Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Injection, as mesylate:
Cogentin: 1 mg/mL (2 mL)
Generic: 1 mg/mL (2 mL)
Solution, Injection, as mesylate [preservative free]:
Generic: 1 mg/mL (2 mL)
Tablet, Oral, as mesylate:
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Possesses both anticholinergic and antihistaminic effects. In vitro anticholinergic activity approximates that of atropine; in vivo it is only about half as active as atropine. Animal data suggest its antihistaminic activity and duration of action approach that of pyrilamine maleate.
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic (N-oxidation, N-dealkylation, and ring hydroxylation) (from animal studies only) (Brocks 1999)
Onset of Action
IM, IV: Within a few minutes; there is no significant difference between onset of effect after intravenous or intramuscular injection
Oral: Within 1 hour
Time to Peak
Plasma: Oral: 7 hours (Brocks 1999)
Use: Labeled Indications
Drug-induced extrapyramidal symptoms, acute treatment: Acute treatment drug-induced extrapyramidal symptoms (excluding tardive dyskinesia).
Parkinsonism: Adjunctive therapy of all forms of parkinsonism.
Contraindications
Hypersensitivity to benztropine mesylate or any component of the formulation.
Children <3 years of age (due to atropine-like adverse effects including severe anhidrosis and fatal hyperthermia) and should be used cautiously in older children.
Dosage and Administration
Dosing: Adult
Drug-induced extrapyramidal symptoms:
Acute treatment: IM, IV, Oral: Note: Parenteral administration is preferred for initial treatment of severe acute symptoms. Treatment should continue with oral administration for several days to prevent recurrence. Oral prophylactic use is generally not recommended to prevent antipsychotic-associated extrapyramidal symptoms (EPS) (Kreyenbuhl 2010). Duration of therapy and prophylactic use should be based on severity of EPS reaction, pharmacologic profile of the causative agent (eg, half-life, adverse effects), and patient risk factors (Holloman 1997; Lavonas 2019; Marder 2019; Tonda 1994).
General dosing recommendations: Initial: IM, IV, Oral: 1 to 2 mg 2 to 3 times daily; adjust dose based on response and tolerability in 0.5 mg increments at intervals >5 days up to a maximum daily dose of 6 mg.
Dystonic reactions:
Initial dose: IM, IV, Oral: 1 to 2 mg once.
Subsequent doses: Oral: 1 to 2 mg 1 to 2 times daily.
Prevention, dystonic reactions: Note: May be useful for preventing acute dystonic reactions when administering drugs with increased risk of causing such reactions (eg, haloperidol, metoclopramide) (Kane 1996; Kreyenbuhl 2010).
IM, IV: 1 to 2 mg prior to administration of high-risk medication (Marder 2019).
Parkinsonism: IM, IV, Oral:
Idiopathic parkinsonism: Initial: 0.5 to 1 mg/day as a single dose at bedtime or in 2 to 4 divided doses. Titrate in 0.5 mg increments every 5 to 6 days based on response and tolerability. Usual dose: 1 to 2 mg/day (range: 0.5 to 6 mg/day) although some patients may need 4 to 6 mg/day; maximum: 6 mg/day.
Postencephalitic parkinsonism: Initial: 2 mg/day as a single dose at bedtime or in 2 to 4 divided doses; a lower initial dose of 0.5 mg at bedtime may be considered in highly sensitive patients. Titrate in 0.5 mg increments every 5 to 6 days based on response and tolerability. Usual dose: 1 to 2 mg/day (range: 0.5 to 6 mg/day); maximum: 6 mg/day.
Note: Lower initial doses may be appropriate for older and thinner patients.
Dosing: Geriatric
Refer to adult dosing. Start at low end of dosing range and increase only as needed and as tolerated.
Dosing: Pediatric
Drug-induced extrapyramidal symptoms (EPS): Limited data available: Note: IV route should be reserved for situations when oral or IM are not appropriate. Prophylactic use is generally not recommended to prevent antipsychotic-associated EPS; consider individual preferences, history of EPS, and baseline risk factors for EPS, including antipsychotic receptor binding and adverse effect profile (Kreyenbuhl 2010).
Children >3 years and Adolescents: Oral, IM, IV: 0.02 to 0.05 mg/kg/dose 1 to 2 times daily has been used for treatment of EPS; usual adult dose range: 1 to 4 mg/dose (Bellman 1974; Habre 1999; Joseph 1995; Nelson 1996; pdp-Benztropine [Canadian manufacturer's labeling 2015]; Teoh 2002). In clinical trials of pediatric patients ≥8 years with early-onset schizophrenia spectrum disorders (EOSS), benztropine 0.5 mg orally every 12 hours has been used to reduce the risk of development of anti-psychotic drug-induced EPS (Findling 2010; McClellan 2007). Note: Use in children <3 years has been reported minimally and should be reserved for life-threatening emergencies.
Administration
Oral: Administer with or without food.
Injectable: Administer IM or IV if oral route is unacceptable. Manufacturer’s labeling states there is no difference in onset of effect after IV or IM injection and therefore there is usually no need to use the IV route. No specific instructions on administering benztropine IV are provided in the labeling. The IV route has been reported in the literature (slow IV push when reported), although specific instructions are lacking (Duncan 2001; Lydon 1998; Sachdev 1993; Schramm 2002).
Storage
Store at 20°C to 25°C (68°F to 77°F).
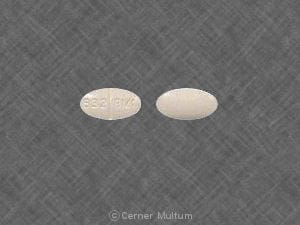
Benztropine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ioflupane I 123: Benztropine may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
Frequency not defined.
Cardiovascular: Tachycardia
Central nervous system: Confusion, depression, disorientation, heatstroke, hyperthermia, lethargy, memory impairment, nervousness, numbness of fingers, psychotic symptoms (exacerbation of pre-existing symptoms), toxic psychosis, visual hallucination
Dermatologic: Skin rash
Gastrointestinal: Constipation, nausea, paralytic ileus, vomiting, xerostomia
Genitourinary: Dysuria, urinary retention
Ophthalmic: Blurred vision, mydriasis
Warnings/Precautions
Concerns related to adverse effects:
- Anhidrosis/hyperthermia: May cause anhidrosis and hyperthermia, which may be severe; use with caution in hot weather or during exercise. The risk is increased in hot environments, particularly in the elderly, alcoholics, patients with CNS disease, and those with prolonged outdoor exposure. If there is evidence of anhidrosis, consider decreasing dose so the ability to maintain body heat equilibrium by perspiration is not impaired.
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention).
- CNS effects: May be associated with confusion, visual hallucinations or excitement (generally at higher dosages); intensification of symptoms or toxic psychosis may occur in patients with mental disorders. May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Weakness: When given in large doses or to susceptible patients, may cause weakness and inability to move particular muscle groups.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with tachycardia.
- GI obstruction: Use with caution in patients with obstructive disease of the GI tract (eg, pyloric or duodenal obstruction).
- Glaucoma: Use with caution in patients with glaucoma; avoid use in angle-closure glaucoma.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture or retention.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Use with caution in children >3 years of age due to its anticholinergic effects; dose has not been established. Use is contraindicated in children <3 years of age.
Other warnings/precautions:
- Tardive dyskinesia: Not recommended for use in patients with tardive dyskinesia; benztropine does not relieve symptoms of tardive dyskinesia and may potentially exacerbate symptoms.
Monitoring Parameters
Pulse, anticholinergic effects (baseline; as clinically indicated)
Pregnancy
Pregnancy Considerations
Paralytic ileus (which resolved rapidly) was reported in two newborns exposed to a combination of benztropine and chlorpromazine during the second and third trimesters and the last 6 weeks of pregnancy, respectively (Falterman 1980).
Patient Education
What is this drug used for?
- It is used to treat Parkinson's disease.
- It is used to treat side effects caused by some other drugs.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Dry mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Mood changes
- Behavioral changes
- Sensing things that seem real but are not
- Confusion
- Severe anxiety
- Vision changes
- Eye pain
- Severe eye irritation
- Difficulty swallowing
- Difficulty speaking
- Lack of appetite
- Weight loss
- Difficult urination
- Painful urination
- Fast heartbeat
- Enlarged pupils
- Trouble with memory
- Severe abdominal pain
- Severe constipation
- Weakness
- Difficulty moving
- Lack of sweating
- Heat stroke
- High fever
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.