Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
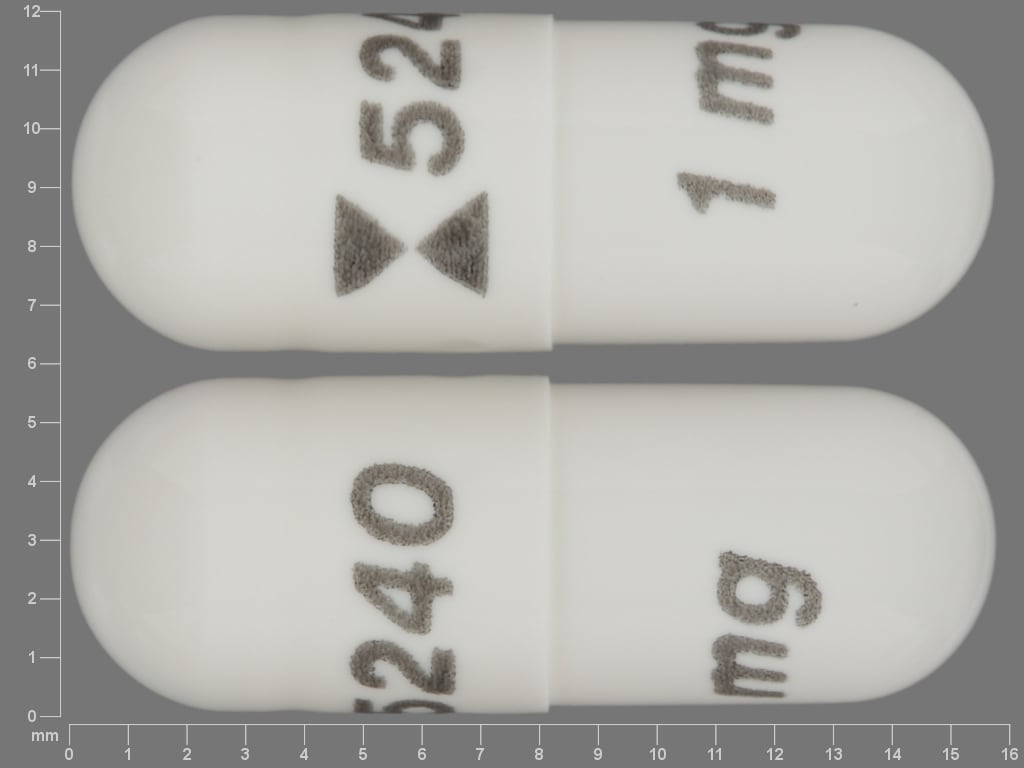
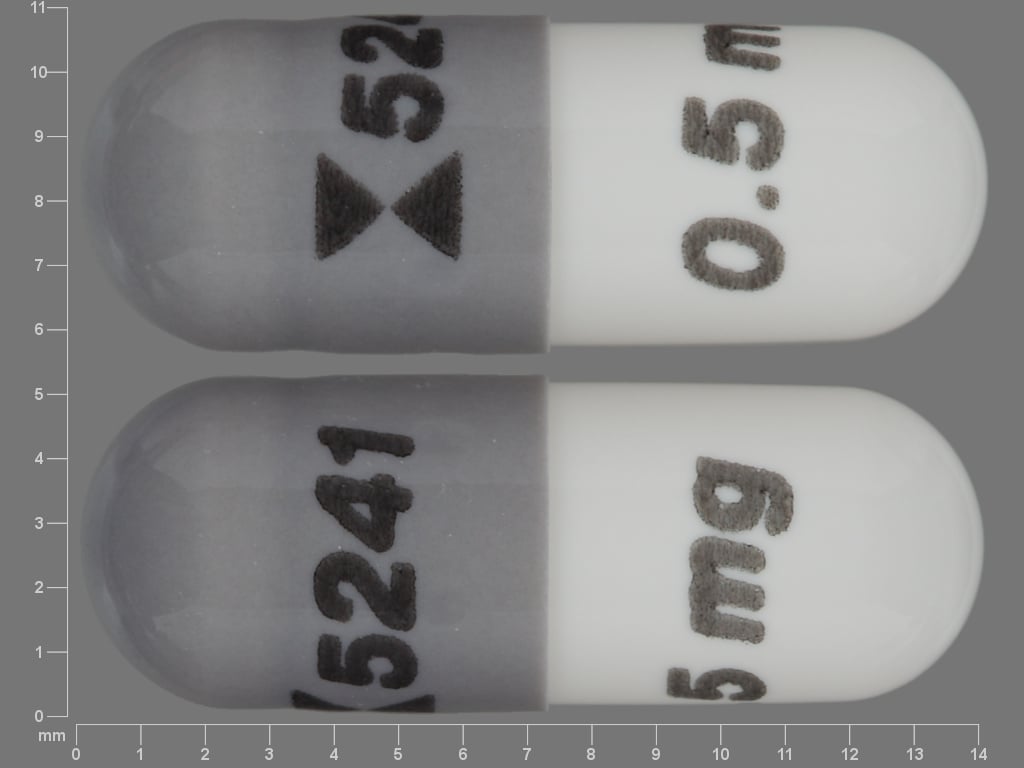
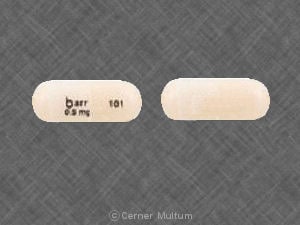
Capsule, Oral:
Agrylin: 0.5 mg
Generic: 0.5 mg, 1 mg
Pharmacology
Mechanism of Action
Anagrelide appears to inhibit cyclic nucleotide phosphodiesterase and the release of arachidonic acid from phospholipase, possibly by inhibiting phospholipase A2. Anagrelide also causes a dose-related reduction in platelet production, which results from decreased megakaryocyte hypermaturation (disrupts the postmitotic phase of maturation).
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic; primarily via CYP1A2 to two major metabolites, 3-hydroxy anagrelide (active) and RL603 (inactive)
Excretion
Urine (<1% as unchanged drug; ~3% as 3-hydroxy anagrelide [active metabolite]; 16% to 20% as RL603 [inactive metabolite])
Onset of Action
Initial: Within 7 to 14 days; complete response (platelets ≤600,000/mm3): 4 to 12 weeks
Time to Peak
Serum: ~1 hour (in fasted state), similar data reported in pediatric patients 7 to 14 years of age
Duration of Action
Platelet rebound: Variable; upon discontinuation, platelet count begins to rise within 4 days and returns to baseline in 1 to 2 weeks (may rebound above baseline)
Half-Life Elimination
Anagrelide: ~1.5 hours, similar data reported in pediatric patients 7 to 14 years of age; 3-hydroxy anagrelide: ~2.5 hours
Use in Specific Populations
Special Populations: Hepatic Function Impairment
AUC increased 8-fold in patients with moderate hepatic function impairment.
Special Populations: Elderly
AUC and Cmax of anagrelide were 61% and 36% higher, respectively, in patients ages 65 to 75 years compared to patients ages 22 to 50 years, but the AUC and Cmax of the active metabolite, 3-hydroxy anagrelide, were 37% and 42% lower, respectively, in the older adult population.
Special Populations: Children
In pediatric patients 7 to 14 years of age; data have shown a decreased maximum serum concentration (48%) and AUC (55%) compared to adults when normalized to dose and bodyweight.
Use: Labeled Indications
Essential thrombocythemia: Treatment of thrombocythemia secondary to myeloproliferative neoplasms to reduce elevated platelets and the risk of thrombosis and to reduce associated symptoms (including thrombo-hemorrhagic events).
Note: The use of hydroxyurea and low-dose aspirin may be preferred over anagrelide for the initial treatment of essential thrombocythemia; however, anagrelide may be appropriate in patients who are resistant or intolerant to hydroxyurea (ESMO [Vannucchi 2015]).
Contraindications
There are no contraindications listed in the US manufacturer's labeling.
Canadian labeling: Hypersensitivity to anagrelide or any component of the formulation; severe hepatic impairment.
Dosage and Administration
Dosing: Adult
Essential thrombocythemia (alternative agent): Oral: Initial: 0.5 mg 4 times daily or 1 mg twice daily (most patients will experience adequate response at dose ranges of 1.5 to 3 mg per day).
Dose titration: Maintain initial dose for at least 1 week, then titrate to reduce and maintain platelet count <600,000/mm3 and ideally between 150,000/mm3 and 400,000/mm3; the dose must not be increased by >0.5 mg per day in any 1 week; maximum single dose: 2.5 mg; maximum daily dose: 10 mg
Off-label dosing: Oral: 0.5 mg twice daily for 1 week, then adjust dose to maintain platelet counts at normal (≤450,000/mm3) or near normal (450,000/mm3 to 600,000/mm3) levels (Gisslinger 2013).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Essential thrombocythemia: Very limited data available; several small case series: Children ≥6 years and Adolescents: Oral: Initial: 0.5 mg 2-3 times daily; increase at weekly intervals in 0.5 mg increments until platelet count begins to decrease; usual reported maintenance dose range: 1-2.5 mg/day; maximum daily dose: 10 mg/day (per manufacturer) although the maximum reported dose for essential thrombocythemia: 4 mg/day; once platelet count normalizes, further adjust dose to lowest effective dose; in some cases, discontinuation of therapy has been accomplished (Chintagumpala, 1995; Lackner, 1998; Lackner, 2006); Note: Essential thrombocytopenia is also considered a type myeloproliferative disorder.
Secondary thrombocythemia (associated with myeloproliferative disorders): Children >6 years and Adolescents: Oral: Initial: 0.5 mg once daily; usual range: 0.5 mg 1-4 times daily; median maintenance daily dose: Patient age 7-11 years: 1.75 mg/day; patient age: 11-14 years: 2 mg; Note: Maintain initial dose for ≥1 week, then adjust to the lowest effective dose to reduce and maintain platelet count <600,000/mm3 ideally to the normal range; the dose must not be increased by >0.5 mg per day in any 1 week; maximum single dose: 2.5 mg; maximum daily dose: 10 mg/day
Administration
Oral: May be administered without regard to food.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Anagrelide Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Apixaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Monitor therapy
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cilostazol: Anagrelide may enhance the adverse/toxic effect of Cilostazol. Avoid combination
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Dabigatran Etexilate: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Dabigatran Etexilate. Agents with Antiplatelet Properties may increase the serum concentration of Dabigatran Etexilate. This mechanism applies specifically to clopidogrel. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Dasatinib: May enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Edoxaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Monitor therapy
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enoximone: May enhance the adverse/toxic effect of Anagrelide. Avoid combination
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Milrinone: Anagrelide may enhance the adverse/toxic effect of Milrinone. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Riociguat: Anagrelide may enhance the hypotensive effect of Riociguat. Management: Riociguat is contraindicated with nonselective phosphodiesterase (PDE) inhibitors and PDE type 5 inhibitors. Other types of PDE inhibitors are not contraindicated, but caution is advised and patients should be monitored for hypotension. Monitor therapy
Rivaroxaban: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Rivaroxaban. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
Frequency not always defined; reactions similar in adult and pediatric patients unless otherwise noted.
Cardiovascular: Palpitations (26%), edema (21%), peripheral edema (9%), chest pain (8%), tachycardia (8%), angina pectoris (1% to <5%), cardiac arrhythmia (1% to <5%), cardiac failure (1% to <5%), hypertension (1% to <5%), orthostatic hypotension (1% to <5%), syncope (1% to <5%), vasodilation (1% to <5%), atrial fibrillation, cardiomegaly, cardiomyopathy, cerebrovascular accident, complete atrioventricular block, decreased diastolic pressure (pediatric patients), increased heart rate (pediatric patients), myocardial infarction, pericardial effusion, systolic hypotension (pediatric patients)
Central nervous system: Headache (44%), dizziness (15%), pain (15%), malaise (6%), paresthesia (6%), amnesia (1% to <5%), chills (1% to <5%), confusion (1% to <5%), depression (1% to <5%), drowsiness (1% to <5%), insomnia (1% to <5%), migraine (1% to <5%), nervousness (1% to <5%), fatigue (pediatric patients)
Dermatologic: Skin rash (8%), pruritus (6%), alopecia (1% to <5%)
Gastrointestinal: Diarrhea (26%), nausea (17%), abdominal pain (16%), flatulence (10%), vomiting (10%), anorexia (8%), dyspepsia (5%), constipation (1% to <5%), gastritis (1% to <5%), gastrointestinal hemorrhage (1% to <5%), pancreatitis
Hematologic & oncologic: Anemia (1% to <5%), bruise (1% to <5%), hemorrhage (1% to <5%), thrombocytopenia (1% to <5%)
Hepatic: Increased liver enzymes (1% to <5%)
Neuromuscular & skeletal: Weakness (23%), back pain (6%), arthralgia (1% to <5%), myalgia (1% to <5%), muscle cramps (pediatric patients)
Ophthalmic: Diplopia (1% to <5%), visual field defect (1% to <5%)
Otic: Tinnitus (1% to <5%)
Renal: Hematuria (1% to <5%), renal failure (1%)
Respiratory: Dyspnea (12%), cough (6%), epistaxis (1% to <5%), flu-like symptoms (1% to <5%), pneumonia (1% to <5%), pleural effusion, pulmonary hypertension, pulmonary fibrosis, pulmonary infiltrates
Miscellaneous: Fever (9%)
<1%, postmarketing, and/or case reports: Eosinophilic pneumonitis, hepatotoxicity, hypersensitivity pneumonitis, increased serum ALT (>3 x ULN), increased serum AST (>3 x ULN), interstitial nephritis, interstitial pneumonitis, leukocytosis, prolonged Q-T interval on ECG, skin photosensitivity (pediatric patients), torsades de pointes, ventricular tachycardia
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding risk: The risk for major hemorrhagic events is increased when anagrelide is used concomitantly with aspirin; assess risks versus benefits if using anagrelide in combination with aspirin. Monitor for bleeding, particularly when used concurrently with other agents known to increase bleeding risk (eg, anticoagulants, nonsteroidal anti-inflammatory drugs, antiplatelet agents, other phosphodiesterase 3 [PDE3] inhibitors, selective serotonin reuptake inhibitors).
- Cardiovascular adverse events: Ventricular tachycardia and torsades de pointes have been reported with anagrelide. As with other PDE3 inhibitors, anagrelide may cause vasodilation, tachycardia, palpitations and heart failure. PDE3 inhibitors are associated with decreased survival (compared to placebo) in patients with class III or IV heart failure. In a scientific statement from the American Heart Association, anagrelide has been determined to be an agent that may cause direct myocardial toxicity (magnitude: major) (AHA [Page 2016]). Dose-related increases in heart rate and mean QTc interval have been observed in a clinical trial. The maximum change in mean heart rate was ~8 beats per minute (bpm) at a dose of 0.5 mg and ~29 bpm with a 2.5 mg dose. The maximum mean change in QTc I (individual subject correlation) from placebo was 7 msec and 13 msec with doses of 0.5 and 2.5 mg, respectively. Do not use in patients with hypokalemia, congenital long QT syndrome, a known history of acquired QTc prolongation, or when using concomitant therapy that may prolong the QTc interval. Hypotension accompanied by dizziness may occur, particularly with higher doses. Consider periodic ECG monitoring in patients with heart failure, bradyarrhythmias, or electrolyte abnormalities. The benefits of anagrelide therapy should outweigh risks in patients with cardiovascular disease. Pretreatment cardiovascular evaluation (including ECG) and careful monitoring during treatment is recommended.
- Pulmonary hypertension: Pulmonary hypertension has been reported with anagrelide; evaluate for signs and symptoms of underlying cardiopulmonary disease prior to and during anagrelide therapy.
- Pulmonary toxicity: Interstitial lung disease (including allergic alveolitis, eosinophilic pneumonia, and interstitial pneumonitis) has been associated with anagrelide. The onset is from 1 week to several years after anagrelide initiation, usually presenting with progressive dyspnea with lung infiltrations; symptoms usually improve after discontinuation.
- Renal abnormalities: Renal abnormalities (including hematuria and renal failure) have been observed with anagrelide.
Disease-related concerns:
- Hepatic impairment: Hepatic impairment increases anagrelide exposure and may increase the risk of QTc prolongation. Assess risks versus benefits of anagrelide treatment in patients with mild to moderate hepatic impairment; dosage reduction and careful cardiovascular monitoring are required for moderate impairment. Avoid use in patients with severe impairment. Monitor liver function prior to and during treatment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Monitor platelet count (every 2 days during the first week of treatment and at least weekly thereafter until the maintenance dose is reached; continue to monitor after cessation of treatment); CBC with differential (monitor closely during first 2 weeks of treatment), liver function (ALT and AST; baseline and during treatment), BUN, and serum creatinine (monitor closely during first weeks of treatment); serum electrolytes; blood pressure; heart rate; cardiovascular exam, including ECG (pretreatment; monitor during therapy). Monitor for signs/symptoms of interstitial lung disease and cardiopulmonary disease; monitor for thrombosis or bleeding. Monitor adherence.
Pregnancy
Pregnancy Considerations
Data regarding use of anagrelide during pregnancy is limited (Alkindi 2005; Birgegård 2018; Cornet 2017; Doubek 2004; Sobas 2009; Wright 2001).
Thrombocythemia is associated with an increased risk for adverse pregnancy outcomes including miscarriage, stillbirth, and preeclampsia. When treatment for essential thrombocythemia is needed during pregnancy, other agents are currently preferred (Tefferi 2018).
Patient Education
What is this drug used for?
- It is used to lower platelet count.
Frequently reported side effects of this drug
- Headache
- Loss of strength and energy
- Back pain
- Nausea
- Vomiting
- Passing gas
- Diarrhea
- Lack of appetite
- Heartburn
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes.
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Blue/gray skin discoloration
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Severe dizziness
- Passing out
- Burning or numbness feeling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.