Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Film, Buccal:
Bunavail: Buprenorphine 6.3 mg and naloxone 1 mg (1 ea, 30 ea); Buprenorphine 2.1 mg and naloxone 0.3 mg (1 ea, 30 ea); Buprenorphine 4.2 mg and naloxone 0.7 mg (1 ea, 30 ea) [contains brilliant blue fcf (fd&c blue #1), methylparaben, propylparaben, saccharin sodium, sodium benzoate]
Film, Sublingual:
Suboxone: Buprenorphine 4 mg and naloxone 1 mg (1 ea, 30 ea); Buprenorphine 8 mg and naloxone 2 mg (1 ea, 30 ea); Buprenorphine 12 mg and naloxone 3 mg (1 ea, 30 ea); Buprenorphine 2 mg and naloxone 0.5 mg (1 ea, 30 ea) [contains fd&c yellow #6 (sunset yellow); lime flavor]
Generic: Buprenorphine 12 mg and naloxone 3 mg (1 ea, 30 ea); Buprenorphine 2 mg and naloxone 0.5 mg (1 ea, 30 ea); Buprenorphine 4 mg and naloxone 1 mg (1 ea, 30 ea); Buprenorphine 8 mg and naloxone 2 mg (1 ea, 30 ea)
Tablet Sublingual, Sublingual:
Zubsolv: Buprenorphine 5.7 mg and naloxone 1.4 mg, Buprenorphine 8.6 mg and naloxone 2.1 mg, Buprenorphine 0.7 mg and naloxone 0.18 mg, Buprenorphine 1.4 mg and naloxone 0.36 mg, Buprenorphine 11.4 mg and naloxone 2.9 mg, Buprenorphine 2.9 mg and naloxone 0.71 mg [contains menthol; menthol flavor]
Generic: Buprenorphine 2 mg and naloxone 0.5 mg, Buprenorphine 8 mg and naloxone 2 mg
Pharmacology
Mechanism of Action
Buprenorphine: Buprenorphine exerts its analgesic effect via high affinity binding to mu opiate receptors in the CNS; displays partial mu agonist and weak kappa antagonist activity
Naloxone: Pure opioid antagonist that competes and displaces opioids at opioid receptor sites
Pharmacokinetics/Pharmacodynamics
Absorption
Absorption widely is variable among patients following sublingual and buccal use, but variability within each individual patient is low.
Half-Life Elimination
Suboxone: Buprenorphine 24 to 42 hours; Naloxone 2 to 12 hours; Bunavail: Buprenorphine 16.4 to 27.5 hours; Naloxone 1.9 to 2.4 hours; Cassipa: Buprenorphine 35 to 37 hours; Naloxone 5.6 to 6.6 hours
Protein Binding
Buprenorphine: ~96%, primarily to alpha and beta globulin; Naloxone: ~45%, primarily to albumin
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Because both drugs are extensively metabolized, the plasma levels will be expected to be higher and the half-life values have been shown to be longer in patients with moderate and severe hepatic impairment; the significance of the effects are greater for naloxone compared to buprenorphine and for patients with severe hepatic impairment compared to patients with moderate hepatic impairment.
Use: Labeled Indications
Opioid dependence: Treatment of opioid dependence.
General information: Buprenorphine/naloxone should be used as part of a complete treatment plan to include counseling and psychosocial support.
Contraindications
Hypersensitivity (eg, anaphylactic shock) to buprenorphine, naloxone, or any component of the formulation.
Documentation of allergenic cross-reactivity for opioids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling (sublingual tablets): Additional contraindications (not in US labeling): Opioid-naive patients; severe respiratory insufficiency (eg, acute or severe bronchial asthma, chronic obstructive airway, status asthmaticus, acute respiratory depression, cor pulmonale); severe hepatic impairment; acute alcoholism or delirium tremens; convulsive or seizure disorders; known or suspected mechanical GI obstruction or diseases/conditions that affect bowel transit (eg, ileus of any type); suspected surgical abdomen (eg, acute appendicitis or pancreatitis); severe CNS depression, increased cerebrospinal or intracranial pressure, or head injury; concurrent use or within 2 weeks of MAO inhibitors.
Dosage and Administration
Dosing: Adult
Opioid dependence:
US labeling:
Induction: Heroin or other short-acting opioid dependency:
Notes:
Buprenorphine/naloxone is not recommended for use during the induction period for long-acting opioids or methadone; initial treatment should begin using buprenorphine monotherapy under supervision. Patients should be switched to the combination product for maintenance and unsupervised therapy.
Initiate treatment with buccal or sublingual buprenorphine/naloxone or sublingual buprenorphine monotherapy during the induction period for short-acting opioids or heroin; initiate treatment only when signs of moderate opioid withdrawal appear and not less than 6 hours after last opioid use. Titrate to adequate maintenance dose as rapidly as possible based on control of acute withdrawal symptoms.
Buccal film (Bunavail: Buprenorphine 2.1 mg/naloxone 0.3 mg; buprenorphine 4.2 mg/naloxone 0.7 mg; buprenorphine 6.3 mg/naloxone 1 mg):
Day 1 induction dose: Initial: Buccal: Buprenorphine 2.1 mg/naloxone 0.3 mg; may repeat dose after ~2 hours, based on control of acute withdrawal symptoms; maximum total dose: buprenorphine 4.2 mg/naloxone 0.7 mg.
Day 2 induction dose: Up to buprenorphine 8.4 mg/naloxone 1.4 mg as a single dose.
Sublingual film (Suboxone: Buprenorphine 2 mg/naloxone 0.5 mg; buprenorphine 4 mg/naloxone 1 mg; buprenorphine 8 mg/naloxone 2 mg; buprenorphine 12 mg/naloxone 3 mg):
Day 1 induction dose: Initial: Sublingual: Buprenorphine 2 mg/naloxone 0.5 mg or buprenorphine 4 mg/naloxone 1 mg; may titrate dose, based on control of acute withdrawal symptoms, in buprenorphine 2 mg/naloxone 0.5 mg or buprenorphine 4 mg/naloxone 1 mg increments approximately every 2 hours up to a total dose of buprenorphine 8 mg/naloxone 2 mg.
Day 2 induction dose: Sublingual: Up to buprenorphine 16 mg/naloxone 4 mg as a single dose
Sublingual tablet (Zubsolv: Buprenorphine 0.7 mg/naloxone 0.18 mg, buprenorphine 1.4 mg/naloxone 0.36 mg, buprenorphine 2.9 mg/naloxone 0.71 mg, buprenorphine 5.7 mg/naloxone 1.4 mg, buprenorphine 8.6 mg/naloxone 2.1 mg, or buprenorphine 11.4 mg/naloxone 2.9 mg):
Day 1 induction dose: Sublingual: Start with an initial dose of buprenorphine 1.4 mg/naloxone 0.36 mg; based on control of acute withdrawal symptoms, may administer additional doses in increments of 1 to 2 buprenorphine 1.4 mg/naloxone 0.36 mg tablets every 1.5 to 2 hours to a total day 1 dose up to buprenorphine 5.7 mg/naloxone 1.4 mg. Some patients (eg, those with recent exposure to buprenorphine) may tolerate up to buprenorphine 4.2 mg/naloxone 1.08 mg as a single, second dose.
Day 2 induction dose: Sublingual: Up to buprenorphine 11.4 mg/naloxone 2.9 mg as a single dose
Maintenance:
Buccal film (Bunavail: Buprenorphine 2.1 mg/naloxone 0.3 mg, buprenorphine 4.2 mg/naloxone 0.7 mg, buprenorphine 6.3 mg/naloxone 1 mg): Buccal: Target dose: Buprenorphine 8.4 mg/naloxone 1.4 mg once daily; dosage should be adjusted in increments/decrements of buprenorphine 2.1 mg/naloxone 0.3 mg to a level that maintains treatment and suppresses opioid withdrawal symptoms; usual range: Buprenorphine 2.1 to 12.6 mg/naloxone 0.3 to 2.1 mg once daily.
Sublingual film (Suboxone: Buprenorphine 2 mg/naloxone 0.5 mg; buprenorphine 4 mg/naloxone 1 mg; buprenorphine 8 mg/naloxone 2 mg; buprenorphine 12 mg/naloxone 3 mg): Sublingual or buccal: Target dose: Buprenorphine 16 mg/naloxone 4 mg once daily; dosage should be adjusted in increments/decrements of buprenorphine 2 mg/naloxone 0.5 mg or buprenorphine 4 mg/naloxone 1 mg to a level that maintains treatment and suppresses opioid withdrawal symptoms; usual range: Buprenorphine 4 to 24 mg/naloxone 1 to 6 mg once daily.
Sublingual film (Cassipa: Buprenorphine 16 mg/naloxone 4 mg): Sublingual: Buprenorphine 16 mg/naloxone 4 mg once daily; dosage should be adjusted to a level that maintains treatment and suppresses opioid withdrawal symptoms. Note: Buprenorphine 16 mg/naloxone 4 mg sublingual film is only for use following titration from lower doses.
Sublingual tablet (buprenorphine 2 mg/naloxone 0.5 mg or buprenorphine 8 mg/naloxone 2 mg): Sublingual: Target dose: Buprenorphine 16 mg/naloxone 4 mg once daily; dosage should be adjusted in increments/decrements of buprenorphine 2 mg/naloxone 0.5 mg or buprenorphine 4 mg/naloxone 1 mg to a level that maintains treatment and suppresses opioid withdrawal symptoms; usual range: Buprenorphine 4 to 24 mg/naloxone 1 to 6 mg once daily. Doses higher than buprenorphine 24 mg/naloxone 6 mg have not been demonstrated to provide any clinical advantage.
Sublingual tablet (Zubsolv: Buprenorphine 0.7 mg/naloxone 0.18 mg, buprenorphine 1.4 mg/naloxone 0.36 mg, buprenorphine 2.9 mg/naloxone 0.71 mg, buprenorphine 5.7 mg/naloxone 1.4 mg, buprenorphine 8.6 mg/naloxone 2.1 mg, or buprenorphine 11.4 mg/naloxone 2.9 mg): Sublingual: Target dose: Buprenorphine 11.4 mg/naloxone 2.9 mg once daily; dosage should be adjusted in increments/decrements of buprenorphine 2.9 mg/naloxone 0.71 mg or lower to a level that maintains treatment and suppresses opioid withdrawal symptoms; usual range: Buprenorphine 2.9 to 17.2 mg/naloxone 0.71 to 4.2 mg once daily. Doses higher than buprenorphine 17.2 mg/naloxone 4.2 mg have not been demonstrated to provide any clinical advantage.
Off-label dosing recommendations (US Department of Health and Human Services, 2004): Doses provided based on buprenorphine content.
Induction (only administer combination product for induction in patients who are dependent on short-acting opioids and whose last dose of opioids was >12 to 24 hours prior to induction):
Day 1 induction dose: Initial: 4 mg; may repeat dose after >2 hours if withdrawal symptoms not relieved; maximum daily dose on day 1: 8 mg daily.
Day 2 induction dose: Previous dose from day 1 if no withdrawal symptoms present; if symptoms of withdrawal present, increase day 1 dose by 4 mg. If withdrawal symptoms not relieved after >2 hours, may administer 4 mg; maximum daily dose on day 2: 16 mg daily.
Subsequent induction days: If withdrawal symptoms are not present, daily dose is established. If withdrawal symptoms are present, increase dose in increments of 2 mg or 4 mg each day as needed for symptom relief. Target daily dose by the end of the first week: 12 mg or 16 mg daily; maximum daily dose: 32 mg daily.
Stabilization: Usual dose: 16 to 24 mg daily; maximum dose: 32 mg daily.
Switching between sublingual tablets and sublingual film: Same dosage should be used as the previous administered product. Note: Potential for greater bioavailability with certain sublingual film strengths compared to the same strength of the sublingual tablet; monitor closely for either over- or underdosing when switching patients from one formulation to another.
Switching between buccal film and sublingual tablets or films: Due to differences in the bioavailability of Bunavail buccal films compared to other buprenorphine/naloxone sublingual tablets, different strengths must be given to achieve equivalent doses. When switching between Bunavail and other sublingual tablets, corresponding dosage strengths are as follows:
Bunavail buprenorphine 2.1 mg/naloxone 0.3 mg = buprenorphine 4 mg/naloxone 1 mg sublingual tablets or films
Bunavail buprenorphine 4.2 mg/naloxone 0.7 mg = buprenorphine 8 mg/naloxone 2 mg sublingual tablets or films
Bunavail buprenorphine 6.3 mg/naloxone 1 mg = buprenorphine 12 mg/naloxone 3 mg sublingual tablets or films
Switching between sublingual film strengths:
Systemic exposure may be different with various combinations of sublingual film strengths; pharmacists should not substitute one or more film strengths for another (eg, switching from three buprenorphine 4 mg/naloxone 1 mg films to a single buprenorphine 12 mg/naloxone 3 mg film, or vice-versa) without health care provider approval, and patients should be monitored closely for either over- or underdosing when switching between film strengths.
Cassipa: Patients may switch from two buprenorphine 8 mg/naloxone 2 mg sublingual films to a single buprenorphine 16 mg/ naloxone 4 mg sublingual film.
Switching between sublingual and buccal sites of administration (Suboxone): Systemic exposure between buccal and sublingual administration of buprenorphine/naloxone sublingual film is similar. Once induction is complete, patients can switch between buccal and sublingual administration without significant risk of under or overdosing.
Switching between sublingual tablet products: Due to differences in the bioavailability of Zubsolv sublingual tablets compared to other buprenorphine/naloxone sublingual tablets, different strengths must be given to achieve equivalent doses. When switching between Zubsolv and other sublingual tablets, corresponding dosage strengths are as follows:
Zubsolv buprenorphine 1.4 mg/naloxone 0.36 mg sublingual tablets = buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets
Zubsolv buprenorphine 2.9 mg/naloxone 0.71 mg sublingual tablets = buprenorphine 4 mg/naloxone 1 mg (as two buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets)
Zubsolv buprenorphine 5.7 mg/naloxone 1.4 mg sublingual tablets = buprenorphine 8 mg/naloxone 2 mg sublingual tablets
Zubsolv buprenorphine 8.6 mg/naloxone 2.1 mg sublingual tablet = buprenorphine 12 mg/naloxone 3 mg sublingual tablets (as one buprenorphine 8 mg/naloxone 2 mg sublingual tablets and two buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets)
Zubsolv buprenorphine 11.4 mg/naloxone 2.9 mg sublingual tablet = buprenorphine 16 mg/naloxone 4 mg sublingual tablets (as two buprenorphine 8 mg/naloxone 2 mg sublingual tablets)
Canadian labeling: Sublingual tablet: Note: Dose based on buprenorphine content. Prior to induction, consider patient's type of dependence (ie, long- or short-acting opiate), time since last use of opiate and extent of dependence. Initiate buprenorphine/naloxone only when early signs of opiate withdrawal appear but no sooner than 6 hours after the last use of heroin or other short-acting opiates. Patients on methadone should have their methadone maintenance dose reduced to the minimum tolerable dose; initiate buprenorphine/naloxone only when early signs of withdrawal appear but no sooner than 24 hours after the last methadone dose.
Induction: Day 1: Initial: 4 mg as single dose; may repeat dose if necessary depending on patient's requirement; target dose: 8 to 12 mg.
Maintenance: Day 2 and beyond: Titrate per response in increments or decrements of 2 to 8 mg; usual maintenance dose: 12 to 16 mg once daily (maximum: 24 mg/day). Upon stabilization, may consider less frequent administration of corresponding equivalent dose (eg, 16 mg every other day instead of 8 mg/day or 3 times/week dosing [eg, Monday-Wednesday-Friday] with twice the maintenance dose on Monday and Wednesday and three times the maintenance dose on Friday); continue to limit maximum dose to 24 mg/day on any single day. Note: When switching dosing to less than once daily, monitor all patients for at least 90 minutes following the initial dose of the new regimen. The less frequent dosing regimen is not recommended in patients dependent on concurrent CNS-active drugs, including ethanol.
Missed doses: Reassess patients who have missed multiple doses; initial induction doses may be required when resuming therapy.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Sublingual tablets and film contain a free-base ratio of buprenorphine:naloxone of 4:1. Not all sublingual dosage forms are bioequivalent and dosing adjustment or additional monitoring may be necessary when switching products; refer to specific dosing sections below. Doses based on buprenorphine content; titrate to appropriate effect.
Opioid dependence, maintenance treatment (heroin or short-acting opioid) (ASAM [Kampman 2015]): Note: Buprenorphine alone (without naloxone) is preferred over the combination product for use during the induction period for long-acting opioids or methadone.
Adolescents: Limited data available: Sublingual: Tablets or Film:
Induction: Note: Combination products should only be administered for induction in patients dependent on short-acting opioids (eg, heroin, oxycodone) who have begun to show mild to moderate opioid withdrawal signs (to avoid precipitated withdrawal) and whose last dose of opioids was at least 6 to 12 hours prior to induction.
Initial: 2 to 4 mg; if no signs of precipitated withdrawal after 60 to 90 minutes, may increase in increments of 2 to 4 mg. Once initial dose is tolerated, may increase to a dose that is clinically effective and provides 24 hours of stabilization.
After induction and titration, daily doses usually ≥8 mg/day are necessary. In patients continuing to use opioids, consider increasing the dose by 4 to 8 mg to a daily dose of 12 to 16 mg/day. Maximum daily dose: 24 mg/day.
Switching between sublingual tablets and sublingual film: The same dosage should be used as the previous administered product with close patient monitoring. Note: Potential for greater bioavailability with certain sublingual film strengths compared to the same strength of the sublingual tablet; monitor closely for either over- or underdosing when switching patients from one formulation to another (ASAM [Kampman 2015]).
Switching between sublingual film strengths: Systemic exposure may be different with various combinations of sublingual film strengths; pharmacists should not substitute one or more film strengths for another (eg, switching from three buprenorphine 4 mg/naloxone 1 mg films to a single buprenorphine 12 mg/naloxone 3 mg film, or vice-versa) without health care provider approval, and patients should be monitored closely for either over- or underdosing when switching between film strengths.
Cassipa: Patients may switch from two buprenorphine 8 mg/naloxone 2 mg sublingual films to a single buprenorphine 16 mg/ naloxone 4 mg sublingual Cassipa film.
Switching between sublingual tablet products: Due to differences in the bioavailability of Zubsolv sublingual tablets compared to other buprenorphine/naloxone sublingual tablets, different strengths must be given to achieve equivalent doses. When switching between Zubsolv and other sublingual tablets, corresponding dosage strengths are as follows:
Zubsolv buprenorphine 1.4 mg/naloxone 0.36 mg sublingual tablets = buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets.
Zubsolv buprenorphine 2.9 mg/naloxone 0.71 mg sublingual tablets = buprenorphine 4 mg/naloxone 1 mg (as two buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets).
Zubsolv buprenorphine 5.7 mg/naloxone 1.4 mg sublingual tablets = buprenorphine 8 mg/naloxone 2 mg sublingual tablets.
Zubsolv buprenorphine 8.6 mg/naloxone 2.1 mg sublingual tablet = buprenorphine 12 mg/naloxone 3 mg sublingual tablets (as one buprenorphine 8 mg/naloxone 2 mg sublingual tablets and two buprenorphine 2 mg/naloxone 0.5 mg sublingual tablets).
Zubsolv buprenorphine 11.4 mg/naloxone 2.9 mg sublingual tablet = buprenorphine 16 mg/naloxone 4 mg sublingual tablets (as two buprenorphine 8 mg/naloxone 2 mg sublingual tablets).
Administration
Film:
Bunavail: Buccal: Although the manufacturer recommends administering the film whole without cutting, chewing, or swallowing, one stability study (using Suboxone brand) suggested that films split in half have uniform content and maintain stability for up to 7 days (Reindel 2019). Immediately before placing the film, moisten inside of cheek with tongue or water. Apply film with a dry finger immediately after removing it from packaging. Place film with the text (BN2, BN4, or BN6) against the inside of the moistened cheek; press and hold the film in place for 5 seconds with finger (film should stay in place after this period). Keep film in place until it dissolves completely. Do not chew, swallow or move film after placement. Liquids and food can be consumed after film dissolves. If using more than 1 film simultaneously, the additional film should be placed on the inside of the other cheek; no more than 2 films should be applied to the inside of one cheek at a time.
Cassipa: Sublingual: Although the manufacturer recommends administering the film whole without cutting, chewing, or swallowing, one stability study (using Suboxone brand) suggested that films split in half have uniform content and maintain stability for up to 7 days (Reindel 2019). Prior to film placement, rinse mouth with a small volume of room temperature water; avoid beverages with a high pH prior to dosing. Place one film under the tongue until the film completely dissolves, close to the base on the left or right side. Do not move film after placement. Liquids and food should not be consumed until after film completely dissolves.
Suboxone: May be used buccally or sublingually.
Buccal: Although the manufacturer recommends administering the film whole without cutting, chewing, or swallowing, one stability study suggested that films split in half have uniform content and maintain stability for up to 7 days (Reindel 2019). Place one film on the inside of the right or left cheek. If more than one film is needed, the additional film should be placed on the inside of the opposite cheek. Keep the film on the inside of the cheek until completely dissolved. Do not move film after placement. If a third film is necessary, place it on the inside of the right or left cheek after the first 2 films have dissolved.
Sublingual film: Although the manufacturer recommends administering the film whole without cutting, chewing, or swallowing, one stability study suggested that films split in half have uniform content and maintain stability for up to 7 days (Reindel 2019). Place one film under the tongue until the film completely dissolves, close to the base on the left or right side. If more than one film is needed, the additional film should be placed under the tongue on the opposite side from the first film. Place the film in a manner to minimize overlapping as much as possible. Do not move film after placement. If a third film is necessary to achieve the prescribed dose, place it under the tongue on either side after the first 2 films have dissolved.
Sublingual tablet: Immediately after removal from blister pack, tablet should be placed under the tongue until dissolved. If 2 or more tablets are needed per dose, all may be placed under the tongue at once, or 2 at a time. In patients requiring more than one sublingual tablet, place all tablets in different places under the tongue at the same time. To ensure consistent bioavailability, subsequent doses should always be taken the same way. Patients should not eat or drink anything until the tablet(s) are completely dissolved. If a sequential mode of administration is preferred, patients should follow the same manner of dosing with continued use of the product, to ensure consistency in bioavailability. Do not chew or swallow sublingual tablets.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from freezing and moisture.
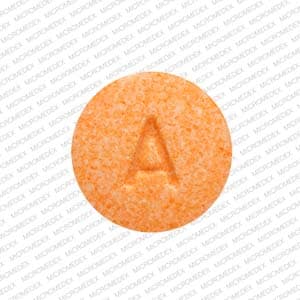
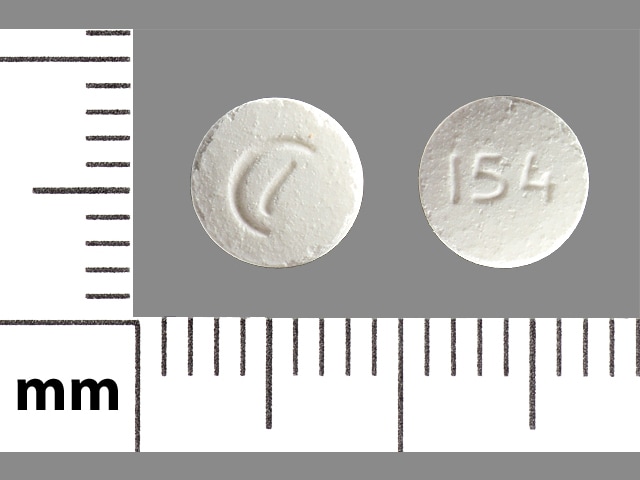
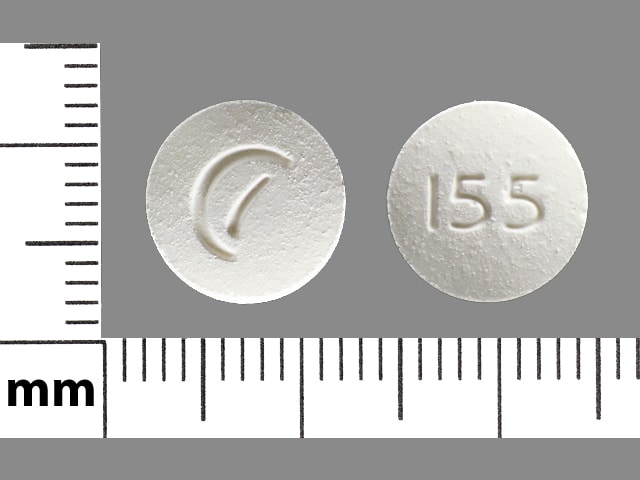
Buprenorphine and Naloxone Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of Buprenorphine. Management: Advise patients receiving buprenorphine about the increased risk of CNS depression if they consume alcohol. Consider alternatives to buprenorphine for opioid addiction treatment in patients who are dependent on alcohol. Consider therapy modification
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alvimopan: Opioid Agonists may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amphetamines: May enhance the analgesic effect of Opioid Agonists. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Atazanavir: Buprenorphine may decrease the serum concentration of Atazanavir. Atazanavir may increase the serum concentration of Buprenorphine. Management: Avoid this combination in patients un-boosted atazanavir due to possible decreased atazanavir concentrations. This combination is not contraindicated in patients also receiving ritonavir, but monitoring for buprenorphine toxicity is recommended. Avoid combination
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cobicistat: May increase the serum concentration of Buprenorphine. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Buprenorphine. Monitor therapy
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Buprenorphine. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May increase the serum concentration of Buprenorphine. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Desmopressin: Opioid Agonists may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Agonists may enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease serum concentrations of the active metabolite(s) of Buprenorphine. Efavirenz may decrease the serum concentration of Buprenorphine. Monitor therapy
Eluxadoline: Opioid Agonists may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Etravirine: May decrease the serum concentration of Buprenorphine. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gastrointestinal Agents (Prokinetic): Opioid Agonists may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylnaltrexone: May enhance the adverse/toxic effect of Opioid Antagonists. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: Buprenorphine may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naldemedine: Opioid Antagonists may enhance the adverse/toxic effect of Naldemedine. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
Nalmefene: May diminish the therapeutic effect of Opioid Agonists. Management: Avoid the concomitant use of nalmefene and opioid agonists. Discontinue nalmefene 1 week prior to any anticipated use of opioid agonistss. If combined, larger doses of opioid agonists will likely be required. Consider therapy modification
Naloxegol: Opioid Antagonists may enhance the adverse/toxic effect of Naloxegol. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
Naltrexone: May diminish the therapeutic effect of Opioid Agonists. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May increase the serum concentration of Buprenorphine. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May increase the serum concentration of Buprenorphine. Monitor therapy
Opioid Agonists: Opioids (Mixed Agonist / Antagonist) may diminish the analgesic effect of Opioid Agonists. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Exceptions: Buprenorphine; Butorphanol; Meptazinol; Nalbuphine; Pentazocine. Avoid combination
Opioids (Mixed Agonist / Antagonist): May diminish the therapeutic effect of Buprenorphine. This combination may also induce opioid withdrawal. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Agonists may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
PHENobarbital: May enhance the CNS depressant effect of Buprenorphine. PHENobarbital may decrease the serum concentration of Buprenorphine. Management: Avoid use of buprenorphine and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased buprenorphine efficacy and withdrawal if combined. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: May enhance the CNS depressant effect of Buprenorphine. Primidone may decrease the serum concentration of Buprenorphine. Management: Avoid use of buprenorphine and primidone when possible. Monitor for respiratory depression/sedation. Because primidone is also a strong CYP3A4 inducer, monitor for decreased buprenorphine efficacy and withdrawal if combined. Consider therapy modification
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Avoid) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ramosetron: Opioid Agonists may enhance the constipating effect of Ramosetron. Monitor therapy
Rifabutin: May decrease the serum concentration of Buprenorphine. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): Opioid Agonists may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Succinylcholine: May enhance the bradycardic effect of Opioid Agonists. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Also see individual agents.
>10%:
Central nervous system: Headache (7% to 37%), pain (22%)
Dermatologic: Diaphoresis (>1% to 14%)
Gastrointestinal: Nausea (sublingual tablet: 5% to 15%), constipation (>1% to 12%), abdominal pain (11%)
1% to 10%:
Cardiovascular: Vasodilation (9%), palpitations (sublingual film: >1%)
Central nervous system: Disturbance in attention (sublingual film: >1%), insomnia (>1%), intoxicated feeling (sublingual film: >1%), withdrawal syndrome (>1%)
Gastrointestinal: Vomiting (5% to 8%), glossalgia (sublingual film: >1%), oral hypoesthesia (sublingual film: >1%), oral mucosa erythema (sublingual film: >1%)
Ophthalmic: Blurred vision (sublingual film: >1%)
Frequency not defined:
Central nervous system: Anxiety, irritability, restlessness
Dermatologic: Piloerection
Gastrointestinal: Stomach discomfort
Neuromuscular & skeletal: Arthralgia
Ophthalmic: Increased lacrimation
Respiratory: Rhinorrhea
<1%, postmarketing, and/or case reports: Glossitis, oral bullae, oral mucosa ulcer, peripheral edema, stomatitis
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Hepatic events: Hepatitis has been reported; hepatic events ranged from transient, asymptomatic transaminase elevations to hepatic failure; in many cases, patients had preexisting hepatic impairment. Monitor liver function tests in patients at increased risk for hepatotoxicity (eg, history of alcohol abuse, preexisting hepatic dysfunction, IV drug abusers) prior to and during therapy.
- Hypersensitivity reactions: Hypersensitivity, including bronchospasm, angioneurotic edema, and anaphylactic shock, have been reported.
- Hypotension: May cause severe hypotension, including orthostatic hypotension and syncope; use with caution in patients with hypovolemia, cardiovascular disease (including acute MI), or drugs that may exaggerate hypotensive effects (including phenothiazines or general anesthetics). Monitor for symptoms of hypotension following initiation or dose titration. Use with caution in patients with circulatory shock.
- Respiratory depression: Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely for respiratory depression, especially during initiation or dose escalation. Misuse by self-injection of buprenorphine or the concomitant use of buprenorphine and benzodiazepines (or other CNS depressants, including alcohol) may result in coma or death. Use with caution in patients with compromised respiratory function (eg, chronic obstructive pulmonary disease, cor pulmonale, decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression).
Disease-related concerns:
- Abdominal conditions: May obscure diagnosis or clinical course of patients with acute abdominal conditions.
- Adrenocortical insufficiency: Use with caution in patients with adrenal insufficiency, including Addison disease. Long-term opioid use may cause secondary hypogonadism, which may lead to sexual dysfunction, infertility, mood disorders, and osteoporosis (Brennan 2013).
- Biliary tract impairment: Use with caution in patients with biliary tract dysfunction, including acute pancreatitis; opioids may cause constriction of sphincter of Oddi.
- Bowel obstruction: Use with caution in patients with a history of ileus or bowel obstruction.
- CNS depression/coma: Use with caution in patients with impaired consciousness or coma because these patients are susceptible to intracranial effects of CO2 retention.
- Delirium tremens: Use with caution in patients with delirium tremens.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure; exaggerated elevation of ICP may occur. Buprenorphine can produce miosis and changes in the level of consciousness that may interfere with patient evaluation.
- Hepatic impairment: Use is not recommended in patients with moderate hepatic impairment for induction therapy (Suboxone) or in patients with severe hepatic impairment. Use with caution in patients with moderate hepatic impairment for maintenance treatment; due to reduced clearance of naloxone and potential for reduced buprenorphine efficacy, use may not be appropriate.
- Obesity: Use with caution in patients who are morbidly obese (DeVido 2015).
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Psychosis: Use with caution in patients with toxic psychosis.
- Respiratory disease: Use with caution and monitor for respiratory depression in patients with significant chronic obstructive pulmonary disease, cor pulmonale, or kyphoscoliosis, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression, particularly when initiating and titrating therapy; critical respiratory depression may occur, even at therapeutic dosages.
- Seizure: Use with caution in patients with a history of seizure disorders; may cause or exacerbate preexisting seizures.
- Sleep-related disorders: Opioid use increases the risk for sleep-related disorders (eg, central sleep apnea [CSA], hypoxemia) in a dose-dependent fashion. Use with caution and titrate dosage cautiously in patients with risk factors for sleep-disordered breathing (eg, heart failure, obesity). Consider dose reduction in patients presenting with CSA. Avoid opioids in patients with moderate to severe sleep-disordered breathing (CDC [Dowell 2016]).
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Benzodiazepines and other CNS depressants: Concomitant use of benzodiazepines or other CNS depressants, including alcohol and opioids, may result in profound sedation, respiratory depression, coma, and death. Prohibiting medication-assisted treatment of opioid use disorder may increase the risk of morbidity and mortality, therefore patients should be educated on the risks of concomitant use with benzodiazepines, sedatives, opioid analgesics, and alcohol. Strategies should be developed to manage use of prescribed or illicit benzodiazepines or other CNS depressants at initiation of or during treatment with buprenorphine; adjustments to induction procedures and additional monitoring may be required. If appropriate, delay or omit buprenorphine dose if a patient is sedated at time of buprenorphine dosing. Discontinuation of benzodiazepines or other CNS depressants is preferred; gradual tapering of benzodiazepine or other CNS depressant, decreasing to lowest effective dose, or monitoring in a higher level of care for taper may be appropriate. Benzodiazepines are not the treatment of choice for anxiety or insomnia for patients in buprenorphine treatment; make sure patients are appropriately diagnosed and consider alternative medications for anxiety and insomnia prior to coadministration of benzodiazepines and buprenorphine.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Cachectic or debilitated patients: Use with caution in cachectic or debilitated patients; there is a greater potential for life-threatening respiratory depression, even at therapeutic dosages.
- Elderly: Use with caution in elderly patients; may be more sensitive to adverse effects (eg, life-threatening respiratory depression).
- Neonates: Neonatal withdrawal syndrome: Prolonged use of opioids during pregnancy can cause neonatal withdrawal syndrome, which may be life-threatening if not recognized and treated according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal withdrawal syndrome and ensure that appropriate treatment will be available. Signs and symptoms include irritability, hyperactivity and abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. Onset, duration, and severity depend on the drug used, duration of use, maternal dose, and rate of drug elimination by the newborn.
Special handling:
- Disposal: Dispose of unused buccal and sublingual films (if they are no longer needed) by removing from foil patch and flushing down the toilet. If multiple films are no longer needed, flush each film individually.
Other warnings/precautions:
- Accidental ingestion: Accidental ingestion in children can result in severe respiratory depression (may be fatal); store buprenorphine-containing medications out of reach of children and dispose of unused medication appropriately.
- Acute pain: When using buprenorphine for treatment of opioid dependence, treat acute pain with nonopioid analgesics whenever possible. If treatment with a high-affinity full opioid analgesic is required, monitor closely for respiratory depression because high doses may be necessary to achieve pain relief.
- Addiction/abuse/misuse: Use exposes patients and other users to the risks of addiction, abuse, and misuse, potentially leading to overdose and death. Assess each patient's risk prior to prescribing; monitor all patients regularly for development of these behaviors or conditions. Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Other factors associated with an increased risk for misuse include younger age and psychotropic medication use. Consider offering naloxone prescriptions in patients with factors associated with an increased risk for overdose, such as history of overdose or substance use disorder, higher opioid dosages (≥50 morphine milligram equivalents/day orally), and concomitant benzodiazepine use (Dowell [CDC 2016]).
- Appropriate use: Buprenorphine/naloxone is not appropriate for pain management; deaths have been reported in opioid-naive patients receiving oral buprenorphine for analgesia.
- Discontinuation of therapy: There is no maximum recommended duration for maintenance treatment of opioid addiction; patients may require treatment indefinitely. Advise patients of the potential to relapse to illicit drug use following discontinuation of opioid agonist/partial agonist medication-assisted treatment.
- Partial opioid agonist and mixed opioid agonist/antagonist overdose: Reversal of partial opioid agonists or mixed opioid agonist/antagonists (eg, buprenorphine, pentazocine) may be incomplete and large doses of naloxone may be required.
- Withdrawal: Concurrent use of opioid agonist/antagonist analgesics may precipitate withdrawal symptoms and/or reduced analgesic efficacy in patients following prolonged therapy with mu opioid agonists. Abrupt discontinuation following prolonged use may also lead to withdrawal symptoms and is not recommended; taper dose gradually when discontinuing. Treatment of opioid dependence with buprenorphine/naloxone should not be started until effects of withdrawal are evident.
Monitoring Parameters
Liver function tests (prior to initiation and periodically during therapy); respiratory and mental status; CNS depression; blood pressure; symptoms of withdrawal; signs of addiction, abuse, or misuse; signs or symptoms of hypogonadism or hypoadrenalism (Brennan 2013).
Pregnancy
Pregnancy Considerations
Buprenorphine and naloxone can be detected in cord blood following maternal use of sublingual tablets; cord blood concentrations of buprenorphine and naloxone correlate with maternal serum levels (Weigand 2016).
Prolonged use of opioids during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure appropriate treatment will be available.
Opioid agonist pharmacotherapy is recommended when treating opioid use disorder in pregnancy; however, use of buprenorphine monotherapy is currently preferred due to limited safety data with the buprenorphine/naloxone combination product (ACOG 711 2017; SAMHSA 2018). Treatment with the combination product should not be initiated during pregnancy (SAMHSA 2018).
Refer to individual monographs for additional information.
Pregnancy testing is recommended prior to initiating therapy for opioid use disorders (SAMHSA 2018). Long-term opioid use may cause infertility in males and females of reproductive potential. Amenorrhea may develop secondary to substance abuse. Initiation of buprenorphine maintenance treatment may improve fertility resulting in unplanned pregnancy. Contraception counseling is recommended (Dow 2012).
Patient Education
What is this drug used for?
- It is used to treat pain drug (opioid) addiction.
- Do not use for pain relief or on an as needed basis.
Frequently reported side effects of this drug
- Loss of strength and energy
- Nausea
- Vomiting
- Headache
- Abdominal pain
- Constipation
- Trouble sleeping
- Sweating a lot
- Flushing
- Back pain
- Burning, numbness or tingling of mouth
- Application site pain or redness
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Withdrawal like excessive sweating, chills, diarrhea, stomach pain, anxiety, irritability, or yawning
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea
- Severe dizziness
- Passing out
- Difficulty breathing
- Slow breathing
- Shallow breathing
- Severe fatigue
- Confusion
- Vision changes
- Change in balance
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Extra muscle movement
- Slow movements
- Slurred speech
- Intoxicated feeling
- Difficulty focusing
- Abnormal heartbeat
- Sexual dysfunction (males)
- No menstrual periods
- Decreased sex drive
- Trouble getting pregnant
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.