Boxed Warning
Distribution program:
Because of the risks of hepatotoxicity and birth defects, bosentan is available only through a restricted program called the Bosentan REMS Program. Under the Bosentan REMS, prescribers, patients, and pharmacies must enroll in the program.
Hepatotoxicity:
In clinical studies, bosentan caused at least a 3-fold upper limit of normal (ULN) elevation of liver aminotransferases (ALT and AST) in about 11% of patients, accompanied by elevated bilirubin in a small number of cases. Because these changes are a marker for potential serious hepatotoxicity, serum aminotransferase levels must be measured prior to initiation of treatment and then monthly. In the postmarketing period, in the setting of close monitoring, rare cases of unexplained hepatic cirrhosis were reported after prolonged (more than 12 months) therapy with bosentan in patients with multiple comorbidities and drug therapies. There have also been reports of liver failure. The contribution of bosentan in these cases could not be excluded.
In at least 1 case, the initial presentation of hepatotoxicity (after more than 20 months of treatment) included pronounced elevations in aminotransferases and bilirubin levels accompanied by nonspecific symptoms, all of which resolved slowly over time after discontinuation of bosentan. This case reinforces the importance of strict adherence to the monthly monitoring schedule for the duration of treatment and the treatment algorithm, which includes stopping bosentan if a rise of aminotransferase accompanied by signs or symptoms of liver dysfunction occurs.
Elevations in aminotransferases require close attention. Generally, avoid using bosentan in patients with elevated aminotransferases (greater than 3 times the ULN) at baseline because monitoring for hepatotoxicity may be more difficult. Stop treatment with bosentan if liver aminotransferase elevations are accompanied by clinical symptoms of hepatotoxicity (eg, abdominal pain, fever, jaundice, nausea, unusual lethargy or fatigue, vomiting) or increases in bilirubin 2 times the ULN or greater. There is no experience with the reintroduction of bosentan in these circumstances.
Embryo-fetal toxicity:
Bosentan is likely to cause major birth defects if used by pregnant women based on animal data. Therefore, pregnancy must be excluded before the start of treatment with bosentan. Throughout treatment and for 1 month after stopping bosentan, women of childbearing potential must use 2 reliable methods of contraception unless the patient has an intrauterine device (IUD) or tubal sterilization in which case no other contraception is needed. Hormonal contraceptives, including oral, injectable, transdermal, and implantable contraceptives, should not be used as the sole means of contraception because these may not be effective in patients receiving bosentan. Obtain monthly pregnancy tests.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Tracleer: 62.5 mg, 125 mg
Generic: 62.5 mg, 125 mg
Tablet Soluble, Oral:
Tracleer: 32 mg [scored; contains aspartame]
Pharmacology
Mechanism of Action
Endothelin receptor antagonist that blocks endothelin receptors on endothelium and vascular smooth muscle (stimulation of these receptors is associated with vasoconstriction). Bosentan blocks both ETA and ETB receptors, with a slightly higher affinity for the A subtype.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~18 L (does not distribute into RBCs)
Metabolism
Hepatic via CYP2C9 and 3A4 to three metabolites (one active, contributing ~10% to 20% pharmacologic activity); steady-state plasma concentrations are 50% to 65% of those attained after single dose (most likely due to autoinduction of liver enzymes); steady-state is attained within 3 to 5 days
Excretion
Feces (as metabolites); urine (<3% as unchanged drug)
Time to Peak
Plasma: 3 to 5 hours
Half-Life Elimination
~5 hours; prolonged with heart failure, possibly with PAH
Protein Binding
Plasma: >98%, primarily to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with severe renal impairment (CrCl 15 to 30 mL/minute), concentrations of the 3 metabolites may increase 2-fold, although it is not clinically significant.
Special Populations: Hepatic Function Impairment
Exposure to bosentan may be significantly increased in hepatic impairment.
Special Populations: Children
Exposure to bosentan reaches a plateau at lower doses in pediatric patients than in adults, and doses >2 mg/kg twice daily do not increase the exposure to bosentan in pediatric patients.
Use: Labeled Indications
Pulmonary arterial hypertension: Treatment of pulmonary artery hypertension (PAH) (WHO Group I) in adults with WHO-FC II, III, or IV symptoms to improve exercise ability and to decrease clinical deterioration; treatment of PAH (WHO Group 1) in pediatric patients ≥3 years with idiopathic or congenital PAH to improve pulmonary vascular resistance (PVR), resulting in an improvement in exercise ability.
Note: According to treatment guidelines from the Fifth World Symposium on Pulmonary Hypertension (WSPH), only a small number of PAH patients with WHO-FC IV symptoms (ie, severely ill patients) were included in clinical trials, therefore, most experts consider bosentan second-line therapy in these patients (WSPH [Gailè 2013]).
Use: Off Label
Prevention of digital ulcers in systemic sclerosisb
Based on small controlled trials, bosentan may be effective for patients with digital ulcers caused by systemic sclerosis. Bosentan has been found to decrease the number of new ulcers, but has not been found to improve healing of existing ulcers
Raynaud phenomenon in systemic sclerosiscyes
Data from controlled and noncontrolled trials evaluating bosentan in the management of secondary Raynaud phenomenon demonstrate conflicting results in clinical and microvascular assessments Giordano 2010, Hettema 2007, Moore 2007, Nguyen 2010. According to evidence-based international consensus-derived recommendations, bosentan has no confirmed efficacy in the treatment of active digital ulcers in systemic sclerosis patients but is effective in the prevention of digital ulcers, particularly multiple ulcers, and should be considered after other therapies have failed EULAR [Kowal-Bielecka 2009].
Contraindications
Hypersensitivity to bosentan or any component of the formulation; concurrent use of cyclosporine or glyburide; use in women who are or may become pregnant.
Canadian labeling: Additional contraindications (not in US labeling): Moderate to severe hepatic impairment (eg, ALT or AST >3 times ULN, particularly when total bilirubin >2 times ULN).
Dosage and Administration
Dosing: Adult
Pulmonary artery hypertension: Oral:
<40 kg: Initial and maintenance: 62.5 mg twice daily
≥40 kg: Initial: 62.5 mg twice daily for 4 weeks; increase to maintenance dose of 125 mg twice daily. Doses >125 mg twice daily do not appear to confer additional clinical benefit but may increase risk of hepatotoxicity.
Note: When discontinuing treatment, consider a reduction in dosage to 62.5 mg twice daily for 3 to 7 days (to avoid clinical deterioration).
Coadministration with ritonavir: Oral:
Dosage adjustment for concurrent use with ritonavir:
Coadministration of bosentan in patients currently receiving ritonavir for at least 10 days: Begin with bosentan 62.5 mg once daily or every other day based on tolerability.
Coadministration of ritonavir in patients currently receiving bosentan: Discontinue bosentan 36 hours prior to the initiation of ritonavir. After at least 10 days following the initiation of ritonavir, resume bosentan 62.5 mg once daily or every other day based on tolerability.
Prevention of digital ulcers in systemic sclerosis (off-label use): Oral: 62.5 mg twice daily for 4 weeks followed by an increase to a maintenance dose of 125 mg twice daily; has been studied in clinical trials for up to 12 weeks (Korn 2004)
Raynaud phenomenon in systemic sclerosis (off-label use): Oral: 62.5 mg twice daily for 4 weeks followed by an increase to a maintenance dose of 125 mg twice daily (Giordano 2010; Hettema 2007).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Pulmonary arterial hypertension: Note: Doses >125 mg twice daily do not provide additional benefit sufficient to offset the increased risk of hepatic injury.
Infants and Children <12 years: Oral: Initial: 1 mg/kg/dose twice daily; increase to a target dose of 2 mg/kg/dose twice daily; maximum dose: 125 mg/dose (AHA/ATS [Abman 2015]; Berger 2017)
Children ≥12 years and Adolescents (AHA/ATS [Abman 2015]): Oral:
>20 to 40 kg: Initial: 31.25 mg twice daily; increase to a target dose of 62.5 mg twice daily
>40 kg: Initial: 62.5 mg twice daily; increase to a target dose of 125 mg twice daily
Alternate dosing: Manufacturer's labeling:
Children ≥3 years:
4 to 8 kg: Oral: 16 mg twice daily
>8 to 16 kg: Oral: 32 mg twice daily
>16 to 24 kg: Oral: 48 mg twice daily
>24 to 40 kg: Oral: 64 mg twice daily
Adolescents:
≤40 kg: Oral: 62.5 mg twice daily
>40 kg: Oral: Initial: 62.5 mg twice daily for 4 weeks; increase to target dose of 125 mg twice daily
Dosage adjustment for concurrent use with ritonavir:
Coadministration of bosentan in patients currently receiving ritonavir for at least 10 days: There are no pediatric-specific recommendations; based on experience in adult patients, dosage adjustment suggested.
Coadministration of ritonavir in patients currently receiving bosentan: There are no pediatric-specific recommendations; based on experience in adult patients, discontinue bosentan 36 hours prior to the initiation of ritonavir. After at least 10 days following the initiation of ritonavir, resume bosentan at an adjusted dose.
Extemporaneously Prepared
Note: Tablets for oral suspension (32 mg dispersible tablets) are commercially available.
6.25 mg/mL Oral Suspension
Note: The following personal protective equipment should be used when preparing bosentan oral suspension: Double gloving, protective gown and a respiratory mask if preparation does not occur in a fume hood.
A 6.25 mg/mL oral suspension may be made from nondispersable tablets and a 1:1 mixture of FlavorPlus and FlavorSweet. Crush three 62.5 mg tablets in a ceramic mortar. Add a small amount of glycerin and reduce to a fine powder. Add ~10 mL of the vehicle and triturate; add an additional 10 mL of vehicle and transfer to a calibrated amber bottle. Rinse the mortar and pestle with 10 mL vehicle and add to bottle to bring the final volume to 30 mL. Stable for 30 days when stored in a amber bottle at room temperature or under refrigeration.
Malik A, Gorman G, Coward L, Arnold JJ. Stability of an extemporaneously compounded oral suspension of bosentan. Hosp Pharm. 2016;51(5):389-95. doi: 10.1310/hpj5105-389.27303093
Administration
Administer with or without food.
Tablets for oral suspension (dispersible tablets): Disperse in a minimal amount of water immediately before administration. The 32 mg dispersible tablet may be divided into halves; do not break into quarters.
Storage
Store film-coated and dispersible tablets at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store divided dispersible tablet pieces in the opened blister for up to 7 days.
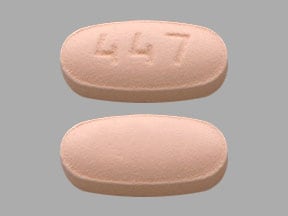
Bosentan Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Abemaciclib. Avoid combination
Antihepaciviral Combination Products: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Asunaprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Asunaprevir. Avoid combination
Atazanavir: Bosentan may decrease the serum concentration of Atazanavir. Atazanavir may increase the serum concentration of Bosentan. Management: Concurrent use of atazanavir (without ritonavir) and bosentan is not recommended. Bosentan dose adjustments are required when used together with atazanavir/ritonavir. Consider therapy modification
Avapritinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Axitinib. Avoid combination
Bedaquiline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bedaquiline. Avoid combination
Benzhydrocodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Bosutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bosutinib. Avoid combination
Brigatinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inducers when possible. If combined, increase the daily dose of brigatinib in 30 mg increments after 7 days of treatment with the current brigatinib dose, up to maximum of twice the dose. Consider therapy modification
Clarithromycin: Bosentan may increase serum concentrations of the active metabolite(s) of Clarithromycin. Specifically, bosentan may increase concentrations of 14-hydroxyclarithromycin. Bosentan may decrease the serum concentration of Clarithromycin. Clarithromycin may increase the serum concentration of Bosentan. Management: Consider alternative antimicrobial if possible. The clinical activity of clarithromycin may be altered, and increased bosentan toxicity may be expected. Consider therapy modification
CloZAPine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Cobicistat: May increase the serum concentration of Bosentan. Management: See full drug interaction monograph for details. Consider therapy modification
Cobimetinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
CycloSPORINE (Systemic): May increase the serum concentration of Bosentan. Bosentan may decrease the serum concentration of CycloSPORINE (Systemic). Avoid combination
CYP2C9 Inhibitors (Moderate): May increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Exceptions: Letermovir. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
CYP3A4 Substrates (High risk with Inducers): Bosentan may decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Daclatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Daclatasvir. Management: Increase the daclatasvir dose to 90 mg once daily if used with a moderate CYP3A4 inducer. Consider therapy modification
Darunavir: Bosentan may decrease the serum concentration of Darunavir. Darunavir may increase the serum concentration of Bosentan. Management: Use bosentan 62.5 mg/day or every other day in adults taking ritonavir- or cobicistat-boosted darunavir for at least 10 days. Stop bosentan for at least 36 hrs before starting boosted darunavir; wait at least 10 days before restarting bosentan. Consider therapy modification
Dasabuvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Dasabuvir. Avoid combination
Deflazacort: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Doravirine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Doravirine. Monitor therapy
Elbasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Monitor therapy
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Encorafenib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Encorafenib. Avoid combination
Entrectinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Entrectinib. Avoid combination
Erdafitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Erdafitinib. Management: Dose modifications of erdafitinib may be required. See full monograph for details. Consider therapy modification
Estriol (Systemic): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Bosentan may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Use an alternative (i.e., non-hormonal) means of contraception for all women of childbearing potential who are using bosentan, and do not rely on hormonal contraceptives alone. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inducers (Moderate) may decrease the serum concentration of FentaNYL. Monitor therapy
Flibanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Flibanserin. Avoid combination
Fosamprenavir: Bosentan may decrease the serum concentration of Fosamprenavir. Fosamprenavir may increase the serum concentration of Bosentan. Management: Use bosentan 62.5 mg/day or every other day in adult patients taking fosamprenavir for at least 10 days. Temporarily stop bosentan (for at least 36 hrs) before starting fosamprenavir; wait at least 10 days before restarting bosentan. Consider therapy modification
Gemfibrozil: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. See separate drug interaction monographs for agents listed as exceptions. Monitor therapy
Glecaprevir and Pibrentasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
GlyBURIDE: May enhance the hepatotoxic effect of Bosentan. GlyBURIDE may decrease the serum concentration of Bosentan. Bosentan may decrease the serum concentration of GlyBURIDE. Avoid combination
Grazoprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Grazoprevir. Avoid combination
GuanFACINE: CYP3A4 Inducers (Moderate) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a moderate CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating a moderate CYP3A4 inducer in a patient already taking guanfacine. Consider therapy modification
HYDROcodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ibrutinib. Monitor therapy
Ifosfamide: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Indinavir: May increase the serum concentration of Bosentan. Bosentan may decrease the serum concentration of Indinavir. Management: Initiate bosentan at, or adjust bosentan to, 62.5 mg once daily or every other day (based on tolerability) in indinavir-treated patients (see ritonavir for dosing if that agent is used). Additionally, monitor for possible reduced response to indinavir. Consider therapy modification
Istradefylline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Istradefylline. Monitor therapy
Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ivacaftor. Monitor therapy
Lefamulin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: Bosentan may decrease the serum concentration of Letermovir. Avoid combination
Lopinavir: May increase the serum concentration of Bosentan. Bosentan may decrease the serum concentration of Lopinavir. Management: Use bosentan 62.5 mg/day or every other day in adult patients taking lopinavir/ritonavir for at least 10 days. Temporarily stop bosentan (for at least 36 hrs) before starting lopinavir/ritonavir; wait at least 10 days before restarting bosentan. Consider therapy modification
Lorlatinib: CYP3A4 Inducers (Moderate) may enhance the hepatotoxic effect of Lorlatinib. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with moderate CYP3A4 inducers. If such a combination must be used, monitor AST, ALT, and bilirubin within 48 hours of starting the combination and at least three times within the first week of combined use. Consider therapy modification
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumacaftor and Ivacaftor. Monitor therapy
Lumateperone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lurasidone. Management: Monitor for decreased lurasidone effects if combined with moderate CYP3A4 inducers and consider increasing the lurasidone dose if coadministered with a moderate CYP3A4 inducer for 7 or more days. Consider therapy modification
Macimorelin: Bosentan may diminish the diagnostic effect of Macimorelin. Monitor therapy
Meperidine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Meperidine. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Mirodenafil. Monitor therapy
Naldemedine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Naldemedine. Monitor therapy
Nelfinavir: May increase the serum concentration of Bosentan. Bosentan may decrease the serum concentration of Nelfinavir. Management: Initiate bosentan at, or adjust bosentan dose to, 62.5 mg once daily or every other day (based on tolerability) in patients who receive nelfinavir. Additionally, monitor for possible reduced clinical response to nelfinavir. Consider therapy modification
Neratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Neratinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of NiMODipine. Monitor therapy
Nisoldipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Olaparib. Avoid combination
Palbociclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Palbociclib. Management: The US label does not provide specific recommendations concerning use with moderate CYP3A4 inducers, but the Canadian label recommends avoiding use of moderate CYP3A4 inducers. Consider therapy modification
Perampanel: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pexidartinib. Monitor therapy
Phosphodiesterase 5 Inhibitors: Bosentan may decrease the serum concentration of Phosphodiesterase 5 Inhibitors. Phosphodiesterase 5 Inhibitors may increase the serum concentration of Bosentan. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pimavanserin. Avoid combination
Pitolisant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pitolisant. Monitor therapy
Pretomanid: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pretomanid. Avoid combination
Progestins (Contraceptive): Bosentan may decrease the serum concentration of Progestins (Contraceptive). Management: Use an alternative (i.e., non-hormonal) means of contraception for all women of childbearing potential who are using bosentan, and do not rely on hormonal contraceptives alone. Consider therapy modification
Ranolazine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ranolazine. Avoid combination
RifAMPin: May decrease the serum concentration of Bosentan. Following the initial several weeks of concurrent rifampin, this effect is most likely. RifAMPin may increase the serum concentration of Bosentan. This effect is most likely to be observed within the initial few weeks of concurrent therapy (and may be greatest immediately following initiation of the combination). Management: Weekly monitoring of liver function tests during the first 4 weeks of concurrent therapy is recommended, with a return to normal recommended monitoring thereafter as appropriate. Monitor therapy
Ritonavir: May increase the serum concentration of Bosentan. Management: Use bosentan 62.5 mg daily or every other day in adult patients who have been on ritonavir for at least 10 days. Temporarily stop bosentan (for at least 36 hrs) before starting ritonavir; wait until at least 10 days on ritonavir before restarting. Consider therapy modification
Rolapitant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Rolapitant. Monitor therapy
Saquinavir: Bosentan may decrease the serum concentration of Saquinavir. Saquinavir may increase the serum concentration of Bosentan. Management: Use bosentan 62.5 mg/day or every other day in adult patients taking saquinavir/ritonavir for at least 10 days. Temporarily stop bosentan (for at least 36 hrs) before starting saquinavir/ritonavir; wait at least 10 days before restarting bosentan. Consider therapy modification
Simeprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Simeprevir. Avoid combination
Simvastatin: Bosentan may decrease the serum concentration of Simvastatin. Monitor therapy
Sonidegib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Sonidegib. Avoid combination
Tazemetostat: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tazemetostat. Avoid combination
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tezacaftor and Ivacaftor. Monitor therapy
Tipranavir: Bosentan may decrease the serum concentration of Tipranavir. Tipranavir may increase the serum concentration of Bosentan. Management: Use bosentan 62.5 mg/day or every other day in adult patients taking tipranavir/ritonavir for at least 10 days. Temporarily stop bosentan (for at least 36 hrs) before starting tipranavir/ritonavir; wait at least 10 days before restarting bosentan. Consider therapy modification
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Ubrogepant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a moderate CYP3A4 inducer. Consider therapy modification
Ulipristal: Bosentan may decrease the serum concentration of Ulipristal. Avoid combination
Upadacitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Upadacitinib. Monitor therapy
Velpatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Venetoclax: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Venetoclax. Avoid combination
Vitamin K Antagonists (eg, warfarin): Bosentan may increase the metabolism of Vitamin K Antagonists. Monitor therapy
Voxelotor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and moderate CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zolpidem. Monitor therapy
Adverse Reactions
>10%:
Cardiovascular: Edema (≤11%)
Central nervous system: Headache (15%)
Hepatic: Increased serum ALT (≥3 times ULN: ≤12%; 8 times ULN: ≤2%; dose-related), increased serum AST (≥3 times ULN: ≤12%; 8 times ULN: ≤2%; dose-related)
Respiratory: Respiratory tract infection (22%)
1% to 10%:
Cardiovascular: Chest pain (5%), syncope (5%), flushing (4%), hypotension (4%), palpitations (4%)
Endocrine & metabolic: Fluid retention (≤2%)
Hematologic & oncologic: Anemia (3%)
Neuromuscular & skeletal: Arthralgia (4%)
Respiratory: Sinusitis (4%)
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, DRESS syndrome, hepatic cirrhosis (prolonged therapy), hepatic failure (rare), hypersensitivity reaction, jaundice, leukopenia, nasal congestion, neutropenia, peripheral edema, severe anemia, skin rash, thrombocytopenia
Warnings/Precautions
Concerns related to adverse effects:
- Fluid retention/peripheral edema: Development of peripheral edema due to treatment and/or disease state (pulmonary arterial hypertension) may occur. There have also been postmarketing reports of fluid retention requiring treatment (eg, diuretics, fluid management, hospitalization) for heart failure. If clinically significant fluid retention develops (with or without weight gain), further evaluation is necessary to determine cause and appropriate treatment or discontinuation of therapy. Use with caution in patients with underlying heart failure due to potential complications from fluid retention. In a scientific statement from the American Heart Association, bosentan has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]).
- Hematologic effects: Dose-related decreases in hematocrit/hemoglobin may be observed, usually within the first few weeks of therapy with subsequent stabilization of levels by 4 to 12 weeks of treatment. Monitor hemoglobin prior to treatment initiation, after 1 and 3 months, and every 3 months thereafter. Significant decreases in hemoglobin require further evaluation to determine the cause and specific management.
- Hepatotoxicity: [US Boxed Warning]: Bosentan is associated with transaminase elevations (ALT or AST ≥3 times ULN), and in a small number of cases may occur with elevations in bilirubin. Monitor transaminases at baseline then monthly thereafter. Adjust dosage if elevations in liver enzymes occur without symptoms of hepatic injury or elevated bilirubin. In the postmarketing surveillance (with close monitoring), there have been rare cases of unexplained hepatic cirrhosis after prolonged therapy (>12 months) in patients with multiple comorbidities and drug therapies. There have also been cases of hepatic failure. Treatment should be stopped in patients who develop elevated transaminases either in combination with symptoms of hepatic injury (unusual fatigue, jaundice, nausea, vomiting, abdominal pain, and/or fever) or elevated bilirubin (≥2 times ULN); safety of reintroduction is unknown. Avoid use in patients with baseline serum transaminases >3 times ULN at baseline (monitoring for hepatotoxicity may be more difficult) or moderate to severe hepatic impairment. The combination of hepatocellular injury (transaminase elevations >3 times ULN) and bilirubin increased ≥2 times ULN are a marker for potential serious hepatotoxicity. Transaminase elevations are dose dependent, generally asymptomatic, occur both early and late in therapy, progress slowly, and are usually reversible after treatment interruption or discontinuation. Transaminase elevations may also spontaneously reverse while continuing bosentan treatment. Consider the benefits of treatment versus the risk of hepatotoxicity when initiating therapy in patients with WHO Class II symptoms.
- Hypersensitivity: Hypersensitivity reactions, including Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), anaphylaxis, rash and angioedema have been observed.
- Spermatogenesis: Decreased sperm counts have been observed in men during treatment; bosentan may have an adverse effect on spermatogenesis.
- Pulmonary veno-occlusive disease: If signs of pulmonary edema occur, consider possibility of pulmonary veno-occlusive disease; may require discontinuation of bosentan.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pregnancy: [US Boxed Warning]: Bosentan is likely to cause major birth defects if used by pregnant women based on animal data. Therefore, pregnancy must be excluded before the start of treatment with bosentan. Throughout treatment and for 1 month after stopping bosentan, women of childbearing potential must use 2 reliable methods of contraception unless the patient has an intrauterine device (IUD) or tubal sterilization in which case no other contraception is needed. Hormonal contraceptives, including oral, injectable, transdermal, and implantable contraceptives, should not be used as the sole means of contraception because these may not be effective in patients receiving bosentan. Obtain monthly pregnancy tests.
Dosage form specific issues:
- Aspartame: Some products may contain aspartame, which is metabolized to phenylalanine and must be avoided (or used with caution) in patients with phenylketonuria.
Other warnings/precautions:
- REMS program: [US Boxed Warning]: Because of the risks of hepatotoxicity and birth defects, bosentan is only available through the Bosentan REMS Program. Patients, prescribers, and pharmacies must enroll with the program. Call 1-866-359-2612 or visit www.BosentanREMSProgram.com for more information.
Monitoring Parameters
Serum transaminase (AST and ALT) and bilirubin (prior to treatment initiation and monthly thereafter, or more frequently if clinically necessary [every 2 weeks following transaminase elevations and 3 days after reintroducing therapy if withheld due to transaminase elevations]). Hemoglobin and hematocrit (at baseline, at 1 month and 3 months of treatment, and every 3 months thereafter [generally stabilizes after 4 to 12 weeks of treatment]).
Pregnancy test in women of childbearing potential (prior to the initiation of therapy, monthly during treatment, and one month after stopping bosentan).
Monitor for clinical signs/symptoms of liver injury (eg, abdominal pain, fatigue, fever, jaundice, nausea, vomiting) and fluid retention.
Pregnancy
Pregnancy Considerations
Bosentan is contraindicated in females who are or who may become pregnant.
[US Boxed Warning]: Bosentan is likely to cause major birth defects if used by pregnant women based on animal data. Therefore, pregnancy must be excluded before the start of treatment with bosentan. Throughout treatment and for 1 month after stopping bosentan, women of childbearing potential must use two reliable methods of contraception unless the patient has an intrauterine device (IUD) or tubal sterilization in which case no other contraception is needed. Hormonal contraceptives, including oral, injectable, transdermal, and implantable contraceptives, should not be used as the sole means of contraception because these may not be effective in patients receiving bosentan. Obtain monthly pregnancy tests. When a hormonal or barrier contraceptive is used, one additional method of contraception is still needed if a male partner has had a vasectomy. A missed menses or suspected pregnancy should be reported to a health care provider and prompt immediate pregnancy testing. Sperm counts may be reduced in men during treatment; fertility may be impaired.
Women with pulmonary arterial hypertension (PAH) are encouraged to avoid pregnancy (McLaughlin 2009; Taichman 2014).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure in the lungs.
Frequently reported side effects of this drug
- Headache
- Flushing
- Stuffy nose
- Common cold symptoms
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe loss of strength and energy
- Weight gain
- Trouble breathing
- Swelling
- Severe dizziness
- Passing out
- Abnormal heartbeat
- Joint pain
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.