Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Malarone: Atovaquone 250 mg and proguanil hydrochloride 100 mg
Generic: Atovaquone 250 mg and proguanil hydrochloride 100 mg
Tablet, Oral [pediatric]:
Malarone: Atovaquone 62.5 mg and proguanil hydrochloride 25 mg
Generic: Atovaquone 62.5 mg and proguanil hydrochloride 25 mg
Pharmacology
Mechanism of Action
Atovaquone: Selectively inhibits parasite mitochondrial electron transport.
Proguanil: The metabolite cycloguanil inhibits dihydrofolate reductase, disrupting deoxythymidylate synthesis. Together, atovaquone/cycloguanil affect the erythrocytic and exoerythrocytic stages of development.
Pharmacokinetics/Pharmacodynamics
Absorption
Atovaquone: The rate and extent of absorption is increased when administered with dietary fat.
Proguanil: Extensive
Distribution
Vd:
Atovaquone: Children and Adults: ~8.8 L/kg
Proguanil: Children >15 years and Adults and 31-110 kg: 1617-2502 L; Pediatric patients ≤15 years and 11-56 kg: 462-966 L; concentrated in erythrocytes
Metabolism
Proguanil: Hepatic to active metabolites, cycloguanil (via CYP2C19) and 4-chlorophenylbiguanide
Excretion
Atovaquone: Feces (>94% as unchanged drug); urine (<0.6%)
Proguanil: Urine (40% to 60%)
Half-Life Elimination
Atovaquone: 2-3 days (adults), 1-2 days (children)
Proguanil: 12-21 hours
Protein Binding
Atovaquone: >99%
Proguanil: 75%
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with moderate renal impairment (CrCl 30-50 mL/minute), mean oral clearance for proguanil was reduced by ~35% compared with patients with normal renal function CrCl >80 mL/minute). In patients with severe renal impairment (CrCl <30 mL/minute), atovaquone Cmax and AUC are reduced, but the elimination half-lives for proguanil and cycloguanil are prolonged, with corresponding increases in AUC, resulting in the potential of drug accumulation and toxicity with repeated dosing.
Special Populations: Hepatic Function Impairment
Atovaquone elimination half-life was increased in patients with moderate hepatic impairment. Proguanil AUC, Cmax, and elimination half-life were increased and cycloguanil (metabolite) AUC and Cmax were decreased and elimination half-life was increased in patients with mild hepatic impairment. Proguanil AUC and Cmax were increased in patients with moderate hepatic impairment. The pharmacokinetics of atovaquone, proguanil, and cycloguanil have not been studied in patients with severe hepatic impairment.
Special Populations: Elderly
AUC was increased, Tmax was longer, and elimination half-life was longer in elderly subjects (~15 hours) compared to younger subjects (~8 hours).
Use: Labeled Indications
Malaria due to Plasmodium falciparum, prevention: Prophylaxis of P. falciparum malaria, including areas where chloroquine resistance has been reported
Malaria (uncomplicated) due to P. falciparum, treatment: Treatment of acute, uncomplicated P. falciparum malaria
Use: Off Label
Malaria (uncomplicated) due to Plasmodium vivax, treatmentyes
Based on the Centers for Disease Control and Prevention (CDC) guidelines for the treatment of malaria in the United States, atovaquone/proguanil (in combination with primaquine) is effective and recommended for the treatment of uncomplicated, chloroquine-resistant P. vivax malaria.
Contraindications
Hypersensitivity to atovaquone, proguanil, or any component of the formulation; prophylactic use in severe renal impairment (CrCl <30 mL/minute)
Dosage and Administration
Dosing: Adult
Malaria: Oral:
Prevention of P. falciparum malaria: Atovaquone/proguanil 250 mg/100 mg once daily; start 1 to 2 days prior to entering a malaria-endemic area, continue throughout the stay and for 7 days after returning.
Treatment of uncomplicated P. falciparum malaria: Atovaquone/proguanil 1,000 mg/400 mg once daily for 3 consecutive days
Treatment of uncomplicated P. vivax malaria (off-label use): Atovaquone/proguanil 1,000 mg/400 mg once daily for 3 consecutive days, in combination with primaquine (CDC 2013)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Tablets are available in different strengths (pediatric and adult tablets) and both may be used in pediatric patients depending upon patient weight; use extra precaution
Malaria; prevention (Yellow Book [CDC 2018]): Infants, Children, and Adolescents: Begin 1 to 2 days prior to entering a malaria-endemic area, continue throughout the stay and for 7 days after leaving area: Oral:
5 to 8 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 31.25 mg atovaquone/12.5 mg proguanil (1/2 tablet) once daily
>8 to 10 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 46.88 mg atovaquone/18.75 mg proguanil (3/4 tablet) once daily
>10 to 20 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 62.5 mg atovaquone/25 mg proguanil (1 tablet) once daily
>20 to 30 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 125 mg atovaquone/50 mg proguanil (2 tablets) once daily
>30 to 40 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 187.5 mg atovaquone/75 mg proguanil (3 tablets) once daily
>40 kg: Adult tablet (250 mg atovaquone/100 mg proguanil per tablet): 250 mg atovaquone/100 mg proguanil (1 tablet) once daily
Malaria; treatment, uncomplicated P. falciparum or P. vivax (CDC 2013): Infants, Children, and Adolescents: Oral:
5 to 8 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 125 mg atovaquone/50 mg proguanil (2 tablets) once daily for 3 doses
9 to 10 kg: Pediatric tablet (62.5 mg atovaquone/25 mg proguanil per tablet): 187.5 mg atovaquone/75 mg proguanil (3 tablets) once daily for 3 doses
11 to 20 kg: Adult tablet (250 mg atovaquone/100 mg proguanil per tablet): 250 mg atovaquone/100 mg proguanil (1 tablet) once daily for 3 doses
21 to 30 kg: Adult tablet (250 mg atovaquone/100 mg proguanil per tablet): 500 mg atovaquone/proguanil/200 mg proguanil (2 tablets) once daily for 3 doses
31 to 40 kg: Adult tablet (250 mg atovaquone/100 mg proguanil per tablet): 750 mg atovaquone/300 mg proguanil (3 tablets) once daily for 3 doses
>40 kg: Adult tablet (250 mg atovaquone/100 mg proguanil per tablet): 1,000 mg atovaquone/400 mg proguanil (4 tablets) once daily for 3 doses
Administration
Administer with food or milk-based drink at the same time each day. If vomiting occurs within 1 hour of administration, repeat the dose. For patients who have difficulty swallowing tablets, tablets may be crushed and mixed with condensed milk just prior to administration.
Dietary Considerations
Must be taken with food or milk-based drink.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
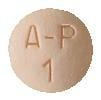
Atovaquone and Proguanil Images
Drug Interactions
Antihepaciviral Combination Products: May decrease the serum concentration of Proguanil. Monitor therapy
Antipsychotic Agents (Phenothiazines): Antimalarial Agents may increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Artemether: May enhance the adverse/toxic effect of Antimalarial Agents. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C19 Inhibitors (Strong): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
Dapsone (Systemic): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Dapsone (Topical): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Topical). Specifically, the risk of hemolytic reactions may be increased. Management: Closely monitor for signs/symptoms of hemolytic reactions with concomitant use of topical dapsone and antimalarial agents. Patients with glucose-6-phosphate dehydrogenase deficiency may be at particularly high risk for adverse hematologic effects. Consider therapy modification
Efavirenz: May decrease the serum concentration of Atovaquone. Management: Consider alternatives to the use of atovaquone with efavirenz when possible. If this combination must be used, monitor for evidence of reduced atovaquone clinical effectiveness. Consider therapy modification
Ethinyl Estradiol: May diminish the therapeutic effect of Proguanil. Monitor therapy
Etoposide: Atovaquone may increase the serum concentration of Etoposide. Management: Consider separating the administration of atovaquone and etoposide by at least 1 to 2 days. Monitor therapy
Etoposide Phosphate: Atovaquone may increase the serum concentration of Etoposide Phosphate. Management: Consider separating the administration of atovaquone and etoposide by at least 1 to 2 days. Monitor therapy
Indinavir: Atovaquone may decrease the serum concentration of Indinavir. Monitor therapy
Lumefantrine: Antimalarial Agents may enhance the adverse/toxic effect of Lumefantrine. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Metoclopramide: May decrease the serum concentration of Atovaquone. Management: Consider alternatives to metoclopramide when possible; atovaquone should only be used with metoclopramide if no other antiemetics are available. Consider therapy modification
Pyrimethamine: May enhance the adverse/toxic effect of Proguanil. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Atovaquone. Avoid combination
Ritonavir: May decrease the serum concentration of Atovaquone. Monitor therapy
Ritonavir: May decrease the serum concentration of Proguanil. Monitor therapy
Tetracycline (Systemic): May decrease the serum concentration of Atovaquone. Monitor therapy
Typhoid Vaccine: Proguanil may diminish the therapeutic effect of Typhoid Vaccine. This applies only to the oral (live) typhoid vaccine. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with proguanil. When possible, proguanil should not be started within 10 days of the last vaccine dose. Consider therapy modification
Warfarin: Proguanil may enhance the anticoagulant effect of Warfarin. Monitor therapy
Adverse Reactions
The following adverse reactions were reported in patients being treated for malaria. When used for prophylaxis, reactions are similar to those seen with placebo.
>10%:
Gastrointestinal: Abdominal pain (17%), nausea (12%), vomiting (children: 10% to 13%; adults: 12%)
Hepatic: Increased serum ALT (27%; increased liver function test values typically normalized after ~ 4 weeks), increased serum AST (17%; increased liver function test values typically normalized after ~4 weeks)
1% to 10%:
Central nervous system: Headache (10%), dizziness (5%)
Dermatologic: Pruritus (children: 6%)
Gastrointestinal: Diarrhea (children: 6%; adults: 8%), anorexia (5%)
Neuromuscular & skeletal: Weakness (8%)
<1%, postmarketing, and/or case reports: Anaphylaxis (rare), anemia (rare), angioedema, cholestasis, erythema multiforme (rare), hallucination, hepatic failure (case report), hepatitis (rare), neutropenia, pancytopenia (with severe renal impairment), psychotic reaction (rare), seizure (rare), skin photosensitivity, skin rash, Stevens-Johnson syndrome (rare), stomatitis, urticaria, vasculitis (rare)
Warnings/Precautions
Concerns related to adverse events:
- Hepatic effects: Increased transaminase levels and hepatitis have been reported with prophylactic use; single case report of hepatic failure requiring transplantation documented. Monitor closely and use caution in patients with existing hepatic impairment. Elevations in AST/ALT may persist for up to 4 weeks following treatment (Looareesuwan, 1999).
Disease-related concerns:
- Diarrhea/vomiting: Absorption of atovaquone may be decreased in patients who have diarrhea or vomiting; monitor closely and consider use of an antiemetic. If severe, consider use of an alternative antimalarial.
- Malaria: Appropriate use: Not indicated for cerebral malaria or other severe manifestations of complicated malaria. Delayed cases of P. falciparum malaria may occur after stopping prophylaxis; travelers returning from endemic areas who develop febrile illnesses should be evaluated for malaria. Recrudescent infections or infections following prophylaxis with this agent should be treated with alternative agent(s).
- Renal impairment: Use with caution in patients with preexisting renal disease. May use with caution for treatment of malaria in patients with severe renal impairment (CrCl <30 mL/minute) if benefit outweighs risk. Contraindicated for prophylactic use in severe renal impairment due to the risk of pancytopenia in patients with severe renal impairment treated with proguanil.
Special populations:
- Obesity: Treatment failures have been reported in patients >100 kg (case reports); follow-up monitoring is recommended (Durand, 2008).
Monitoring Parameters
Liver and renal function; closely monitor response to treatment in patients with vomiting or diarrhea and in patients >100 kg (Durand, 2008)
Pregnancy
Pregnancy Considerations
Outcome information following maternal use of atovaquone and proguanil in pregnancy is limited (Andrejko 2019; Mayer 2018; Pasternak 2011).
The pharmacokinetics of atovaquone and proguanil may be altered during pregnancy (Burger 2016). Malaria infection in pregnant women may be more severe than in nonpregnant women. Because P. falciparum malaria can cause maternal death and fetal loss, pregnant women traveling to malaria-endemic areas must use personal protection against mosquito bites. Atovaquone/proguanil may be used as an alternative treatment of malaria in pregnant women; consult current CDC guidelines (CDC 2013).
Patient Education
What is this drug used for?
- It is used to treat or prevent malaria.
Frequently reported side effects of this drug
- Headache
- Cough
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Fever
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.