Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Asparlas: 3750 units/5 mL (5 mL)
Pharmacology
Mechanism of Action
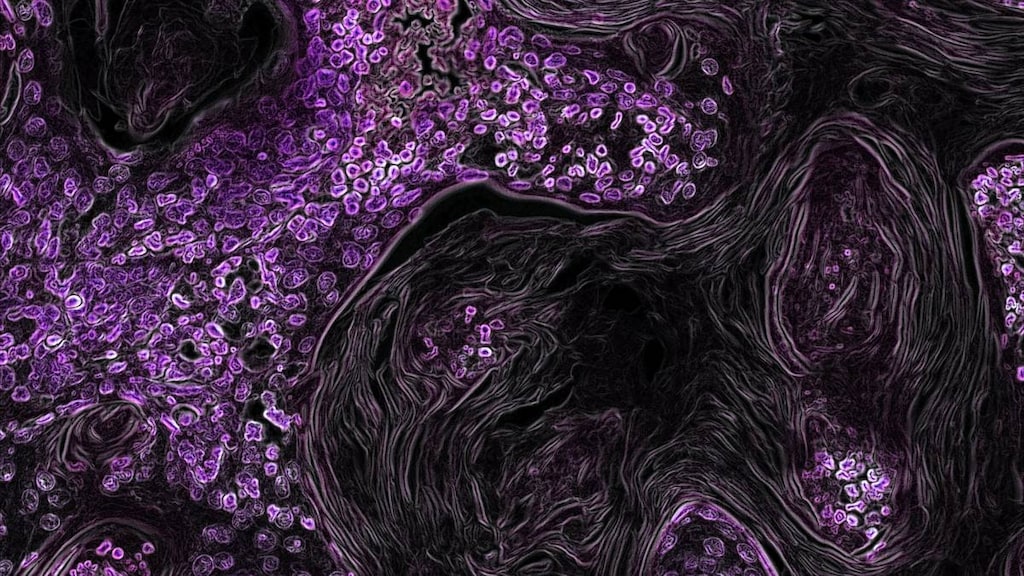
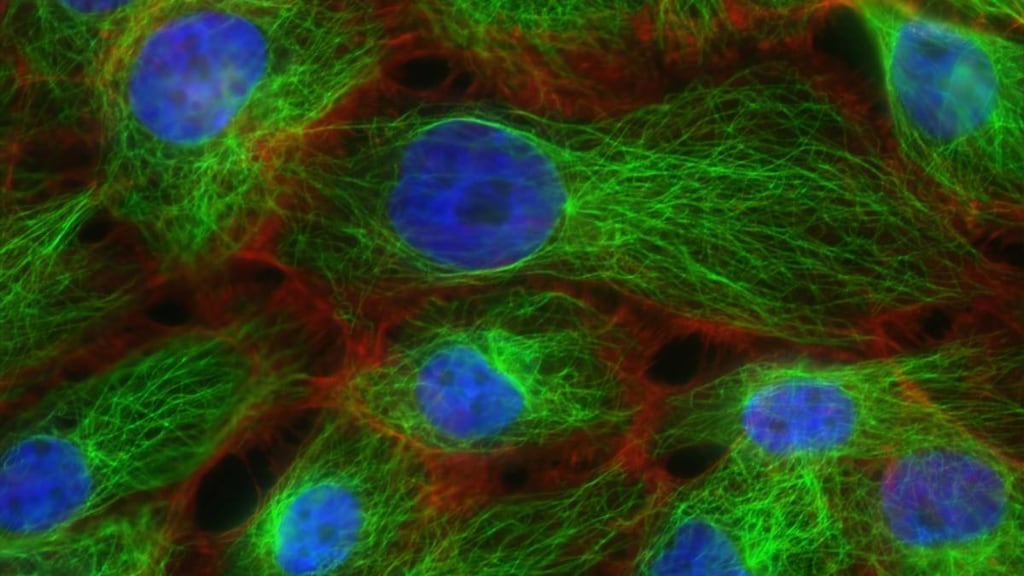
Calaspargase pegol contains an E. coli-derived asparagine-specific enzyme, as a conjugate of L-asparaginase and monomethoxypolyethylene glycol (mPEG) with a succinimidyl carbonate linker which produces a stable bond between the mPEG component and the L-asparaginase lysine groups. L-asparaginase is an enzyme which catalyzes the deamidation of asparagine to aspartic acid and ammonia, reducing circulating levels of asparagine. Leukemic cells with low asparagine synthetase expression have a reduced ability to synthesize L-asparagine. L-asparaginase reduces the exogenous asparagine source for the leukemic cells, resulting in cytotoxicity specific to leukemic cells.
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: 2.96 L
Excretion
Clearance: 0.147 L/day
Time to Peak
1.17 hours
Half-Life Elimination
16.1 days
Use: Labeled Indications
Acute lymphoblastic leukemia: Treatment of acute lymphoblastic leukemia (ALL) (as part of a combination chemotherapy regimen) in children and adults age 1 month to 21 years.
Contraindications
History of serious hypersensitivity reactions, including anaphylaxis, to pegylated L-asparaginase therapy; history of serious pancreatitis, thrombosis, or hemorrhagic events during previous L-asparaginase therapy; severe hepatic impairment
Dosage and Administration
Dosing: Adult
Acute lymphoblastic leukemia: Adults ≤21 years of age: IV: 2,500 units/m2 (as a part of a combination chemotherapy regimen); do not administer more frequently than every 21 days.
Dosing: Pediatric
Acute lymphoblastic leukemia (ALL): Infants, Children, and Adolescents: IV: 2,500 units/m2/dose administered no more frequently than every 21 days (as part of a combination chemotherapy regimen).
Dosing adjustment for toxicity: Infants, Children, and Adolescents:
Hemorrhage: Grade 3 or 4: Hold therapy, evaluate for coagulopathy, and consider clotting factor replacement as needed; if resolution (ie, bleeding controlled), resume therapy with the next scheduled dose.
Hypersensitivity or infusion reactions:
Grade 1: Reduce infusion rate by 50%.
Grade 2: Interrupt infusion and treat symptoms; after resolution of symptoms, resume infusion at 50% of previous rate.
Grade 3 or 4: Discontinue permanently.
Pancreatitis: Grade 3 or 4: If lipase or amylase >3 times ULN, hold therapy until enzyme levels stabilize or are declining. Discontinue permanently if clinical pancreatitis confirmed.
Thromboembolism:
Uncomplicated deep vein thrombosis (DVT): Hold therapy, evaluate and treat DVT with antithrombotic therapy; upon resolution of symptoms, consider resuming therapy while continuing concomitant antithrombotic agent(s).
Severe or life-threatening thrombosis: Discontinue permanently; treat thrombosis with necessary medical management.
The following additional adjustments have been recommended for other asparaginase products (Stock 2011): Older Adolescents:
Hyperammonemia-related fatigue: Continue therapy for grade 2 toxicity. If grade 3 toxicity occurs, reduce dose by 25%; resume full dose when toxicity ≤ grade 2 (make up for missed doses). If grade 4 toxicity occurs, reduce dose by 50%; resume full dose when toxicity ≤ grade 2 (make up for missed doses).
Hyperglycemia: Continue therapy for uncomplicated hyperglycemia. If hyperglycemia requires insulin therapy, hold the asparaginase product (and any concomitant corticosteroids) until blood glucose controlled; resume dosing at prior dose level. For life-threatening hyperglycemia or toxicity requiring urgent intervention, hold the asparaginase product (and corticosteroids) until blood glucose is controlled with insulin; resume the asparaginase product and do not make up for missed doses.
Hypertriglyceridemia: If serum triglyceride level <1 g/dL, continue the asparaginase product but monitor closely for pancreatitis. If triglyceride level >1 g/dL, hold the asparaginase product and monitor; resume therapy at prior dose level after triglyceride level returns to baseline.
Dosing: Adjustment for Toxicity
Hemorrhage: Grade 3 or 4: Withhold calaspargase pegol. Evaluate for coagulopathy and consider clotting factor replacement as needed. Resume calaspargase pegol with the next scheduled dose if bleeding is controlled.
Hypersensitivity or infusion reaction:
Grade 1: Reduce the infusion rate by 50%.
Grade 2: Interrupt infusion and manage symptoms; when symptoms resolve, resume the infusion with the infusion rate decreased by 50%.
Grade 3 or 4: Permanently discontinue calaspargase pegol.
Pancreatitis: Grade 3 or 4: Withhold calaspargase pegol for lipase or amylase elevations >3 times ULN until enzyme levels stabilize or are declining. Discontinue calaspargase pegol permanently if clinical pancreatitis is confirmed.
Thromboembolism:
Uncomplicated DVT: Withhold calaspargase pegol and treat with appropriate antithrombotic therapy. Upon resolution of symptoms, consider resuming calaspargase pegol while continuing antithrombotic therapy.
Severe or life-threatening thrombosis: Discontinue calaspargase pegol permanently and treat with appropriate antithrombotic therapy.
The following additional adjustments have been recommended for other asparaginase products (Stock 2011):
Hyperammonemia-related fatigue: Continue therapy for grade 2 toxicity. If grade 3 toxicity occurs, reduce dose by 25%; resume full dose when toxicity ≤ grade 2 (make up for missed doses). If grade 4 toxicity occurs, reduce dose by 50%; resume full dose when toxicity ≤ grade 2 (make up for missed doses).
Hyperglycemia: Continue therapy for uncomplicated hyperglycemia. If hyperglycemia requires insulin therapy, hold the asparaginase product (and any concomitant corticosteroids) until blood glucose controlled; resume dosing at prior dose level. For life-threatening hyperglycemia or toxicity requiring urgent intervention, hold the asparaginase product (and corticosteroids) until blood glucose is controlled with insulin; resume the asparaginase product and do not make up for missed doses.
Hypertriglyceridemia: If serum triglyceride level <1 g/dL, continue the asparaginase product but monitor closely for pancreatitis. If triglyceride level >1 g/dL, hold the asparaginase product and monitor; resume therapy at prior dose level after triglyceride level returns to baseline.
Reconstitution
Dilute in 100 mL of sodium chloride 0.9% injection or dextrose 5% injection. Do not shake or agitate vigorously.
Administration
IV: Infuse over 1 hour into a running infusion of either NS or D5W. Do not infuse other medications through the same intravenous line. Observe for 1 hour after infusion for signs of hypersensitivity.
Do not administer if solution has been shaken or vigorously agitated.
Storage
Store intact vials at 2°C to 8°C (36°F to 46°F); do not freeze. Do not shake. Store in the original carton to protect from light. Unopened vials may be stored at room temperature (15°C to 25°C [59°F to 77°F]) for no more than 48 hours (do not use if stored at room temperature >48 hours). Solutions diluted for infusion should be used immediately after preparation, although may be stored for up to 4 hours at room temperature (15°C to 25°C [59°F to 77°F]) or for up to 24 hours refrigerated at 2°C to 8°C (36°F to 46°F); do not freeze. Protect solutions diluted for infusion from light; do not shake.
Drug Interactions
Pegloticase: May diminish the therapeutic effect of PEGylated Drug Products. Monitor therapy
Pegvaliase: PEGylated Drug Products may enhance the adverse/toxic effect of Pegvaliase. Specifically, the risk of anaphylaxis or hypersensitivity reactions may be increased. Monitor therapy
Adverse Reactions
>10%:
Cardiovascular: Decreased blood pressure
Gastrointestinal: Pancreatitis (12% to 16%)
Hematologic & oncologic: Disorder of hemostatic components of blood (grades 3/4: 14%)
Hepatic: Increased serum transaminases (grades 3/4: 52%), increased serum bilirubin (grades 3/4: 20%)
Hypersensitivity: Hypersensitivity (grades 3/4: 7% to 21%), angioedema
Ophthalmic: Swelling of eye
Respiratory: Bronchospasm
1% to 10%:
Cardiovascular: Embolism (grades 3/4: ≤8%), thrombosis (grades 3/4: ≤8%), cardiac arrhythmia (grades 3/4: 2%), cardiac failure (grades 3/4: 2%)
Gastrointestinal: Diarrhea (grades 3/4: 9%)
Hematologic & oncologic: Hemorrhage (grades 3/4: 4%)
Infection: Sepsis (grades 3/4: 5%), fungal infection (grades 3/4: 3%)
Respiratory: Dyspnea (grades 3/4: 4%), pneumonia (grades 3/4: 3%)
Frequency not defined:
Hematologic & oncologic: Hypofibrinogenemia, prolonged partial thromboplastin time, prolonged prothrombin time
Hypersensitivity: Anaphylaxis
Warnings/Precautions
Concerns related to adverse effects:
- Hemorrhage: Hemorrhage associated with increased prothrombin time (PT), increased partial thromboplastin time (PTT), and hypofibrinogenemia have been reported in patients receiving calaspargase pegol. Evaluate coagulation parameters (including PT, PTT, fibrinogen) in patients with signs/symptoms of hemorrhage. Consider appropriate clotting factor replacement therapy in patients with severe or symptomatic coagulopathy.
- Hepatotoxicity: Hepatotoxicity and abnormal liver function, including elevations of transaminase and bilirubin (direct and indirect) and reduced serum albumin may occur with calaspargase pegol therapy. During treatment cycles that include calaspargase pegol, monitor bilirubin and transaminases at least weekly; continue monitoring for at least 6 weeks after the last calaspargase pegol dose. If serious liver toxicity occurs, discontinue calaspargase pegol and provide supportive care.
- Hyperglycemia: Hyperglycemia has been reported with calaspargase pegol (Angiolillo 2014) and with other asparaginase products. Use with caution in patients with diabetes mellitus and hyperglycemia. Monitor serum glucose.
- Hyperlipidemia: Hyperlipidemia was reported in a small pharmacokinetic study; the incidence was higher in induction phase (Angiolillo 2014).
- Hypersensitivity: Grade 3 and 4 hypersensitivity reactions, including anaphylaxis, have been reported in clinical studies with calaspargase pegol. Hypersensitivity reactions observed with other asparaginase products have included angioedema, lip swelling, eye swelling, erythema, hypotension, bronchospasm, dyspnea, pruritus, and rash. Due to the risk of serious allergic reactions (eg, life-threatening anaphylaxis), administer calaspargase pegol in a clinical setting with resuscitation equipment and other agents necessary to treat anaphylaxis (eg, epinephrine, oxygen, intravenous corticosteroids, and antihistamines). Observe patients for 1 hour after calaspargase pegol administration. Discontinue calaspargase pegol in patients with serious hypersensitivity reactions.
- Pancreatitis: Cases of pancreatitis have been reported in clinical trials with calaspargase pegol. Hemorrhagic or necrotizing pancreatitis have been reported with other asparaginase products. Inform patients of the signs/symptoms of pancreatitis. Untreated pancreatitis may be fatal. Assess serum amylase and/or lipase levels to confirm early signs of pancreatic inflammation. If pancreatitis is suspected, discontinue calaspargase pegol; if pancreatitis is confirmed, do not resume calaspargase pegol.
- Thrombosis: Serious thrombotic events, including sagittal sinus thrombosis (cerebral venous thrombosis), have been reported in clinical studies with calaspargase pegol. Discontinue calaspargase pegol in patients experiencing serious thrombotic events. Consider monitoring antithrombin III activity (Baretto 2017; Czogała 2017); consider repletion if indicated (Baretto 2017).
Other warnings/precautions:
- Medication error prevention: Do not interchange calaspargase pegol for asparaginase (E. coli) or asparaginase (Erwinia), or pegaspargase; ensure the proper asparaginase formulation, route of administration, and dose prior to administration.
Monitoring Parameters
Bilirubin, ALT, AST, and glucose (at least weekly until recovery from treatment cycle); pregnancy test (prior to treatment in females of reproductive potential). Consider monitoring antithrombin III activity (Baretto 2017; Czogała 2017). Observe for 1 hour after infusion for signs of hypersensitivity. Monitor for signs/symptoms of hemorrhage, hepatotoxicity, pancreatitis, and thrombosis.
Pregnancy
Pregnancy Considerations
Adverse events were observed in some animal reproduction studies.
Evaluate pregnancy status prior to use in females of reproductive potential. Effective contraception (which includes a barrier method) should be used during therapy and for at least 3 months after the last calaspargase pegol dose. Oral contraceptives may not be effective and are not recommended as a form of contraception.
Patient Education
What is this drug used for?
- It is used to treat a type of leukemia.
Frequently reported side effects of this drug:
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
- Bruising
- Bleeding
- Severe dizziness
- Passing out
- Severe headache
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.