelial keratopathy (98% to 99%; vortex; Raizman 2016)
Respiratory: Pulmonary toxicity (oral: 2% to 17%; intravenous: <1%)
1% to 10%:
Cardiovascular: Bradycardia (2% to 6%), atrioventricular block (≤5%), sinus bradycardia (≤5%), exacerbation of cardiac arrhythmia (oral: 2% to 5%), cardiac failure (2% to 3%), cardiac arrhythmia (1% to 3%), edema (oral: 1% to 3%; intravenous: <1%), flushing (oral: 1% to 3% intravenous: <1%), sinus node dysfunction (≤3%), ventricular tachycardia (2%), atrial fibrillation (intravenous: <2%), cardiogenic shock (intravenous: <2%), nodal arrhythmia (intravenous: <2%), prolonged Q-T interval on ECG (<2%; associated with worsening arrhythmia), torsades de pointes (<2%), ventricular fibrillation (<2%)
Dermatologic: Skin photosensitivity (10%), solar dermatitis (oral: ≤9%), Stevens-Johnson syndrome (<2%)
Endocrine & metabolic: Hypothyroidism (1% to 10%), decreased libido (oral: 1% to 3%), hyperthyroidism (2%)
Gastrointestinal: Anorexia (oral: 4% to 9%), constipation (oral: 4% to 9%), altered salivation (oral: 1% to 3%), dysgeusia (oral: 1% to 3%), abdominal pain (oral: 1% to 3%), diarrhea (intravenous: <2%)
Hematologic & oncologic: Disorder of hemostatic components of blood (oral: 1% to 3%), thrombocytopenia (<2%)
Hepatic: Abnormal hepatic function tests (4%), hepatic disease (oral: 1% to 3%), increased serum alanine aminotransferase (<2%), increased serum aspartate aminotransferase (<2%)
Nervous system: Abnormal gait (oral: ≤9%), ataxia (oral: ≤9%), fatigue (oral: ≤9%), involuntary body movements (oral: ≤9%), malaise (oral: ≤9%), dizziness (oral: 4% to 9%; intravenous: <1%), paresthesia (oral: 4% to 9%), altered sense of smell (oral: 1% to 3%), headache (oral: 1% to 3%), insomnia (oral: 1% to 3%), sleep disorder (oral: 1% to 3%)
Neuromuscular & skeletal: Tremor (oral: ≤9%)
Ophthalmic: Blurred vision (oral: ≤10%; intravenous: <1%), visual halos around lights (oral: ≤10%), visual disturbance (oral: 4% to 9%), optic neuritis (1%)
Renal: Renal insufficiency (<2%)
Respiratory: Pneumonitis (oral: ≤9%), pulmonary fibrosis (oral: ≤9%; intravenous: <1%), acute respiratory distress syndrome (≤2%), pulmonary edema (intravenous: <2%)
Miscellaneous: Fever (intravenous: 3%; oral: <1%)
Frequency not defined:
Cardiovascular: Asystole
Nervous system: Peripheral neuropathy
Ophthalmic: Dry eye syndrome, photophobia
Respiratory: Hypersensitivity pneumonitis, pneumonitis (alveolar)
<1%, postmarketing, and/or case reports: Acute pancreatitis, acute renal failure, agranulocytosis, alopecia, anaphylactic shock, anaphylaxis, angioedema, aplastic anemia, back pain, blue-gray skin pigmentation, bronchiolitis obliterans organizing pneumonia, bronchospasm, bullous dermatitis, cardiac conduction disturbance (including bundle branch block, infra-HIS block, and antegrade conduction via an accessory pathway), cholestasis, cholestatic hepatitis, confusion, cough, delirium, demyelinating disease (polyneuropathy), disorientation, drug-induced Parkinson's disease, drug reaction with eosinophilia and systemic symptoms, dyspnea, eczema, eosinophilic pneumonitis, epididymitis, erythema multiforme, exfoliative dermatitis, granulocytosis, hallucination, hemolytic anemia, hemoptysis, hepatic cirrhosis, hepatic failure, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), hypoesthesia, hypoxia, idiopathic intracranial hypertension, impotence, increased intracranial pressure, increased lactate dehydrogenase, increased serum alkaline phosphatase, increased serum creatinine, infusion site reaction (including cellulitis, edema, erythema, extravasation possibly leading to venous/infusion site necrosis, granuloma, hypoesthesia, induration, inflammation, intravascular amiodarone deposition/mass, pain, phlebitis, pigment changes, pruritus, skin sloughing, thrombophlebitis, thrombosis, urticaria), interstitial pneumonitis, intracranial hypertension (Tan 2019), jaundice, lupus-like syndrome, malignant neoplasm of skin, malignant neoplasm of thyroid, mass (pulmonary), muscle spasm, myasthenia, myopathy, myxedema (including myxedema coma), neutropenia, nonimmune anaphylaxis, optic neuropathy, pancytopenia, pleural effusion, pleurisy, pruritus, pulmonary alveolar hemorrhage, pulmonary infiltrates, respiratory failure, rhabdomyolysis, SIADH, sinoatrial arrest, skin carcinoma, skin granuloma, skin rash, spontaneous ecchymoses, thyroid nodule, thyrotoxicosis, toxic epidermal necrolysis, urticaria, vasculitis, ventricular premature contractions, visual field defect, wheezing, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Bradycardia/hypotension: May cause hypotension, which may be refractory and fatal, and bradycardia (infusion-rate related). Hypotension with rapid administration has been attributed to the emulsifier polysorbate 80. Commercially-prepared premixed solutions do not contain polysorbate 80 and may have a lower incidence of hypotension.
- Dermatologic toxicity: May cause life-threatening or fatal cutaneous reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis (TEN). If symptoms or signs (eg, progressive skin rash often with blisters or mucosal lesions) occur, immediately discontinue.
- Extravasation: May be a vesicant; ensure proper needle or catheter placement prior to infusion. Avoid extravasation.
- Hepatotoxicity: [US Boxed Warning (tablet)]: Hepatotoxicity (may be fatal) can occur. Obtain baseline and periodic liver transaminases and discontinue or reduce dose if the increase exceeds 3 times normal or doubles in a patient with an elevated baseline. Discontinue treatment if the patient experiences signs or symptoms of clinical liver injury. Elevated bilirubin levels have been reported in patients administered IV amiodarone. Note: Although the US Boxed Warning pertains to the tablet prescribing information, these effects may also be seen with intravenous administration, depending on duration of use.
- Neurotoxicity: Peripheral neuropathy has been reported rarely with chronic administration; may resolve when amiodarone is discontinued, but resolution may be slow and incomplete.
- Ocular effects: Regular ophthalmic examination (including slit lamp and fundoscopy) is recommended. May cause optic neuropathy and/or optic neuritis resulting in visual impairment (peripheral vision loss, changes in acuity) at any time during therapy; permanent blindness has occurred. If symptoms of optic neuropathy and/or optic neuritis occur, prompt ophthalmic evaluation is recommended. If diagnosis of optic neuropathy and/or optic neuritis is confirmed, reevaluate amiodarone therapy. Corneal microdeposits occur in a majority of adults and may cause visual disturbances in up to 10% of patients (blurred vision, halos); asymptomatic microdeposits may be reversible and are not generally considered a reason to discontinue treatment. Corneal refractive laser surgery is generally contraindicated in amiodarone users (from manufacturers of surgical devices).
- Photosensitivity: Avoid excessive exposure to sunlight; may cause photosensitivity. During long-term treatment, a blue-gray discoloration of exposed skin may occur; risk increased in patients with fair complexion or excessive sun exposure; may be related to cumulative dose and duration of therapy.
- Proarrhythmic effects: [US Boxed Warning (tablet)]: Amiodarone can exacerbate arrhythmias; initiate therapy in a clinical setting where continuous ECGs and cardiac resuscitation are available; other types of arrhythmias have occurred, including significant heart block, sinus bradycardia, new ventricular fibrillation, incessant ventricular tachycardia, increased resistance to cardioversion, and polymorphic ventricular tachycardia associated with QTc prolongation (torsades de pointes). Risk may be increased with concomitant use of other antiarrhythmic agents or drugs that prolong the QTc interval. Proarrhythmic effects may be prolonged. Note: Although the US Boxed Warning pertains to the tablet prescribing information, these effects may also be seen with intravenous administration, depending on duration of use.
- Pulmonary toxicity: [US Boxed Warning (tablet)]: Pulmonary toxicity (hypersensitivity pneumonitis or interstitial/alveolar pneumonitis) has been reported (including fatalities). Prior to initiation, obtain a baseline chest X-ray and pulmonary function tests, including diffusion capacity. Repeat history, physical exam, and chest X-ray every 3 to 6 months. Alternative therapy should be considered if signs or symptoms of pulmonary toxicity occur. Note: Although the US Boxed Warning pertains to the tablet prescribing information, these effects may also be seen with intravenous administration, depending on duration of use.
- Thyroid effects: May cause hyper- or hypothyroidism; hyperthyroidism may result in thyrotoxicosis (including fatalities) and/or the possibility of arrhythmia breakthrough or aggravation. If any new signs of arrhythmia appear, consider the possibility of hyperthyroidism. Hypothyroidism (sometimes severe) may be primary or subsequent to resolution of preceding amiodarone-induced hyperthyroidism; myxedema (may be fatal) has been reported. If hyper- or hypothyroidism occurs, reduce dose or discontinue amiodarone. Thyroid nodules and/or thyroid cancer have also been reported. Use caution in patients with thyroid disease; thyroid function should be monitored prior to treatment and periodically thereafter, particularly in the elderly and in patients with underlying thyroid dysfunction.
Disease-related concerns:
- Arrhythmias: Appropriate use: [US Boxed Warnings (tablet)]: Only indicated for patients with life-threatening arrhythmias because of risk of substantial toxicity. Alternative therapies should be tried first before using amiodarone. Patients should be hospitalized when amiodarone is initiated. Currently, the 2015 ACLS guidelines recommend the consideration of IV amiodarone as the preferred antiarrhythmic for the treatment of pulseless VT/VF unresponsive to CPR, defibrillation, and vasopressor therapy (AHA [Link 2015]). In patients with non-life-threatening arrhythmias (eg, atrial fibrillation), amiodarone should be used only if the use of other antiarrhythmics has proven ineffective or are contraindicated. Note: Although the US Boxed Warning pertains to the tablet prescribing information, these effects may also be seen with intravenous administration depending on duration of use.
- Cardiac devices (eg, implanted defibrillators, pacemakers): Chronic administration of antiarrhythmic drugs may affect defibrillation or pacing thresholds. Assess when initiating amiodarone and during therapy.
- Electrolyte imbalance: Correct electrolyte disturbances, especially hypokalemia, hypomagnesemia, or hypocalcemia, prior to use and throughout therapy.
- Myocardial infarction: In the setting of acute myocardial infarction, beta-blocker therapy should still be initiated even though concomitant amiodarone therapy provides beta-blockade.
- Wolff-Parkinson-White (WPW) syndrome: Amiodarone should not be used in patients with WPW syndrome and preexcited atrial fibrillation/flutter since ventricular fibrillation may result (AHA/ACC/HRS [January 2014]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Drugs metabolized by CYP enzymes: Amiodarone is a potent inhibitor of CYP enzymes and transport proteins (including p-glycoprotein), which may lead to increased serum concentrations/toxicity of a number of medications.
- Drugs with QT prolongation potential: Particular caution must be used when a drug with QTc-prolonging potential relies on metabolism via enzymes amiodarone inhibits, since the effect of elevated concentrations may be additive with the effect of amiodarone. Carefully assess risk:benefit of coadministration of other drugs which may prolong QTc interval.
- Warfarin: Use caution when initiating amiodarone in patients on warfarin. Cases of increased INR with or without bleeding have occurred in patients treated with warfarin; monitor INR closely after initiating amiodarone in these patients.
Special populations:
- Surgical patients: Use caution and close perioperative monitoring in surgical patients; may enhance myocardial depressant and conduction effects of halogenated inhalational anesthetics; adult respiratory distress syndrome (ARDS) has been reported postoperatively (fatal in rare cases). Hypotension upon discontinuation of cardiopulmonary bypass during open-heart surgery have been reported (rare); relationship to amiodarone is unknown.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity ("gasping syndrome") in neonates; the "gasping syndrome" consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Commercially-prepared premixed infusion: Contains the excipient cyclodextrin (sulfobutyl ether beta-cyclodextrin), which may accumulate in patients with renal insufficiency, although the clinical significance of this finding is uncertain (Luke 2010).
- Long-term use: There has been limited experience in patients receiving IV amiodarone for >3 weeks.
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- CAST trial: In the Cardiac Arrhythmia Suppression Trial (CAST), recent (>6 days but <2 years ago) myocardial infarction patients with asymptomatic, nonlife-threatening ventricular arrhythmias did not benefit and may have been harmed by attempts to suppress the arrhythmia with flecainide or encainide. An increased mortality or nonfatal cardiac arrest rate (7.7%) was seen in the active treatment group compared with patients in the placebo group (3%). The applicability of the CAST results to other populations is unknown. Use of amiodarone post-MI was not associated with an increase in mortality in two post-MI trials. Antiarrhythmic agents should be reserved for patients with life-threatening ventricular arrhythmias.
- Discontinuation of therapy: Patients may still be at risk for amiodarone-related adverse reactions or drug interactions after the drug has been discontinued. The pharmacokinetics are complex (due to prolonged duration of action and half-life) and difficult to predict.
Monitoring Parameters
Blood pressure, heart rate (ECG) and rhythm throughout therapy; assess patient for signs of lethargy, edema of the hands or feet, weight loss, and pulmonary toxicity (baseline pulmonary function tests and chest X-ray; continue monitoring chest X-ray annually during therapy); liver function tests (semiannually); monitor serum electrolytes, especially potassium and magnesium. Assess thyroid function tests before initiation of treatment and then periodically thereafter (some experts suggest every 3 to 6 months). If signs or symptoms of thyroid disease or arrhythmia breakthrough/exacerbation occur then immediate re-evaluation is necessary. Amiodarone partially inhibits the peripheral conversion of thyroxine (T4) to triiodothyronine (T3); serum T4 and reverse triiodothyronine (rT3) concentrations may be increased and serum T3 may be decreased; most patients remain clinically euthyroid, however, clinical hypothyroidism or hyperthyroidism may occur. Monitor infusion site.
Perform regular ophthalmic exams.
Patients with implantable cardiac devices: Monitor pacing or defibrillation thresholds with initiation of amiodarone and during treatment.
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Considerations
Amiodarone and the active metabolite, N-desethylamiodarone, cross the placenta (Plomp 1992).
In utero exposure may cause fetal harm. Reported risks include neonatal bradycardia, QT prolongation, and periodic ventricular extrasystoles; neonatal hypothyroidism (with or without goiter); neonatal hyperthyroxinemia; neurodevelopmental abnormalities independent of thyroid function; jerk nystagmus with synchronous head titubation; fetal growth retardation; and/or premature birth.
Oral or IV amiodarone should be used in pregnancy only to treat arrhythmias refractory to other treatments or when other treatments are contraindicated (ACC/AHA/HRS [Page 2015]).
Amiodarone (administered either maternally or directly to the fetus) may be considered for the in utero management of fetal atrial flutter and in life-threatening cases of sustained fetal supraventricular tachycardia refractory to first and second line agents, but because of potential toxicity, risks and benefits should be assessed (AHA [Donofrio 2014]; Kang 2015).
If in utero exposure occurs, newborns should be monitored for thyroid disorders and cardiac arrhythmias.
Patient Education
What is this drug used for?
- It is used to treat certain types of abnormal heartbeats.
Frequently reported side effects of this drug
- Constipation
- Nausea
- Vomiting
- Loss of strength and energy
- Abdominal pain
- Headache
- Trouble sleeping
- Flushing
- Change in taste
- Change in smell
- Increased saliva
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse
- Thyroid problems like change in weight without trying, anxiety, feeling restless, feeling very weak, hair thinning, depression, neck swelling, trouble focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Change in balance
- Tremors
- Trouble moving
- Rigidity
- Blue/gray skin discoloration
- Sunburn
- Coughing up blood
- Chest pain
- Burning or numbness feeling
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Vision changes
- Eye pain
- Severe eye irritation
- Sensitivity to light
- Dizziness
- Passing out
- Abnormal movements
- Muscle weakness
- Decreased sex drive
- Shortness of breath
- Excessive weight gain
- Swelling of arm or leg
- Bruising
- Bleeding
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.