Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
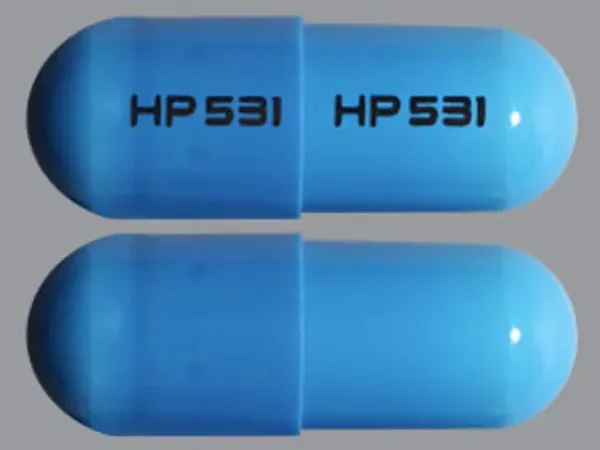
Capsule, Oral:
Generic: 667 mg
Solution, Oral:
Phoslyra: 667 mg/5 mL (473 mL) [contains methylparaben, propylene glycol]
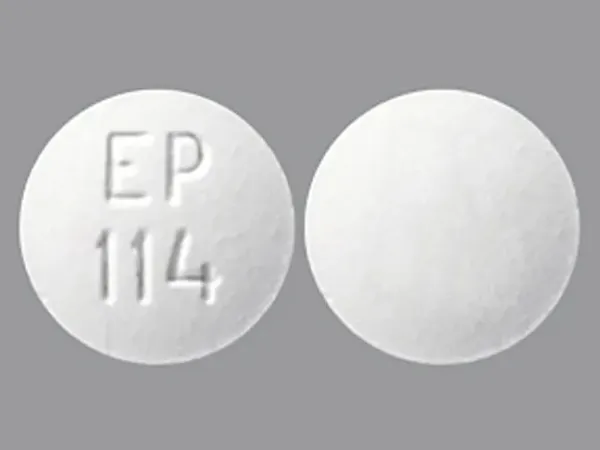
Tablet, Oral:
Calphron: 667 mg
Eliphos: 667 mg [DSC]
Generic: 667 mg, 668 mg
Pharmacology
Mechanism of Action
Combines with dietary phosphate to form insoluble calcium phosphate which is excreted in feces
Pharmacokinetics/Pharmacodynamics
Absorption
30% to 40%; requires vitamin D; minimal unless chronic, high doses are given; calcium is absorbed in soluble, ionized form; solubility of calcium is increased in an acid environment
Excretion
Primarily feces (as unabsorbed calcium); urine (20%)
Use: Labeled Indications
Control of hyperphosphatemia in end-stage renal failure; does not promote aluminum absorption
Contraindications
Hypersensitivity to any component of the formulation; hypercalcemia, renal calculi
Calcium Acetate Images
Dosage and Administration
Dosing: Adult
Control of hyperphosphatemia (ESRD, on dialysis): Oral: Initial: 1334 mg with each meal, can be increased gradually (ie, every 2-3 weeks) to bring the serum phosphate value <6 mg/dL as long as hypercalcemia does not develop (usual dose: 2001-2668 mg calcium acetate with each meal); do not give additional calcium supplements
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dose expressed in mg of calcium acetate. Phosphate binding capacity: Calcium acetate 1 g binds 45 mg of phosphorus (KDOQI 2005)
Control of hyperphosphatemia in end-stage renal failure: Limited data available; dose should be individualized: Children and Adolescents: Oral: Reported initial dose: 667 to 1,000 mg with each meal; titrate (every 2 to 4 weeks) to response and as serum calcium levels allow (Gulati 2010; Wallot 1996). Note: KDOQI guidelines recommend limiting the calcium provided from phosphate binders to 1,500 mg elemental calcium per day and total intake to 2,000 mg elemental calcium from all sources (KDOQI 2010)
Administration
Administer with meals.
Dietary Considerations
Oral dosage forms must be administered with meals to be effective.
Drug Interactions
Alpha-Lipoic Acid: Calcium Salts may decrease the absorption of Alpha-Lipoic Acid. Alpha-Lipoic Acid may decrease the absorption of Calcium Salts. Consider therapy modification
Baloxavir Marboxil: Polyvalent Cation Containing Products may decrease the serum concentration of Baloxavir Marboxil. Avoid combination
Bictegravir: Calcium Salts may decrease the serum concentration of Bictegravir. Management: Bictegravir, emtricitabine, and tenofovir alafenamide can be administered with calcium salts under fed conditions, but coadministration with or 2 hours after a calcium salt is not recommended under fasting conditions. Consider therapy modification
Bisphosphonate Derivatives: Polyvalent Cation Containing Products may decrease the serum concentration of Bisphosphonate Derivatives. Management: Avoid administration of oral medications containing polyvalent cations within: 2 hours before or after tiludronate/clodronate/etidronate; 60 minutes after oral ibandronate; or 30 minutes after alendronate/risedronate. Exceptions: Pamidronate; Zoledronic Acid. Consider therapy modification
Calcium Channel Blockers: Calcium Salts may diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
Calcium Salts: May enhance the adverse/toxic effect of Calcium Acetate. Avoid combination
Cardiac Glycosides: Calcium Salts may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
CefTRIAXone: Calcium Salts (Intravenous) may enhance the adverse/toxic effect of CefTRIAXone. Ceftriaxone binds to calcium forming an insoluble precipitate. Management: Use of ceftriaxone is contraindicated in neonates (28 days of age or younger) who require (or are expected to require) treatment with IV calcium-containing solutions. In older patients, flush lines with compatible fluid between administration. Consider therapy modification
Deferiprone: Polyvalent Cation Containing Products may decrease the serum concentration of Deferiprone. Management: Separate administration of deferiprone and oral medications or supplements that contain polyvalent cations by at least 4 hours. Consider therapy modification
DOBUTamine: Calcium Salts may diminish the therapeutic effect of DOBUTamine. Monitor therapy
Dolutegravir: Calcium Salts may decrease the serum concentration of Dolutegravir. Management: Administer dolutegravir at least 2 hours before or 6 hours after oral calcium. Administer dolutegravir/rilpivirine at least 4 hours before or 6 hours after oral calcium salts. Alternatively, dolutegravir and oral calcium can be taken together with food. Consider therapy modification
Eltrombopag: Polyvalent Cation Containing Products may decrease the serum concentration of Eltrombopag. Management: Administer eltrombopag at least 2 hours before or 4 hours after oral administration of any polyvalent cation containing product. Consider therapy modification
Estramustine: Calcium Salts may decrease the absorption of Estramustine. Consider therapy modification
Multivitamins/Fluoride (with ADE): May increase the serum concentration of Calcium Salts. Calcium Salts may decrease the serum concentration of Multivitamins/Fluoride (with ADE). More specifically, calcium salts may impair the absorption of fluoride. Management: Avoid eating or drinking dairy products or consuming vitamins or supplements with calcium salts one hour before or after of the administration of fluoride. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): May increase the serum concentration of Calcium Salts. Monitor therapy
PenicillAMINE: Polyvalent Cation Containing Products may decrease the serum concentration of PenicillAMINE. Management: Separate the administration of penicillamine and oral polyvalent cation containing products by at least 1 hour. Consider therapy modification
Phosphate Supplements: Calcium Salts may decrease the absorption of Phosphate Supplements. Management: This applies only to oral phosphate and calcium administration. Administering oral phosphate supplements as far apart from the administration of an oral calcium salt as possible may be able to minimize the significance of the interaction. Exceptions: Sodium Glycerophosphate Pentahydrate. Consider therapy modification
Quinolones: Calcium Salts may decrease the absorption of Quinolones. Of concern only with oral administration of both agents. Exceptions: LevoFLOXacin (Oral Inhalation); Moxifloxacin (Systemic). Consider therapy modification
Raltegravir: Polyvalent Cation Containing Products may decrease the serum concentration of Raltegravir. Management: Administer raltegravir 2 hours before or 6 hours after administration of the polyvalent cations. Dose separation may not adequately minimize the significance of this interaction. Consider therapy modification
Strontium Ranelate: Calcium Salts may decrease the serum concentration of Strontium Ranelate. Management: Separate administration of strontium ranelate and oral calcium salts by at least 2 hours in order to minimize this interaction. Consider therapy modification
Tetracyclines: Calcium Salts may decrease the serum concentration of Tetracyclines. Management: If coadministration of oral calcium with oral tetracyclines can not be avoided, consider separating administration of each agent by several hours. Exceptions: Eravacycline. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May decrease the excretion of Calcium Salts. Continued concomitant use can also result in metabolic alkalosis. Monitor therapy
Thyroid Products: Calcium Salts may diminish the therapeutic effect of Thyroid Products. Management: Separate the doses of the thyroid product and the oral calcium supplement by at least 4 hours. Consider therapy modification
Trientine: Polyvalent Cation Containing Products may decrease the serum concentration of Trientine. Management: Avoid concomitant administration of trientine and oral products that contain polyvalent cations. If oral iron supplements are required, separate the administration by 2 hours. If other oral polyvalent cations are needed, separate administration by 1 hour. Consider therapy modification
Vitamin D Analogs: Calcium Salts may enhance the adverse/toxic effect of Vitamin D Analogs. Monitor therapy
Adverse Reactions
>10%:
Endocrine & metabolic: Hypercalcemia
Gastrointestinal: Diarrhea (oral solution)
1% to 10%: Gastrointestinal: Nausea, vomiting
Postmarketing and/or case reports: Dizziness, edema, pruritus, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Gastrointestinal effects: Constipation, bloating, and gas are common with calcium supplements (especially carbonate salt).
- Hypercalcemia: Mild-to-severe hypercalcemia may occur; decrease calcium acetate dose or temporarily discontinue, depending on severity of hypercalcemia; in addition, decrease or discontinue any concomitant vitamin D therapy. Chronic hypercalcemia may result in generalized vascular and soft tissue calcification, exacerbate nephrolithiasis, and has been associated with increased mortality in adults with chronic kidney disease (CKD) (KDIGO 2017).
Disease-related concerns:
- Arrhythmias: Use with caution in patients who may be at risk of cardiac arrhythmias.
- Chronic kidney disease: In CKD patients receiving phosphate-lowering treatment, consider using non-calcium-based phosphate-lowering agents (eg, sevelamer, lanthanum) as an alternative to calcium-based phosphate-lowering agents (eg, calcium acetate, calcium carbonate) or restricting the dose of the calcium-based phosphate-lowering agents (Allison 2013; KDIGO 2017). A meta-analysis observed a trend toward a decrease in all-cause mortality in CKD patients receiving non-calcium-based phosphate-lowering agents compared with those receiving calcium-based phosphate-lowering agents (Jamal 2013); however, further research is needed to identify causes of mortality and fully assess safety of long-term use based on phosphate-lowering agent type.
- Hypoparathyroid disease: Hypercalcemia and hypercalciuria are most likely to occur in hypoparathyroid patients receiving high doses of vitamin D.
Concurrent drug therapy issues:
- Digitalis: Use with caution in digitalized patients; hypercalcemia may precipitate cardiac arrhythmias.
- Minerals/other oral drugs: Calcium administration interferes with absorption of some minerals and drugs; use with caution.
Dosage form specific issues:
- Maltitol: Oral solution may contain maltitol (a sugar substitute) which may cause a laxative effect.
Other warnings/precautions:
- Appropriate product selection: Multiple salt forms of calcium exist; close attention must be paid to the salt form when ordering and administering calcium; incorrect selection or substitution of one salt for another without proper dosage adjustment may result in serious over or under dosing.
Monitoring Parameters
Serum calcium (twice weekly during initial dose adjustments), serum phosphorus; serum calcium-phosphorus product; intact parathyroid hormone (iPTH)
KDIGO guidelines:
Serum calcium, phosphorus, and parathyroid hormone (PTH): Frequency of measurement may be dependent upon the presence and magnitude of abnormalities, the rate of progression of chronic kidney disease (CKD), and the use of treatments for chronic kidney disease-mineral and bone disorder (CKD-MBD) (KDIGO 2017):
CKD stage G3a to G3b: Serum calcium and phosphate: Every 6 to 12 months; PTH: Frequency based on baseline level and progression of CKD
CKD stage G4: Serum calcium and phosphate: Every 3 to 6 months; PTH: Every 6 to 12 months
CKD stage G5 and G5D: Serum calcium and phosphate: Every 1 to 3 months; PTH: Every 3 to 6 months
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted. Calcium crosses the placenta. The amount of calcium reaching the fetus is determined by maternal physiological changes. Intestinal absorption of calcium increases during pregnancy. If use is required in pregnant patients with end stage renal disease, fetal harm is not expected if maternal calcium concentrations are monitored and maintained within normal limits as recommended (IOM 2011).
Patient Education
What is this drug used for?
- It is used to lower high phosphate levels.
Frequently reported side effects of this drug
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.