Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Arimidex: 1 mg
Generic: 1 mg
Pharmacology
Mechanism of Action
Anastrozole is a potent and selective nonsteroidal aromatase inhibitor. By inhibiting aromatase, the conversion of androstenedione to estrone, and testosterone to estradiol, is prevented, thereby decreasing tumor mass or delaying progression in patients with tumors responsive to hormones. Anastrozole causes an 85% decrease in estrone sulfate levels.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed; extent of absorption not affected by food
Metabolism
Extensively hepatic (~85%) via N-dealkylation, hydroxylation, and glucuronidation; primary metabolite (triazole) inactive
Excretion
Feces; urine (urinary excretion accounts for ~10% of total elimination, mostly as metabolites)
Onset of Action
Onset of estradiol reduction: 70% reduction after 24 hours; 80% after 2 weeks of therapy
Time to Peak
Plasma: ~2 hours without food; 5 hours with food
Duration of Action
Duration of estradiol reduction: 6 days
Half-Life Elimination
~50 hours
Protein Binding
Plasma: 40%
Use in Specific Populations
Special Populations: Renal Function Impairment
Renal clearance is decreased proportionally with CrCl and was approximately 50% lower in those with severe renal function impairment (CrCl less than 30 mL/minute per 1.73 m2); this reduced total body clearance by 10%.
Special Populations: Hepatic Function Impairment
Oral clearance was approximately 30% lower in those with stable hepatic cirrhosis, but plasma concentrations were within normal range.
Use: Labeled Indications
Breast cancer:
First-line treatment of locally-advanced or metastatic breast cancer (hormone receptor-positive or unknown) in postmenopausal women
Adjuvant treatment of early hormone receptor-positive breast cancer in postmenopausal women
Treatment of advanced breast cancer in postmenopausal women with disease progression following tamoxifen therapy
Use: Off Label
Endometrial or uterine cancers (recurrent or metastatic)c
Hormonal agents such as progestational agents or tamoxifen may be used in the management of recurrent or metastatic endometrial cancer. In select patients, aromatase inhibitors, including anastrozole may be considered. A small phase II trial evaluated anastrozole in a group of unselected patients with advanced recurrent or persistent endometrial cancer; the results showed minimal activity of anastrozole Rose 2000. A retrospective analysis of patients with uterine leiomyosarcoma suggests that, in patients with low disease burden and an indolent course (who are estrogen- or progesterone-receptor positive), hormone blockade with an aromatase inhibitor such as anastrozole may be considered O'Cearbhaill 2010.
Ovarian cancer (recurrent)c
Hormonal therapy, including aromatase inhibitors such as anastrozole, may be considered in patients with recurrent ovarian cancer who cannot tolerate or have not responded to other chemotherapy regimens. Data from a small phase II study in patients with ovarian cancer suggests that anastrozole may lead to a response in a small number of patients, and is well tolerated del Carmen 2003.
Risk reduction for breast cancer in postmenopausal womena
Data from a large international, randomized, placebo-controlled, double-blind phase III study (IBIS-II) supports the use of anastrozole in the prevention of breast cancer in high-risk postmenopausal women Cuzick 2014.
Contraindications
Hypersensitivity to anastrozole or any component of the formulation
Canadian labeling: Additional contraindications (not in the US labeling): Pregnancy, breastfeeding
Dosage and Administration
Dosing: Adult
Breast cancer, advanced: Postmenopausal females: Oral: 1 mg once daily; continue until tumor progression
Breast cancer, advanced, estrogen receptor-positive, HER2-negative (off-label combination):
Postmenopausal females: Oral: 1 mg once daily (in combination with abemaciclib) until disease progression or unacceptable toxicity (Goetz 2017)
Premenopausal or perimenopausal females: Oral: 1 mg once daily (in combination with ribociclib [and the luteinizing hormone-releasing hormone (LHRH) agonist goserelin]) until disease progression or unacceptable toxicity (Tripathy 2018)
Breast cancer, early (adjuvant treatment): Postmenopausal females: Oral: 1 mg once daily
Duration of therapy: The American Society of Clinical Oncology (ASCO) guidelines for Adjuvant Endocrine Therapy of Hormone-Receptor Positive Breast Cancer (Focused Update) recommend a maximum duration of 5 years of aromatase inhibitor (AI) therapy for postmenopausal women; AIs may be combined with tamoxifen for a total duration of up to 10 years of endocrine therapy. Refer to the guidelines for specific recommendations based on menopausal status and tolerability (Burstein 2014). In a phase III study with another AI (letrozole), treatment with an additional 5 years of AI therapy (for a total of 10 years of AI therapy) demonstrated a significantly improved rate of disease-free survival and a decreased risk of disease recurrence and contralateral breast cancer (when compared to placebo), although overall survival was not significantly different between groups and bone-related adverse events occurred more frequently with letrozole versus placebo (Goss 2016). The decision to extend aromatase inhibitor therapy for an additional 5 years should include initial adjuvant therapy (tamoxifen versus an aromatase inhibitor) and an assessment of the risk of recurrence.
Breast cancer, risk reduction (off-label use): Postmenopausal females ≥40 years of age: Oral: 1 mg once daily for 5 years (Cuzick 2014)
Endometrial or uterine cancer, recurrent or metastatic (off-label use): Oral: 1 mg once daily (Rose 2000)
Ovarian cancer, recurrent (off-label use): Oral: 1 mg once daily until disease progression or unacceptable toxicity (del Carmen 2003)
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: May be administered with or without food.
Storage
Store at 20°C to 25°C (68°F to 77°F).
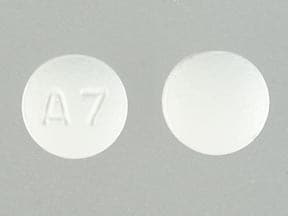
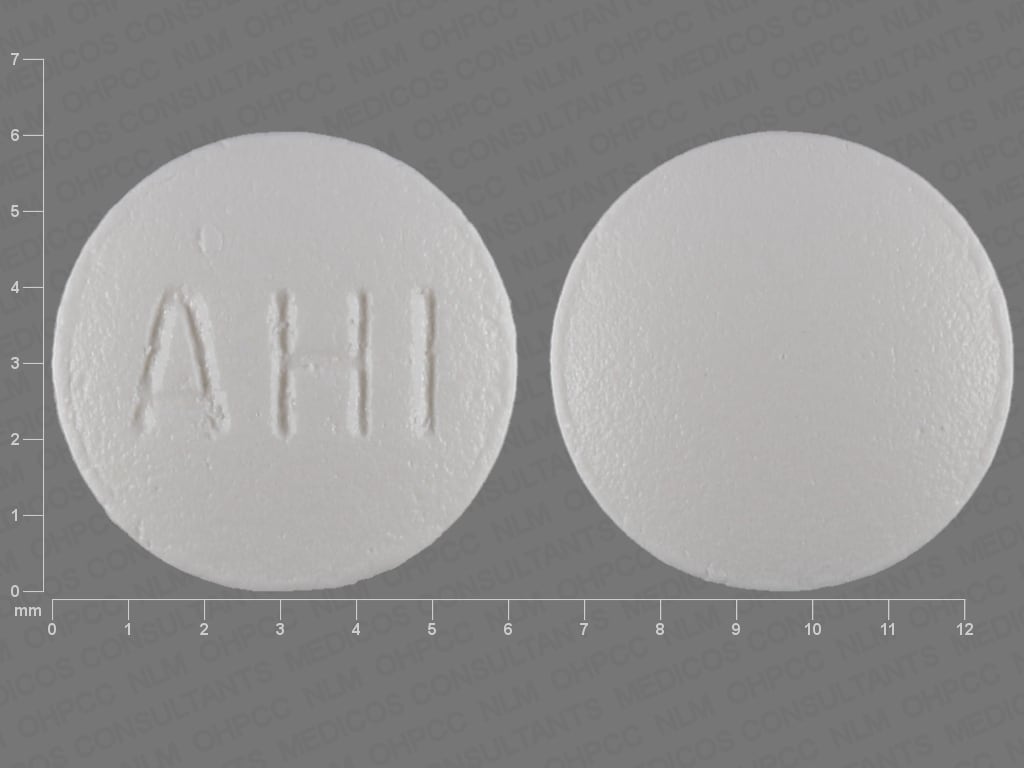
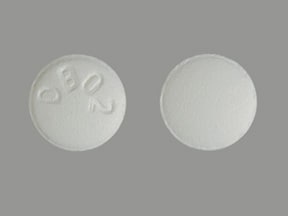
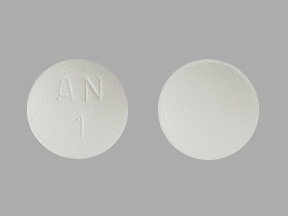
Anastrozole Images
Drug Interactions
Estrogen Derivatives: May diminish the therapeutic effect of Anastrozole. Avoid combination
Levomethadone: Aromatase Inhibitors may increase the serum concentration of Levomethadone. Monitor therapy
Methadone: Aromatase Inhibitors may increase the serum concentration of Methadone. Monitor therapy
Tamoxifen: May decrease the serum concentration of Anastrozole. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Vasodilation (25% to 36%), ischemic heart disease (4%; 17% in patients with preexisting ischemic heart disease), hypertension (5% to 13%), angina pectoris (2%; 12% in patients with preexisting ischemic heart disease)
Dermatologic: Skin rash (6% to 11%)
Endocrine & metabolic: Hot flash (12% to 36%)
Gastrointestinal: Gastrointestinal distress (29% to 34%), nausea (11% to 19%), vomiting (≤13%)
Nervous system: Mood disorder (19%), fatigue (≤19%), pain (11% to 17%), headache (9% to 13%), depression (5% to 13%)
Neuromuscular & skeletal: Asthenia (≤19%), arthritis (17%), arthralgia (15%), back pain (10% to 12%), osteoporosis (11%), ostealgia (6% to 11%),
Respiratory: Pharyngitis (6% to 14%), increased cough (8% to 11%)
1% to 10%:
Cardiovascular: Peripheral edema (5% to 10%), edema (7%), chest pain (5% to 7%), thrombophlebitis (2% to 5%), thromboembolic disease (3% to 4%), venous thrombosis (3%), cerebral ischemia (2%), deep vein thrombosis (2%), acute myocardial infarction (1%)
Dermatologic: Alopecia (2% to 5%), diaphoresis (2% to 5%), pruritus (2% to 5%)
Endocrine & metabolic: Hypercholesterolemia (9%), weight gain (2% to 9%), increased gamma-glutamyl transferase (2% to 5%), weight loss (2% to 5%)
Gastrointestinal: Diarrhea (8% to 9%), abdominal pain (7% to 9%), constipation (7% to 9%), dyspepsia (7%), gastrointestinal disease (7%), anorexia (5% to 7%), xerostomia (4% to 6%)
Genitourinary: Mastalgia (8%), urinary tract infection (8%), vulvovaginitis (6%), pelvic pain (5%), vaginal hemorrhage (1% to 5%), vaginal discharge (4%), vaginitis (4%), leukorrhea (2% to 3%), vaginal dryness (2%)
Hematologic & oncologic: Lymphedema (10%), breast neoplasm (5%), neoplasm (5%), leukopenia (2% to 5%), anemia (4%), tumor flare (3%)
Hepatic: Increased serum alanine aminotransferase (2% to 5%), increased serum alkaline phosphatase (2% to 5%), increased serum aminotransferase (2% to 5%)
Infection: Infection (9%)
Nervous system: Insomnia (6% to 10%), dizziness (6% to 8%), paresthesia (5% to 7%), anxiety (6%), confusion (2% to 5%), drowsiness (2% to 5%), malaise (2% to 5%), nervousness (2% to 5%), carpal tunnel syndrome (3%), hypertonia (3%), lethargy (1%)
Neuromuscular & skeletal: Bone fracture (1% to 10%), arthropathy (6% to 7%), myalgia (6%), neck pain (2% to 5%), pathological fracture (2% to 5%)
Ophthalmic: Cataract (6%)
Respiratory: Dyspnea (8% to 10%), flu-like symptoms (6% to 7%), sinusitis (6%), bronchitis (5%), rhinitis (2% to 5%)
Miscellaneous: Accidental injury (10%), cyst (5%), fever (2% to 5%)
Frequency not defined: Cardiovascular: Cerebral infarction, pulmonary embolism, retinal thrombosis
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, anaphylaxis, angioedema, decreased bone mineral density, dermal ulcer, endometrial carcinoma, erythema multiforme, hepatitis, hepatomegaly, hypercalcemia, increased serum bilirubin, jaundice, skin blister, skin lesion, Stevens-Johnson syndrome, subacute cutaneous lupus erythematosus (Fisher 2016), tenosynovitis (stenosing), urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Decreased bone mineral density: Due to decreased circulating estrogen levels, anastrozole is associated with a reduction in bone mineral density (BMD); decreases (from baseline) in total hip and lumbar spine BMD have been reported. Patients with preexisting osteopenia are at higher risk for developing osteoporosis (Eastell 2008). When initiating anastrozole treatment, follow available guidelines for bone mineral density management in postmenopausal women with similar fracture risk; concurrent use of bisphosphonates may be useful in patients at risk for fractures.
- Hypercholesterolemia: Elevated total cholesterol levels (contributed to by LDL cholesterol increases) have been reported in patients receiving anastrozole; use with caution in patients with hyperlipidemias. Cholesterol levels should be monitored/managed in accordance with current guidelines for patients with LDL elevations.
- Hypersensitivity: Allergic reactions, including anaphylaxis, angioedema, and urticaria, have been reported.
Disease-related concerns:
- Hepatic impairment: Plasma concentrations in patients with stable hepatic cirrhosis were within the range of concentrations seen in normal subjects across all clinical trials. Has not been studied in patients with severe hepatic impairment.
- Ischemic disease: Patients with preexisting ischemic cardiac disease have an increased risk for ischemic cardiovascular events.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Premenopausal females: Aromatase inhibitors (including anastrozole) should not be used as monotherapy in premenopausal women with breast cancer (Puhalla 2009). Premenopausal females with metastatic breast cancer should be offered ovarian suppression or ablation along with hormonal therapy (Rugo 2016).
Monitoring Parameters
Bone mineral density; total cholesterol and LDL. Pregnancy test (prior to treatment in females of reproductive potential). Monitor adherence.
Breast cancer risk reduction (off-label use): Bone mineral density at baseline, mammograms, and clinical breast exam at baseline and at least every 2 years (Cuzick 2014)
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and information from animal reproduction studies, anastrozole may cause fetal harm if exposure occurs during pregnancy.
Evaluate pregnancy status prior to therapy. Females of reproductive potential should use effective contraception during therapy and for at least 3 weeks after the last anastrozole dose.
Patient Education
What is this drug used for?
- It is used to treat breast cancer in women after change of life.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hot flashes
- Loss of strength and energy
- Weight gain
- Anxiety
- Sweating a lot
- Flu-like symptoms
- Dry mouth
- Pelvic pain
- Constipation
- Diarrhea
- Nausea
- Vomiting
- Joint pain
- Joint swelling
- Muscle pain
- Trouble sleeping
- Cough
- Sore throat
- Back pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Shortness of breath
- Swelling of arms or legs
- Severe headache
- Burning or numbness feeling
- Swollen glands
- Bone pain
- Chest pain
- Mood changes
- Depression
- Severe dizziness
- Passing out
- Vision changes
- Breast pain
- Abnormal vaginal bleeding
- Vaginal pain, itching, and discharge
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.