Boxed Warning
Neutropenia:
Neutropenic deaths have been reported. Monitor for neutropenia with frequent blood cell counts. Cabazitaxel is contraindicated in patients with neutrophil counts of ≤1,500 cells/mm3. Primary prophylaxis with filgrastim is recommended in patients with high-risk clinical features.
Hypersensitivity:
Severe hypersensitivity reactions can occur and may include generalized rash/erythema, hypotension, and bronchospasm. Severe hypersensitivity reactions require immediate discontinuation of the cabazitaxel infusion and administration of appropriate therapy. Patients should receive premedication. Cabazitaxel is contraindicated in patients who have a history of severe hypersensitivity reactions to cabazitaxel or to other drugs formulated with polysorbate 80.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous:
Jevtana: 60 mg/1.5 mL (1.5 mL) [contains alcohol, usp, polysorbate 80]
Pharmacology
Mechanism of Action
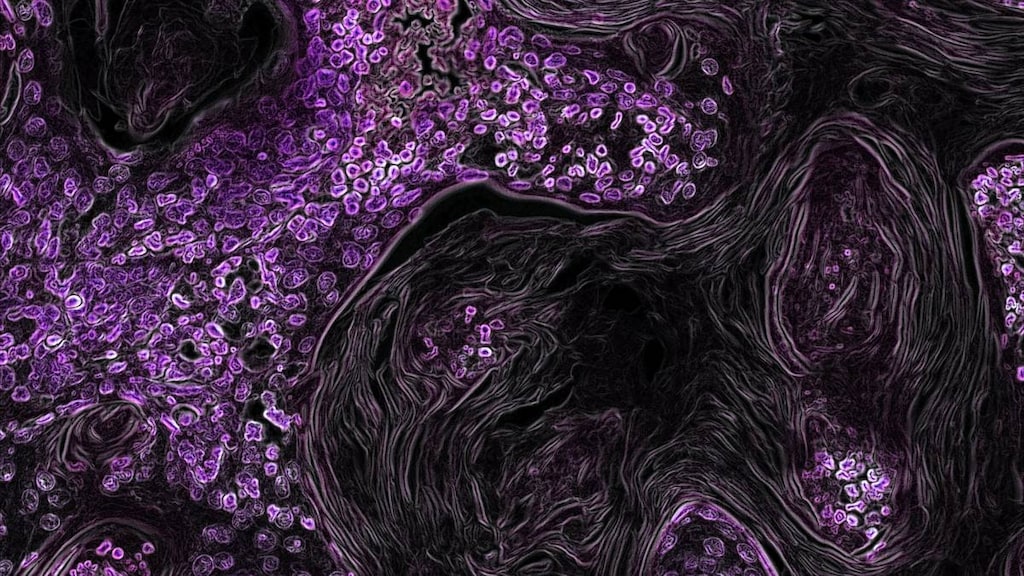
Cabazitaxel is a taxane derivative which is a microtubule inhibitor; it binds to tubulin promoting assembly into microtubules and inhibiting disassembly which stabilizes microtubules. This inhibits microtubule depolymerization and cell division, arresting the cell cycle and inhibiting tumor proliferation. Unlike other taxanes, cabazitaxel has a poor affinity for multidrug resistance (MDR) proteins, therefore conferring activity in resistant tumors.
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: 4,864 L; has greater CNS penetration than other taxanes
Metabolism
Extensively hepatic; primarily via CYP3A4 and 3A5; also via CYP2C8 (minor)
Excretion
Feces (76% as metabolites); Urine (~4%)
Half-Life Elimination
Terminal: 95 hours
Protein Binding
89% to 92%; primarily to serum albumin and lipoproteins
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Clearance was decreased 39% in patients with severe hepatic impairment (total bilirubin >3 times ULN) as compared to patients with mild impairment (total bilirubin >1 to ≤1.5 times ULN and AST >1.5 times ULN).
Use: Labeled Indications
Prostate cancer, metastatic: Treatment of castration-resistant metastatic prostate cancer (in combination with prednisone) in patients previously treated with a docetaxel-containing regimen.
Contraindications
Severe hypersensitivity to cabazitaxel or any component of the formulation, or to other medications formulated with polysorbate 80; neutrophil count ≤1,500/mm3; severe hepatic impairment (total bilirubin >3 times ULN); pregnancy
Canadian labeling: Additional contraindications (not in the US labeling): Concomitant vaccination with yellow fever vaccine
Dosage and Administration
Dosing: Adult
Note: Premedicate at least 30 minutes prior to each dose of cabazitaxel with an antihistamine (eg, diphenhydramine IV 25 mg or equivalent), a corticosteroid (eg, dexamethasone 8 mg IV or equivalent), and an H2 antagonist (eg, ranitidine 50 mg IV or equivalent). Per the manufacturer, antiemetic prophylaxis (oral or IV) is also recommended.
Prostate cancer, metastatic: IV: 20 mg/m2 once every 3 weeks (in combination with prednisone) (Eisenberger 2017). A dose of 25 mg/m2 once every 3 weeks (in combination with prednisone) may be used in select patients at the discretion of the prescriber.
Dosage adjustment for concomitant medications:
Strong CYP3A inhibitors: Concomitant use with strong CYP3A inhibitors (eg, ketoconazole, itraconazole, clarithromycin, protease inhibitors, nefazodone, telithromycin, voriconazole) may increase cabazitaxel plasma concentrations; avoid concurrent use. If concomitant use cannot be avoided, consider reducing cabazitaxel dose by 25%.
Dosing: Adjustment for Toxicity
Note: If receiving cabazitaxel 20 mg/m2 and a dose reduction is required, decrease the dose to 15 mg/m2. If receiving cabazitaxel 25 mg/m2, the dose should decrease to 20 mg/m2; one additional dose reduction to 15 mg/m2 may be considered.
Hematologic toxicity:
Neutropenia ≥ grade 3 for >1 week despite WBC growth factors: Delay treatment until ANC >1,500/mm3 and then reduce dose by one dose level with continued WBC growth factor secondary prophylaxis.
Neutropenic fever or neutropenic infection: Delay treatment until improvement/resolution and ANC >1,500/mm3 and then reduce dose by one dose level with continued WBC growth factor secondary prophylaxis.
Nonhematologic toxicity:
Severe hypersensitivity: Discontinue immediately.
Diarrhea ≥ grade 3 or persistent despite appropriate medication, fluids, and electrolyte replacement: Delay treatment until improves or resolves and then reduce dose by one dose level.
Hemorrhagic cystitis (severe): Interrupt or discontinue cabazitaxel; may require medical/surgical supportive care.
Peripheral neuropathy (grade 2): Delay treatment until improves or resolves and then reduce dose by one dose level.
Peripheral neuropathy ≥ grade 3: Discontinue treatment.
Pulmonary symptoms (new or worsening): Interrupt cabazitaxel treatment, monitor closely and promptly investigate and manage symptoms. May require discontinuation (carefully evaluate the potential benefits of treatment resumption).
Dosing: Obesity
ASCO Guidelines for appropriate chemotherapy dosing in obese adults with cancer: Utilize patient's actual body weight (full weight) for calculation of body surface area- or weight-based dosing, particularly when the intent of therapy is curative; manage regimen-related toxicities in the same manner as for nonobese patients; if a dose reduction is utilized due to toxicity, consider resumption of full weight-based dosing with subsequent cycles, especially if cause of toxicity (eg, hepatic or renal impairment) is resolved (Griggs 2012).
Reconstitution
Do not prepare or administer in PVC-containing infusion containers or polyurethane infusion sets. Cabazitaxel and diluent vials contain overfill. Preparation requires 2 steps. Slowly inject the entire contents of the provided diluent vial into the cabazitaxel 60 mg/1.5 mL vial, directing the diluent down the vial wall. Mix gently by inverting the vial for at least 45 seconds; do not shake. Allow vial to sit so that foam dissipates and solution appears homogeneous. This results in an intermediate reconstituted concentration of 10 mg/mL. Further dilute within 30 minutes into a 250 mL D5W or NS non-PVC infusion container to final concentration of 0.1 to 0.26 mg/mL (total doses >65 mg will require a larger infusion volume; final concentration should not exceed 0.26 mg/mL). Gently invert container to mix. Do not use infusion solutions if crystals or precipitate appear; discard if this occurs. Infusion should be completed within 8 hours if stored at room temperature. For infusion solutions stored under refrigeration, the infusion should be completed within 24 hours.
Administration
IV: Infuse over 1 hour using a 0.22-micron inline filter. Do not use polyurethane-containing infusion sets for administration. Allow to reach room temperature prior to infusion. Premedicate with an antihistamine, a corticosteroid, and an H2 antagonist at least 30 minutes prior to infusion. Observe closely during infusion (for hypersensitivity). Per the manufacturer, antiemetic prophylaxis (oral or IV) is also recommended.
Storage
Store intact vials at 25°C (77°F); excursions permitted between 15°C and 30°C (59°F and 86°F). Do not refrigerate. Do not prepare or administer in PVC-containing infusion containers or polyurethane infusion sets. The initial reconstituted solution (at 10 mg/mL) is stable for 30 minutes in the vial and solutions for infusion are stable for up to 8 hours at room temperature (includes the 1 hour infusion) or 24 hours refrigerated (includes the 1 hour infusion).
Drug Interactions
Anthracyclines: Taxane Derivatives may enhance the adverse/toxic effect of Anthracyclines. Taxane Derivatives may increase the serum concentration of Anthracyclines. Taxane Derivatives may also increase the formation of toxic anthracycline metabolites in heart tissue. Consider therapy modification
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Cabazitaxel. Management: Concurrent use of cabazitaxel with strong inhibitors of CYP3A4 should be avoided when possible. If such a combination must be used, consider a 25% reduction in the cabazitaxel dose. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
DOXOrubicin (Conventional): Taxane Derivatives may decrease the metabolism of DOXOrubicin (Conventional). Management: Consider using docetaxel instead of paclitaxel as a way to avoid this potential interaction, and monitor closely for toxic effects of doxorubicin. Administer doxorubicin prior to paclitaxel when used concomitantly. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Platinum Derivatives: May enhance the myelosuppressive effect of Taxane Derivatives. Administer Taxane derivative before Platinum derivative when given as sequential infusions to limit toxicity. Consider therapy modification
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Adverse reactions reported for combination therapy with prednisone.
>10%:
Central nervous system: Fatigue (25% to 37%), peripheral neuropathy (13%; grades 3/4: <1%), peripheral sensory neuropathy (7% to 11%; grades 3/4: <1%)
Gastrointestinal: Diarrhea (27% to 47%), nausea (25% to 34%), vomiting (15% to 22%), constipation (18% to 20%), decreased appetite (13% to 19%), abdominal pain (6% to 17%), anorexia (16%), dysgeusia (7% to 11%)
Genitourinary: Hematuria (14% to 21%), urinary tract infection (7% to 11%)
Hematologic & oncologic: Anemia (98% to 100%; grades 3/4: 10% to 14%), leukopenia (80% to 96%; grades 3/4: 29% to 69%), neutropenia (3% to 94%; grades 3/4: 2% to 87%), thrombocytopenia (35% to 48%; grades 3/4: 3% to 4%)
Neuromuscular & skeletal: Weakness (15% to 20%), back pain (11% to 16%), arthralgia (7% to 11%)
Respiratory: Dyspnea (5% to 12%), cough (6% to 11%)
Miscellaneous: Fever (5% to 12%)
1% to 10%:
Cardiovascular: Peripheral edema (7% to 9%), cardiac arrhythmia (5%), hypotension (5%)
Central nervous system: Dizziness (4% to 8%), headache (4% to 8%), pain (5%)
Dermatologic: Alopecia (3% to 10%)
Endocrine & metabolic: Weight loss (4% to 9%), dehydration (5%)
Gastrointestinal: Dyspepsia (10%), mucosal inflammation (6%), stomatitis (5%)
Genitourinary: Dysuria (4% to 7%), cystitis (1% to 2%; including radiation cystitis)
Hematologic & oncologic: Febrile neutropenia (2% to 9%; grades 3/4: 2% to 9%), neutropenic infection (3% to 7%; grades 3/4: 2% to 6%)
Hepatic: Increased serum ALT, increased serum AST, increased serum bilirubin
Infection: Infection (28% to 38%)
Neuromuscular & skeletal: Ostealgia (8%), muscle spasm (7%), limb pain (5% to 7%)
Renal: Renal failure (4%)
Frequency not defined:
Endocrine & metabolic: Electrolyte disturbance
<1%, postmarketing, and/or case reports: Adult respiratory distress syndrome, enterocolitis, gastritis, gastrointestinal hemorrhage, gastrointestinal perforation, hemorrhagic cystitis (radiation recall), hypersensitivity reaction (includes bronchospasm, erythema, hypotension, skin rash), interstitial pneumonitis, interstitial pulmonary disease, intestinal obstruction, neutropenic enterocolitis, sepsis, septic shock
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: [US Boxed Warning]: Deaths due to neutropenia have been reported. Monitor blood counts frequently. Cabazitaxel is contraindicated in patients with neutrophil count ≤1,500/mm3. Primary prophylaxis with filgrastim is recommended in patients with high-risk clinical features. Neutropenia, anemia, thrombocytopenia, and/or pancytopenia may occur; grade 3 and 4 neutropenia was observed in over 80% of patients treated with cabazitaxel in a clinical trial. Deaths due to neutropenia, neutropenic fever, or infection have been reported, and some have occurred during the first 30 days of therapy; the incidence of fatal neutropenic events was lower with the 20 mg/m2 dose. Treatment delay and dose reduction is recommended following neutropenic fever or prolonged neutropenia. Administration of WBC growth factors may reduce the risk of complications due to neutropenia. Although the efficacy of primary prophylaxis with WBC growth factor with cabazitaxel has not been studied, use is recommended in high-risk patients (eg, older patients, poor performance status, history of neutropenic fever, extensive prior radiation, poor nutrition status, other serious comorbidities); secondary prophylaxis and therapeutic WBC growth factors should be considered in all patients at increased risk for neutropenic complications. Closely monitor patients with hemoglobin <10 g/dL. Monitor complete blood counts weekly during cycle 1 and prior to subsequent treatment cycles, or as clinically indicated.
- Gastrointestinal toxicity: Nausea, vomiting and diarrhea may occur. Diarrhea may be severe and may result in dehydration and electrolyte imbalance; fatalities have been reported. Per the manufacturer, antiemetic prophylaxis is recommended. Antidiarrheal medication and fluid and electrolyte replacement may be necessary. Diarrhea ≥ grade 3 may require treatment delay and or dosage reduction. GI hemorrhage and perforation, enterocolitis, neutropenic enterocolitis, and ileus (some fatal) have also been observed. Use with caution in patients at risk of developing GI complications (eg, elderly patients, those with neutropenia or a prior history of pelvic radiation [the incidence of GI adverse reactions] increases, adhesions, GI ulceration or bleeding, concomitant use of steroids, NSAIDs, antiplatelet or anticoagulant medications). Evaluate promptly if symptoms such as abdominal pain and tenderness, fever, persistent constipation, and diarrhea (with or without neutropenia) occur. May require treatment interruption and/or therapy discontinuation.
- Hypersensitivity reactions: [US Boxed Warning]: Severe hypersensitivity reactions, including generalized rash, erythema, hypotension, and bronchospasm may occur. Immediate discontinuation is required if hypersensitivity is severe; administer appropriate supportive medications. Premedicate with an IV antihistamine, corticosteroid, and H2 antagonist prior to infusion. Use in patients with history of severe hypersensitivity to cabazitaxel or other medications formulated with polysorbate 80 is contraindicated. Observe closely during infusion, especially during the first and second infusions; reaction may occur within minutes. Do not rechallenge after severe hypersensitivity reactions.
- Pulmonary toxicity: Interstitial pneumonia/pneumonitis, interstitial lung disease, and acute respiratory distress syndrome have been observed; may be fatal. Patients with underlying pulmonary disease may be at higher risk for these events. Acute respiratory distress syndrome may occur in the setting of infection. If new or worsening pulmonary symptoms develop, interrupt cabazitaxel treatment, monitor closely and promptly investigate and manage symptoms. May require discontinuation (carefully evaluate the potential benefits of treatment resumption).
- Renal failure: Renal failure (including rare fatalities) has been reported from clinical trials; generally associated with dehydration, sepsis, or obstructive uropathy. Use with caution in patients with severe renal impairment (CrCl <30 mL/minute) and ESRD.
- Urinary disorders: Cystitis, radiation cystitis, and hematuria may occur in patients with prior history of pelvic radiation; hospitalizations have been reported. Cystitis due to radiation recall may occur late in cabazitaxel treatment. Monitor for signs/symptoms of cystitis in patients who received prior pelvic radiation. Interrupt or discontinue cabazitaxel in patients who experience severe hemorrhagic cystitis; may require medical and/or surgical supportive therapy.
Disease-related concerns:
- Hepatic impairment: Use is contraindicated in patients with severe hepatic impairment (total bilirubin >3 times ULN). Use with caution and monitor closely in patients with mild impairment (total bilirubin >1 to ≤1.5 times ULN or AST >1.5 times ULN) and moderate impairment (total bilirubin >1.5 to ≤3 times ULN and any AST); reduce the initial dose in patients with moderate impairment. Due to extensive hepatic metabolism, cabazitaxel exposure is increased in patients with hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Special populations:
- Elderly: Patients ≥65 years of age are more likely to experience certain adverse reactions, neutropenia (including grades 3 and 4), and neutropenic fever. Fatigue, asthenia, pyrexia, dizziness, dyspnea, urinary tract infection, dehydration, diarrhea, and constipation also occurred more frequently in elderly patients compared to younger patients. Death due to infection within 30 days of starting treatment and due to causes other than disease progression (within 30 days of the last cabazitaxel dose) was higher in elderly patients versus younger patients.
Other warnings/precautions:
- Preparation for administration: Failure to properly reconstitute the concentrated vial of cabazitaxel with the correct amount of diluent may lead to higher dosage being administered and increased risk of toxicity. Follow manufacturer instructions carefully.
Monitoring Parameters
CBC with differential and platelets (weekly during first cycle, then prior to each treatment cycle and as clinically indicated); hepatic/renal function. Monitor for hypersensitivity reactions (especially during the first and second infusions). Monitor for signs/symptoms of gastrointestinal disorders (eg, nausea, vomiting, diarrhea, gastrointestinal hemorrhage and perforation, ileus, colitis, abdominal pain/tenderness). Monitor for new or worsening pulmonary symptoms; if received prior pelvic radiation, monitor for signs/symptoms of cystitis.
Pregnancy
Pregnancy Considerations
Cabazitaxel is contraindicated for use in pregnant women.
Based on animal reproduction studies, use may cause fetal harm if administered during pregnancy.
Male patients with female partners of reproductive potential should use effective contraception during treatment and for 3 months after the last cabazitaxel dose.
Patient Education
What is this drug used for?
- It is used to treat prostate cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Nausea
- Weight loss
- Muscle spasms
- Lack of appetite
- Back pain
- Bone pain
- Joint pain
- Burning or numbness feeling
- Hair loss
- Change in taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Blood in the urine
- Painful urination
- Loss of bladder control
- Bowel problems like black, tarry, or bloody stools; fever; mucus in stools; vomiting; vomiting blood; severe abdominal pain; constipation; or diarrhea.
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse.
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in the amount of urine passed, dry mouth, dry eyes, or nausea or vomiting.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Dizziness
- Passing out
- Abnormal heartbeat
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.