Boxed Warning
Fluid/electrolyte loss:
Bumetanide is a potent diuretic which, if given in excessive amounts, can lead to a profound diuresis with water and electrolyte depletion. Therefore, careful medical supervision is required and dose and dosage schedule have to be adjusted to the individual patient's needs.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection:
Generic: 0.25 mg/mL (2 mL [DSC], 4 mL, 10 mL)
Tablet, Oral:
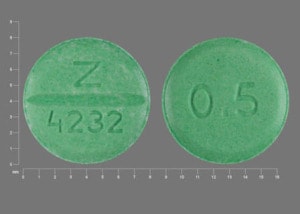
Bumex: 0.5 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
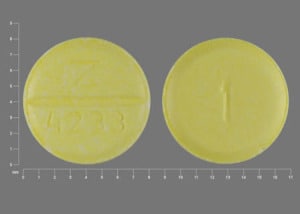
Bumex: 1 mg [contains fd&c yellow #10 (quinoline yellow)]
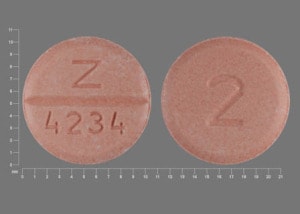
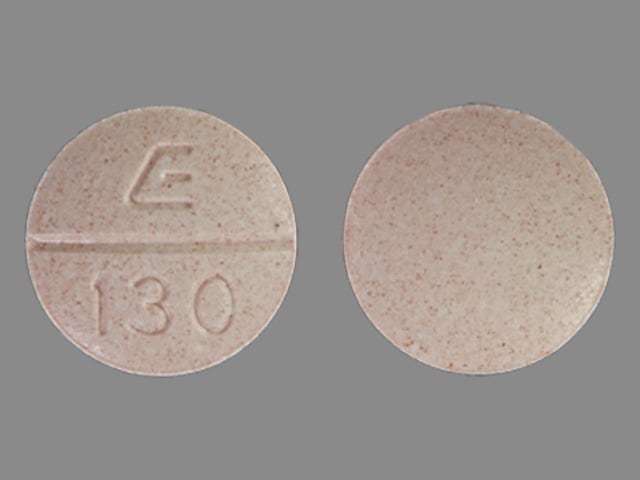
Bumex: 2 mg
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Inhibits reabsorption of sodium and chloride in the ascending loop of Henle and proximal renal tubule, interfering with the chloride-binding cotransport system, thus causing increased excretion of water, sodium, chloride, magnesium, phosphate, and calcium; it does not appear to act on the distal tubule
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: Neonates and Infants: 0.26 to 0.39 L/kg; Adults: 9 to 25 L
Metabolism
Partially hepatic
Excretion
Urine (81% of total dose; 45% of which is unchanged drug); feces (2% of total dose)
Clearance:
Preterm and full term neonates: 0.2 to 1.1 mL/minute/kg
Infants <2 months: 2.17 mL/minute/kg
Infants 2 to 6 months: 3.8 mL/minute/kg
Adults: 2.9 ± 0.2 mL/minute/kg
Onset of Action
Oral, IM: 0.5 to 1 hour; IV: 2 to 3 minutes
Peak effect: Oral: 1 to 2 hours; IV: 15 to 30 minutes
Duration of Action
Oral: 4 to 6 hours; IV: 2 to 3 hours
Half-Life Elimination
Premature and full term neonates: 6 hours (range up to 15 hours)
Infants <2 months: 2.5 hours
Infants 2 to 6 months: 1.5 hours
Adults: 1 to 1.5 hours
Protein Binding
94% to 96%; Neonates: 97%
Use in Specific Populations
Special Populations: Renal Function Impairment
The half-life is prolonged.
Use: Labeled Indications
Edema, heart failure: Management of edema secondary to heart failure or hepatic or renal disease (including nephrotic syndrome)
Use: Off Label
Hypertension (alternative agent)yes
Based on the 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, loop diuretics may be considered as an alternative agent in hypertension and are preferred over thiazides in patients with moderate to severe CKD (eg, GFR <30 mL/minute). Loop diuretics are not recommended for the initial treatment of hypertension.
Contraindications
Hypersensitivity to bumetanide or any component of the formulation; anuria; hepatic coma; patients in states of severe electrolyte depletion until the condition improves or is corrected.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to other sulfonamide derivatives; hepatic encephalopathy; galactose intolerance, glucose-galactose malabsorption, or Lapp lactase deficiency.
Note: Although the product labeling states this medication may be contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Dosage and Administration
Dosing: Adult
Note: Oral dose equivalency (approximate) for patients with normal renal function (Brater 1983; Cody 1994; Vargo 1995): Bumetanide 1 mg = torsemide 20 mg = furosemide 40 mg = ethacrynic acid 50 mg
Edema, heart failure:
Oral: Initial: 0.5 to 2 mg/dose 1 to 2 times daily; if diuretic response to initial dose is not adequate, may repeat in 4 to 5 hours for up to 2 doses (maximum dose: 10 mg/day). ACCF/AHA 2013 heart failure guidelines recommend initial dosing of 0.5 to 1 mg once or twice daily and a maximum total daily dose of 10 mg (Yancy 2013).
IM, IV: 0.5 to 1 mg/dose; if diuretic response to initial dose is not adequate, may repeat in 2 to 3 hours for up to 2 doses (maximum dose: 10 mg/day)
Continuous IV infusion (off-label dose): Initial: 1 mg IV load then 0.5 to 2 mg/hour; repeat loading dose before increasing infusion rate (ACCF/AHA [Yancy 2013]; Brater 1998). Note: With lower baseline CrCl (eg, CrCl <25 mL/minute), the upper end of the initial infusion dosage range should be considered.
Hypertension (alternative agent) (off-label use): Oral: 0.5 to 2 mg/day in 2 divided doses (ACC/AHA [Whelton 2017])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dose equivalency for adult patients with normal renal function (approximate): Bumetanide 1 mg = furosemide 40 mg = torsemide 20 mg = ethacrynic acid 50 mg
Edema (diuresis):
Intermittent dosing:
Infants and Children: Limited data available: Oral, IM, IV: 0.01 to 0.1 mg/kg/dose every 6 to 24 hours; maximum adult daily dose: 10 mg/day; a prospective, open-label dose-range study in infants (mean age: 2 months; range: 0 to 6 months) reported a maximal diuretic response at doses 0.035 to 0.04 mg/kg/dose every 6 to 8 hours, and no additional clinical benefit (ie, urine output) at doses >0.05 mg/kg/dose (Kliegman 2007; Kliegman 2016; Sullivan 1996)
Adolescents: Very limited data: Oral, IM, IV: Initial: 0.5 to 1 mg/dose every 6 to 24 hours; maximum adult daily dose: 10 mg/day. Note: Dosing in adolescents based on experience in adult patients.
Continuous IV infusion: Limited data available: Infants, Children, and Adolescents ≤16 years: 1 to 10 mcg/kg/hour. Dosing based on retrospective study of 95 patients (median age: 0.2 years, range: 0 to 15.7 years) who received a mean dose of 5.7 mcg/kg/hour (range: 1 to 10 mcg/kg/hour); negative fluid balance was achieved in 76% of patients within 48 hours of initiation; of note, 60% of patients were receiving concomitant intermittent diuretics (McCallister 2015). Another retrospective, descriptive trial reported higher doses in 40 neonates and children (mean age: 1.6 ± 2.6 years); the reported mean initial dose was 30 mcg/kg/hour (range: 1 to 100 mcg/kg/hour) and the mean maximum dose was 50 mcg/kg/hour (range: 3 to 200 mcg/kg/hour); of note, a complete safety analysis is lacking in this trial (Bulkley 2012).
Reconstitution
Parenteral: Intermittent IV infusion: May be diluted in D5W, LR, or NS (Rudy 1991)
Administration
IV: Administer IV slowly, over 1 to 2 minutes.
IM: May administer IM.
Oral: May administer with or without food. An intermittent dose schedule, such as an alternate-day schedule or administering for 3 to 4 days with rest periods of 1 to 2 days in between, may be the most tolerable and effective regimen for the continued control of edema.
Dietary Considerations
May cause potassium loss; potassium supplement or dietary changes may be required.
Storage
IV: Store vials at 15°C to 30°C (59°F to 86°F). Infusion solutions in D5W, NS, or LR should be used within 24 hours after preparation. Light sensitive; discoloration may occur when exposed to light.
Tablet: Store at 15°C to 30°C (59°F to 86°F); protect from light.
Bumetanide Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Allopurinol: Loop Diuretics may enhance the adverse/toxic effect of Allopurinol. Loop Diuretics may increase the serum concentration of Allopurinol. Specifically, Loop Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amikacin (Oral Inhalation): Loop Diuretics may enhance the nephrotoxic effect of Amikacin (Oral Inhalation). Loop Diuretics may enhance the ototoxic effect of Amikacin (Oral Inhalation). Monitor therapy
Aminoglycosides: Loop Diuretics may enhance the adverse/toxic effect of Aminoglycosides. Specifically, nephrotoxicity and ototoxicity. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Loop Diuretics may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Loop Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: May enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Bilastine: Loop Diuretics may enhance the QTc-prolonging effect of Bilastine. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Loop Diuretics. Consider therapy modification
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Canagliflozin: May enhance the hypotensive effect of Loop Diuretics. Management: If canagliflozin is combined with a loop diuretic, monitor for symptoms of intravascular volume depletion and hypotension. Canadian product labeling recommends avoiding the combination of canagliflozin and loop diuretics. Consider therapy modification
Cardiac Glycosides: Loop Diuretics may enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of loop diuretics. Monitor therapy
Cefazedone: May enhance the nephrotoxic effect of Loop Diuretics. Monitor therapy
Cefotiam: Loop Diuretics may enhance the nephrotoxic effect of Cefotiam. Monitor therapy
Cefpirome: Loop Diuretics may enhance the nephrotoxic effect of Cefpirome. Monitor therapy
Ceftizoxime: Loop Diuretics may enhance the nephrotoxic effect of Ceftizoxime. Monitor therapy
Cephalothin: Loop Diuretics may enhance the nephrotoxic effect of Cephalothin. Monitor therapy
Cephradine: May enhance the nephrotoxic effect of Loop Diuretics. Monitor therapy
CISplatin: Loop Diuretics may enhance the nephrotoxic effect of CISplatin. Loop Diuretics may enhance the ototoxic effect of CISplatin. Monitor therapy
Corticosteroids (Orally Inhaled): May enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Corticosteroids (Systemic): May enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
CycloSPORINE (Systemic): May enhance the adverse/toxic effect of Loop Diuretics. Monitor therapy
Desmopressin: Loop Diuretics may enhance the hyponatremic effect of Desmopressin. Avoid combination
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dichlorphenamide: Loop Diuretics may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Dofetilide: Loop Diuretics may enhance the QTc-prolonging effect of Dofetilide. Management: Monitor serum potassium and magnesium more closely when dofetilide is combined with loop diuretics. Some therapy modification may be required. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Empagliflozin: May enhance the hypotensive effect of Loop Diuretics. Monitor therapy
Fexinidazole [INT]: May enhance the arrhythmogenic effect of Loop Diuretics. Avoid combination
Foscarnet: Loop Diuretics may increase the serum concentration of Foscarnet. Consider therapy modification
Fosphenytoin: May diminish the diuretic effect of Loop Diuretics. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ipragliflozin: May enhance the adverse/toxic effect of Loop Diuretics. Specifically, the risk for intravascular volume depletion may be increased. Monitor therapy
Ivabradine: Loop Diuretics may enhance the arrhythmogenic effect of Ivabradine. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levosulpiride: Loop Diuretics may enhance the adverse/toxic effect of Levosulpiride. Avoid combination
Licorice: May enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Lithium: Loop Diuretics may decrease the serum concentration of Lithium. Loop Diuretics may increase the serum concentration of Lithium. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Methotrexate: May diminish the therapeutic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Methotrexate. Methotrexate may increase the serum concentration of Loop Diuretics. Management: Monitor for increased methotrexate and/or loop diuretic levels/toxicity with concomitant use of these agents and monitor for decreased therapeutic effects of loop diuretics. Methotrexate and/or loop diuretic dose reductions may be necessary. Consider therapy modification
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Neuromuscular-Blocking Agents: Loop Diuretics may diminish the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Loop Diuretics may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the diuretic effect of Loop Diuretics. Loop Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Management: Monitor for evidence of kidney injury or decreased therapeutic effects of loop diuretics with concurrent use of an NSAID. Consider avoiding concurrent use in CHF or cirrhosis. Concomitant use of bumetanide with indomethacin is not recommended. Consider therapy modification
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Phenytoin: May diminish the diuretic effect of Loop Diuretics. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Probenecid: May enhance the adverse/toxic effect of Loop Diuretics. Probenecid may diminish the diuretic effect of Loop Diuretics. Probenecid may increase the serum concentration of Loop Diuretics. Management: Monitor for decreased diuretic effects or increased adverse effects of loop diuretics with concomitant use of probenecid. Bumetanide prescribing information recommends against concomitant use of probenecid. Monitor therapy
Promazine: Loop Diuretics may enhance the QTc-prolonging effect of Promazine. Avoid combination
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Reboxetine: May enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
RisperiDONE: Loop Diuretics may enhance the adverse/toxic effect of RisperiDONE. Monitor therapy
Salicylates: May diminish the diuretic effect of Loop Diuretics. Loop Diuretics may increase the serum concentration of Salicylates. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Tobramycin (Oral Inhalation): Loop Diuretics may enhance the nephrotoxic effect of Tobramycin (Oral Inhalation). Loop Diuretics may enhance the ototoxic effect of Tobramycin (Oral Inhalation). Monitor therapy
Topiramate: Loop Diuretics may enhance the hypokalemic effect of Topiramate. Monitor therapy
Xipamide: May enhance the adverse/toxic effect of Loop Diuretics. Specifically, the risk of hypovolemia, electrolyte disturbances, and prerenal azotemia may be increased. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016).
Adverse Reactions
>10%:
Endocrine & metabolic: Hyperuricemia (18%), hypochloremia (15%), hypokalemia (15%)
Genitourinary: Azotemia (11%)
1% to 10%:
Central nervous system: Dizziness (1%)
Endocrine & metabolic: Hyponatremia (9%), hyperglycemia (7%), phosphorus change (5%), variations in bicarbonate (3%), abnormal serum calcium (2%), abnormal lactate dehydrogenase (1%)
Neuromuscular & skeletal: Muscle cramps (1%)
Renal: Increased serum creatinine (7%)
Respiratory: Variations in CO2 content (4%)
<1%, postmarketing, and/or case reports: Abdominal pain, abnormal alkaline phosphatase, abnormal bilirubin levels, abnormal hematocrit, abnormal hemoglobin level, abnormal transaminase, arthritic pain, asterixis, auditory impairment, blood cholesterol abnormal, brain disease (in patients with preexisting liver disease), change in creatinine clearance, change in prothrombin time, change in WBC count, chest pain, dehydration, diaphoresis, diarrhea, dyspepsia, ECG changes, erectile dysfunction, fatigue, glycosuria, headache, hyperventilation, hypotension, musculoskeletal pain, nausea, nipple tenderness, orthostatic hypotension, otalgia, ototoxicity, premature ejaculation, proteinuria, pruritus, renal failure, skin rash, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis, urticaria, vertigo, vomiting, weakness, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Fluid/electrolyte loss: [US Boxed Warning]: Loop diuretics are potent diuretics; excess amounts can lead to profound diuresis with fluid and electrolyte loss; close medical supervision and dose evaluation are required. Potassium supplementation and/or use of potassium-sparing diuretics may be necessary to prevent hypokalemia. In contrast to thiazide diuretics, a loop diuretic can also lower serum calcium concentrations. Electrolyte disturbances can predispose a patient to serious cardiac arrhythmias.
- Hyperuricemia: Asymptomatic hyperuricemia has been reported with use.
- Nephrotoxicity: Monitor fluid status and renal function in an attempt to prevent oliguria, azotemia, and reversible increases in BUN and creatinine; close medical supervision of aggressive diuresis required.
- Ototoxicity: Bumetanide-induced ototoxicity (usually transient) may occur with rapid IV administration, renal impairment, excessive doses, and concurrent use of other ototoxins (eg, aminoglycosides).
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Bariatric surgery: Dehydration: Avoid diuretics in the immediate postoperative period after bariatric surgery; electrolyte disturbances and dehydration may occur. Diuretics may be resumed, if indicated, once oral fluid intake goals are met (Ziegler 2009).
- Hepatic impairment: Use caution in patients with cirrhosis; initiate bumetanide therapy with conservative dosing and close monitoring of electrolytes; avoid sudden changes in fluid and electrolyte balance and acid/base status which may lead to hepatic encephalopathy.
- Renal impairment: Larger doses may be necessary in patients with impaired renal function to obtain the same therapeutic response (Brater 1998).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Neonates: In vitro studies using pooled sera from critically-ill neonates have shown bumetanide to be a potent displacer of bilirubin; avoid use in neonates at risk for kernicterus.
- Surgical patients: If given the morning of surgery, bumetanide may render the patient volume depleted and blood pressure may be labile during general anesthesia.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer’s labeling.
Other warnings and precautions:
- Diuretic resistance: For some patients, despite higher doses of loop diuretic treatment, an adequate diuretic response cannot be attained. Diuretic resistance can usually be overcome by intravenous administration, the use of two diuretics together (eg, furosemide and chlorothiazide), or the use of a diuretic with a positive inotropic agent. When such combinations are used, serum electrolytes need to be monitored even more closely (ACC/AHA [Yancy 2013]; HFSA 2010).
Monitoring Parameters
Blood pressure; serum electrolytes, renal function; fluid status (weight and I & O)
Pregnancy
Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to get rid of extra fluid.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, nausea or vomiting.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Chest pain
- Shortness of breath
- Coughing up blood
- Severe dizziness
- Passing out
- Trouble hearing
- Bruising
- Bleeding
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.