Boxed Warning
Myelosuppression (injection)
Carmustine causes suppression of marrow function (including thrombocytopenia and leukopenia), which may contribute to bleeding and overwhelming infections. Monitor blood counts weekly for at least 6 weeks after each dose. Adjust dosage based on nadir blood counts from the prior dose. Do not administer a repeat course of carmustine until blood counts recover.
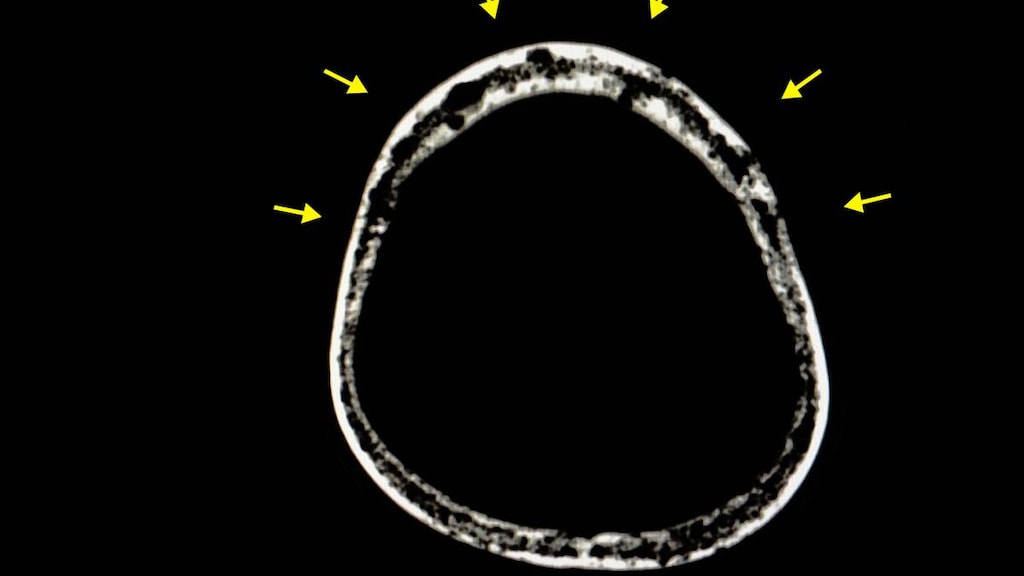
Pulmonary toxicity (injection)
Carmustine causes dose-related pulmonary toxicity. Patients receiving greater than 1,400 mg/m2 cumulative dose are at significantly higher risk than those receiving less. Delayed pulmonary toxicity can occur years after treatment, and can result in death, particularly in patients treated in childhood.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution Reconstituted, Intravenous:
BiCNU: 100 mg (1 ea) [contains alcohol, usp]
Generic: 100 mg (1 ea)
Wafer, Implant:
Gliadel Wafer: 7.7 mg (8 ea) [contains polifeprosan 20]
Pharmacology
Mechanism of Action
Carmustine interferes with the normal function of DNA and RNA by alkylation and cross-linking the strands of DNA and RNA, and by possible protein modification; may also inhibit enzyme processes by carbamylation of amino acids in protein.
Pharmacokinetics/Pharmacodynamics
Absorption
Wafer: Systemic absorption measurable for ~24 hours after insertion
Distribution
IV: 3.3 L/kg; readily crosses blood-brain barrier producing CSF levels ≥50% of blood plasma levels; highly lipid soluble
Metabolism
Rapidly hepatic; forms active metabolites
Excretion
IV: Urine (~60% to 70%) within 96 hours; lungs (~10% as CO2)
Time to Peak
Wafer: Systemic: ~3 hours after insertion
Half-Life Elimination
IV: 15 to 75 minutes
Use: Labeled Indications
Brain tumors:
Injection: Palliative treatment of brain tumors including glioblastoma, brainstem glioma, medulloblastoma, astrocytoma, ependymoma, and metastatic brain tumors
Wafer (implant): Treatment of newly-diagnosed high-grade glioma (as an adjunct to surgery and radiation); treatment of recurrent glioblastoma (as adjunct to surgery)
Hodgkin lymphoma, relapsed/refractory: Injection: Palliative treatment (secondary) of Hodgkin lymphoma (in combination with other antineoplastics) that has relapsed with or was refractory to primary therapy
Multiple myeloma: Injection: Palliative treatment of multiple myeloma (in combination with prednisone)
Non-Hodgkin lymphomas, relapsed/refractory: Injection: Palliative treatment (secondary) of non-Hodgkin lymphoma (in combination with other antineoplastics) that has relapsed with or was refractory to primary therapy
Use: Off Label
Mycosis fungoides (topical)c
Data from a nonrandomized observational study of patients with mycosis fungoides treated with topical carmustine suggests that topical carmustine is beneficial for the treatment of patients with this condition Zackheim 2003. Clinical experience suggests that topical chemotherapy may only be appropriate for early stage disease, when there are limited number of lesions/disease sites Whittaker 2016.
Stem cell or bone marrow transplant (autologous) conditioning regimenb
Data from a nonrandomized clinical study in patients with poor-risk Hodgkin lymphoma, a randomized active comparator study in patients with poor prognosis histologically aggressive non-Hodgkin lymphoma, and a nonrandomized study in relapsed or refractory non-Hodgkin lymphoma support the use of carmustine (in combination with etoposide, cytarabine, and melphalan [BEAM regimen]) administered prior to stem cell or bone marrow transplantation Chopra 1993, Linch 2010, Mills 1995. Data from a nonrandomized clinical study in patients with advanced Hodgkin lymphoma also supports the use of carmustine (in combination with cyclophosphamide and etoposide [CBV regimen]) administered prior to stem cell or bone marrow transplantation Reece 1991.
Contraindications
IV: Hypersensitivity to carmustine or any component of the formulation
Implant: There are no contraindications listed in the manufacturer's labeling.
Dosage and Administration
Dosing: Adult
Note: Carmustine (IV) is associated with a moderate to high emetic potential (dose-related); antiemetics are recommended to prevent nausea and vomiting (Dupuis 2011; Hesketh 2017; Roila 2016).
Brain tumors, Hodgkin lymphoma, multiple myeloma, non-Hodgkin lymphoma: Manufacturer’s labeling: IV: 150 to 200 mg/m2 every 6 weeks or 75 to 100 mg/m2/day for 2 days every 6 weeks (as a single agent in previously untreated patients; lower doses are used in combination with other chemotherapy agents)
Glioblastoma (recurrent), glioma (newly-diagnosed high-grade): Implantation (wafer): 8 wafers (7.7 mg each) implanted intracranially into in the resection cavity (total dose 61.6 mg); should the size and shape not accommodate 8 wafers, the maximum number of wafers feasible (up to 8) should be placed
Indication-specific dosing:
Brain tumor, primary (off-label doses): IV:
80 mg/m2/day for 3 days every 8 weeks for 6 cycles (Brandes 2004)
200 mg/m2 every 8 weeks [maximum cumulative dose: 1,500 mg/m2] (Selker 2002)
Hodgkin lymphoma, relapsed or refractory (off-label dose): IV: Mini-BEAM regimen: 60 mg/m2 day 1 every 4 to 6 weeks (in combination with etoposide, cytarabine, and melphalan) (Colwill 1995; Martin 2001)
Multiple myeloma, relapsed, refractory (off-label dose): IV: VBMCP regimen: 20 mg/m2 day 1 every 35 days (in combination with vincristine, melphalan, cyclophosphamide, and prednisone) (Kyle 2006; Oken 1997)
Mycosis fungoides, early stage (off-label use): Topical:
Ointment (10 mg/100 grams petrolatum): Apply once daily to affected areas (Zackheim 2003).
Solution (10 mg/60 mL water): Apply once daily to affected areas (Zackheim 2003).
Stem cell or bone marrow (autologous) transplant conditioning regimen (off-label use): IV:
BEAM regimen: 300 mg/m2 as a single dose 6 days prior to transplant (in combination with etoposide, cytarabine, and melphalan) (Chopra 1993; Linch 2010)
CBV regimen: 600 mg/m2 as a single dose 3 days prior to transplant (in combination with cyclophosphamide and etoposide) (Reece 1991)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Children are at increased risk for pulmonary toxicity due to carmustine, weigh risk vs benefit before use. Refer to individual protocols; dosing and frequency may vary.
Brain tumors, myeloablative therapy prior to autologous stem cell rescue: Very limited data available; Infants, Children, and Adolescents: IV: 100 mg/m2/dose twice daily for 3 days (total: 600 mg/m2) as part of a high dose combination chemotherapy regimen is most commonly reported in trials with mixed results (Dunkel 1998; Finlay 2008); however, a phase I trial identified a lower dose of 100 mg/m2/dose once daily for 3 days (total: 300 mg/m2) in combination with thiotepa as the maximum tolerated regimen with a high degree of pulmonary toxicity observed (Gilman 2011).
Non-Hodgkin lymphoma; relapsed or resistant, high-dose chemotherapy prior to autologous bone marrow transplant: Limited data available:
BEAM regimen: Adolescents ≥15 years: IV: 300 mg/m2/dose for 1 dose followed by etoposide, cytarabine, and melphalan (Mills 1995).
CBV regimen: Children and Adolescents: IV: 100 mg/m2/dose once daily for 3 days (total dose: 300 mg/m2) on days -8 through -6 in combination with cyclophosphamide and etoposide (Harris 2011).
Dosing adjustment for toxicity: The presented dosing adjustments are based on experience in adult patients; specific recommendations for pediatric patients are limited. Refer to specific protocol for management in pediatric patients if available.
Adult:
Hematologic toxicity: Based on nadir counts with previous dose (manufacturer's labeling). IV:
If leukocytes ≥3,000/mm3 and platelets ≥75,000/mm3: Administer 100% of dose.
If leukocytes 2,000 to 2,999/mm3 or platelets 25,000 to 74,999/mm3: Administer 70% of dose.
If leukocytes <2,000/mm3 or platelets <25,000/mm3: Administer 50% of dose.
Dosing: Adjustment for Toxicity
Hematologic toxicity: Based on nadir counts with previous dose (manufacturer’s labeling). IV:
If leukocytes ≥3,000/mm3 and platelets ≥75,000/mm3: Administer 100% of dose
If leukocytes 2,000 to 2,999/mm3 or platelets 25,000 to 74,999/mm3: Reduce dose to 70% of usual dose
If leukocytes <2,000/mm3 or platelets <25,000/mm3: Reduce dose to 50% of usual dose
Dosing: Obesity
American Society of Clinical Oncology (ASCO) Guidelines for appropriate chemotherapy dosing in obese adults with cancer (Note: Excludes HSCT dosing): Utilize patient's actual body weight (full weight) for calculation of body surface area- or weight-based dosing, particularly when the intent of therapy is curative; manage regimen-related toxicities in the same manner as for nonobese patients; if a dose reduction is utilized due to toxicity, consider resumption of full weight-based dosing with subsequent cycles, especially if cause of toxicity (eg, hepatic or renal impairment) is resolved (Griggs 2012).
American Society for Blood and Marrow Transplantation (ASBMT) practice guideline committee position statement on chemotherapy dosing in obesity: Utilize actual body weight (full weight) for calculation of body surface area in carmustine dosing for hematopoietic stem cell transplant conditioning regimens in adult patients weighing ≤120% of their ideal body weight (IBW). In patients weighing >120% IBW, utilize adjusted body weight 25% (ABW25) to calculate BSA (Bubalo 2014).
ABW25: Adjusted wt (kg) = Ideal body weight (kg) + 0.25 [actual wt (kg) - ideal body weight (kg)]
Reconstitution
Injection: Reconstitute initially with 3 mL of supplied diluent (dehydrated alcohol injection, USP); then further dilute with SWFI (27 mL), this provides a concentration of 3.3 mg/mL in ethanol 10%; protect from light; further dilute for infusion with 500 mL D5W or NS using a non-PVC container (eg, glass, polypropylene or polyolefin) to a concentration of 0.2 mg/mL.
Implant (wafer): Each wafer is packaged within 2 nested aluminum foil pouches; the inner pouch is sterile and is designed to maintain sterility and protect from moisture; the outer wrap is not sterile. Deliver to the operating room in the unopened outer aluminum foil pouch. Do not open until the wafers are ready to be implanted. Follow manufacturer's instructions for opening the pouch, being careful not to apply pressure to the wafer.
Topical (off-label; Zackheim 2003): To prepare an alcohol-based stock solution, dissolve one 100 mg vial with 5 mL of 95% alcohol, then further dilute with 95% alcohol to a total volume of 50 mL for a concentration of 2 mg/mL (0.2%); store in a glass container only. For total body application, dilute 10 mg (5 mL) of the stock solution in 60 mL of room temperature water (avoid warm water). Adjust solution volume needed based on the percentage of skin involvement. To prepare an ointment, mix 10 mg (5 mL) of the stock solution with petrolatum to a final concentration of 10 mg/100 g petrolatum.
Administration
Carmustine (IV) is associated with a moderate to high emetic potential (dose-related); antiemetics are recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016).
Injection: Infuse slowly over at least 2 hours (infusions <2 hours may lead to injection site pain or burning); infuse through a free-flowing saline or dextrose infusion, or administer through a central catheter to alleviate venous pain/irritation. Do not exceed a rate of 1.66 mg/m2/minute.
Irritant; infiltration may result in local pain, erythema, swelling, burning and skin necrosis; the alcohol-based diluent may be an irritant, especially with high doses. Avoid extravasation. Monitor infusion site.
High-dose carmustine (transplant dose; off-label use): Infuse over a least 2 hours to avoid excessive flushing, agitation, and hypotension; was infused over 1 hour in some trials (Chopra 1993). High-dose carmustine may be fatal if not followed by stem cell rescue. Monitor vital signs frequently during infusion; patients should be supine during infusion and may require the Trendelenburg position, fluid support, and vasopressor support.
Implant: Double glove before handling; outer gloves should be discarded as chemotherapy waste after handling wafers. Any wafer or remnant that is removed upon repeat surgery should be discarded as chemotherapy waste. The outer surface of the external foil pouch is not sterile. Open pouch gently; avoid pressure on the wafers to prevent breakage. Wafers that are broken in half may be used, however, wafers broken into more than 2 pieces should be discarded in a biohazard container. Slight overlapping of wafers during placement is acceptable. Oxidized regenerated cellulose (Surgicel) may be placed over the wafer to secure; irrigate cavity prior to closure.
Topical (off-label use): Wear gloves during application. Apply solution with brush or gauze pads; ointment and solution should be applied to involved areas only; avoid contact with eyes/orifices (Zackheim 2003).
Storage
Injection: Store intact vials and provided diluent at 2°C to 8°C (36°F to 46°F). Carmustine has a low melting point (30.5°C to 32°C [86.9°F to 89.6°F]); exposure to temperature at or above the melting point will cause the drug to liquefy and appear as an oil film on the vials; if drug liquefies, discard the vials as this is a sign of decomposition. If there is a question of proper refrigeration upon receipt of product, inspect vials; a small amount of dry flakes or dry congealed mass is acceptable and the vial should be refrigerated immediately.
Reconstituted solutions are stable for 24 hours refrigerated (2°C to 8°C) and protected from light. Examine reconstituted vials for crystal formation prior to use. If crystals are observed, they may be redissolved by warming the vial to room temperature with agitation.
Solutions diluted for infusion to a concentration of 0.2 mg/mL in D5W or NS in glass or polypropylene containers and protected from light should be used within 8 hours when stored at room temperature (25°C); infusion solutions are also stable for 24 hours refrigerated followed by an additional 6 hours at room temperature. Although the manufacturer recommends glass or polypropylene containers be used, stability of a 1 mg/mL solution in D5W has also been demonstrated for up to 6 hours (with a 6% to 7% loss of potency) in polyolefin containers (Trissel 2006).
Implant (wafer): Store at or below -20°C (-4°F). Unopened outer foil pouches may be kept at room temperature for up to 6 hours at a time for up to 3 cycles within a 30-day period.
Topical solution (off-label): Store 0.2% (stock) solution in glass bottle at 2°C to 8°C (36°F to 46°F) for up to 3 months (Zackheim 2003).
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cimetidine: May enhance the myelosuppressive effect of Carmustine. Management: Consider alternatives to cimetidine in patients receiving carmustine. If the combination cannot be avoided, monitor for enhanced carmustine myelotoxicity. Consider therapy modification
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Melphalan: May enhance the adverse/toxic effect of Carmustine. Specifically, melphalan may sensitize patients to carmustine lung toxicity. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Implant:
>10%:
Central nervous system: Seizure (37%; new or worsening: 20%), cerebral edema (4% to 23%), depression (16%)
Dermatologic: Skin rash (5% to 12%)
Gastrointestinal: Nausea (22%), vomiting (21%), constipation (19%)
Genitourinary: Urinary tract infection (21%)
Neuromuscular & skeletal: Weakness (22%)
Miscellaneous: Wound healing impairment (14% to 16%), fever (12%)
1% to 10%:
Cardiovascular: Chest pain (5%)
Central nervous system: Intracranial hypertension (9%), cerebral hemorrhage (6%), meningitis (4%)
Gastrointestinal: Abdominal pain (8%)
Infection: Abscess (local 6%)
Neuromuscular & skeletal: Back pain (7%)
IV: Frequency not defined:
Cardiovascular: Chest pain, flushing (with rapid infusion), occlusive arterial disease, tachycardia
Central nervous system: Brain disease, headache, seizure
Dermatologic: Alopecia, burning sensation of skin, hyperpigmentation
Gastrointestinal: Anorexia, diarrhea, nausea, vomiting
Genitourinary: Gynecomastia
Hematologic & oncologic: Acute leukemia, anemia, bone marrow dysplasia, leukemia, leukopenia (common; onset: 5 to 6 weeks; recovery: after 1 to 2 weeks), thrombocytopenia (common: onset: ~4 weeks; recovery: after 1 to 2 weeks)
Hepatic: Increased serum alkaline phosphatase, increased serum bilirubin, increased serum transaminases
Hypersensitivity: Hypersensitivity reaction
Infection: Opportunistic infection
Local: Burning sensation at injection site, erythema at injection site, pain at injection site, swelling at injection site, tissue necrosis at injection site
Ophthalmic: Blurred vision, conjunctival edema, conjunctival hemorrhage, ophthalmic signs and symptoms (loss of depth perception), suffusion of the conjunctiva (with rapid infusion)
Renal: Azotemia (progressive), nephron atrophy, renal failure
Respiratory: Interstitial pulmonary disease, pneumonitis, pulmonary fibrosis (occurring up to 17 years after treatment), pulmonary infiltrates
<1%, postmarketing, and/or case reports: Febrile neutropenia (Chopra 1993), sepsis (implant), venous thrombosis at injection site (IV)
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: [US Boxed Warning]: Carmustine IV causes bone marrow suppression, primarily thrombocytopenia (which may lead to bleeding) and leukopenia (which may cause infection). Monitor blood counts weekly for at least 6 weeks following each dose. Adjust dosage based on nadir blood counts from prior dose. Do not administer a repeat course until blood counts recover. Hematologic toxicity is dose-limiting, may be severe, and is generally delayed and cumulative; thrombocytopenia is usually more severe than leukopenia. Myelosuppression generally occurs 4 to 6 weeks after administration; thrombocytopenia occurs at ~4 weeks and persists for 1 to 2 weeks; leukopenia occurs at 5 to 6 weeks and persists for 1 to 2 weeks. Anemia may occur (less common and less severe than leukopenia or thrombocytopenia). Platelet counts should be >100,000/mm3, ANC should be >1,000/mm3, and leukocytes should be >4,000/mm3 prior to a repeat course (repeat courses should not be administered more frequently than every 6 weeks).
- Gastrointestinal toxicity: Carmustine IV is associated with a moderate to high emetic potential (dose-related); antiemetics are recommended to prevent nausea and vomiting (Dupuis 2011; Hesketh 2017; Roila 2016).
- Hepatic: Reversible increases in transaminases, bilirubin, and alkaline phosphatase have been reported (rare) with the IV formulation. Monitor liver function tests periodically during treatment.
- Infusion-site reactions: Rapid infusions are associated with skin flushing and suffusion of the conjunctiva (onset: <2 hours; duration ~4 hours). Carmustine is also associated with injection-site burning and local tissue reactions, including swelling, pain, erythema, and necrosis, have been reported. Monitor infusion site closely for infiltration or injection-site reactions. Avoid extravasation.
- Intracranial hypertension: Brain edema has been reported in patients with newly diagnosed glioma receiving wafer implants, including one report of intracranial mass effect unresponsive to corticosteroids that led to brain herniation. Monitor closely for intracranial hypertension related to brain edema, inflammation, or necrosis of brain tissue surrounding resection. Re-operation to remove wafers (or remnants) may be necessary for refractory cases.
- Meningitis: Cases of meningitis have occurred in patients with recurrent glioma receiving wafer implants. Two cases were bacterial (one patient required removal of implants 4 days after implantation and the other developed meningitis following reoperation for recurrent tumor). Another case was determined to be chemical meningitis and resolved with corticosteroids. Monitor postoperatively for signs/symptoms of meningitis and CNS infection.
- Ocular toxicity: Investigational administration (intraarterial intracarotid route [not an approved route]) has been associated with ocular toxicity.
- Pulmonary toxicity: [US Boxed Warning]: Carmustine IV is associated with dose-related pulmonary toxicity; patients receiving cumulative doses >1,400 mg/m2 are at significantly higher risk. Delayed onset of pulmonary fibrosis may occur years after treatment (may be fatal), particularly in children. Pulmonary toxicity has occurred in children and adolescents up to 17 years after treatment; this occurred in ages 1 to 16 for the treatment of intracranial tumors; cumulative doses ranged from 770 to 1,800 mg/m2 (in combination with cranial radiotherapy). Pulmonary toxicity is characterized by pulmonary infiltrates and/or fibrosis and has been reported from 9 days to 43 months after nitrosourea treatment (including carmustine). Although pulmonary toxicity generally occurs in patients who have received prolonged treatment, pulmonary fibrosis has been reported with cumulative doses below 1,400 mg/m2. Interstitial fibrosis at lower doses has occurred (rare). In addition to high cumulative doses, other risk factors for pulmonary toxicity include history of lung disease and baseline predicted forced vital capacity (FVC) or carbon monoxide diffusing capacity (DLCO) <70%. Baseline and periodic pulmonary function tests are recommended. For high-dose treatment (transplant; off-label dose), acute lung injury may occur ~1 to 3 months post transplant; advise patients to contact their transplant physician for dyspnea, cough, or fever; interstitial pneumonia may be managed with a course of corticosteroids.
- Renal: Renal failure, progressive azotemia, and decreased kidney size have been reported. Monitor renal function tests periodically during treatment.
- Secondary malignancies: Long-term IV use is associated with the development of secondary malignancies (acute leukemias and bone marrow dysplasias).
- Seizures: Seizures occurred in patients who received carmustine wafer implants, including new or worsening (treatment-emergent) seizures. Just over half of treatment-emergent seizures occurred within 5 days of surgery; the median onset of first new or worsened post-operative seizure was 4 days. Optimal anti-seizure therapy should be initiated prior to surgery. Monitor (postoperatively) for seizures.
- Wound healing impairment: Impaired neurosurgical wound healing, including would dehiscence, delayed healing, and subdural, subgleal or wound effusions may occur with carmustine wafer implant treatment; cerebrospinal fluid leaks have also been reported. Monitor post-operatively for impaired neurosurgical wound healing.
Disease related concerns:
- Renal impairment: May require dosage adjustment or discontinuation in patients with renal impairment. Do not administer carmustine IV in patients with compromised renal function.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Children are at higher risk of delayed pulmonary toxicity with the IV formulation.
Dosage form specific issues:
- Injection: Diluent contains ethanol.
- Wafer: Monitor closely for known craniotomy-related complications (seizure, intracranial infection, abnormal wound healing, brain edema). Wafer migration may occur; avoid communication between the resection cavity and the ventricular system to prevent wafer migration; communications larger than the wafer should be closed prior to implantation; wafer migration into the ventricular system may cause obstructive hydrocephalus. Monitor for signs/symptoms of obstructive hydrocephalus.
Monitoring Parameters
Evaluate pregnancy status prior to therapy.
Injection: CBC with differential and platelet count (weekly for at least 6 weeks after a dose), pulmonary function tests (FVC, DLCO; at baseline and frequently during treatment), liver function (periodically), renal function tests (periodically); monitor blood pressure and vital signs during administration, monitor infusion site for possible infiltration; monitor for signs/symptoms of pulmonary toxicity; monitor for development of secondary malignancies.
Wafer: Monitor postoperatively for seizures, impaired neurosurgical wound healing, and signs/symptoms of meningitis, CNS infection, and obstructive hydrocephalus; monitor closely for intracranial hypertension related to brain edema, inflammation, or necrosis of brain tissue surrounding resection.
Pregnancy
Pregnancy Considerations
Based on the mechanism of action, and data from animal reproduction studies, carmustine may cause fetal harm if administered to a pregnant woman. Outcome information related to the use of carmustine in pregnancy is limited (NTP 2013).
Evaluate pregnancy status prior to therapy. Females of reproductive potential should use highly effective contraceptives during and for at least 6 months following treatment with carmustine. Males of reproductive potential should use highly effective contraceptives during and for at least 3 months following treatment with carmustine. Carmustine may impair male fertility; advise males of potential risk of infertility.
Patient Education
What is this drug used for?
- It is used to treat cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Lack of appetite
- Diarrhea
- Hair loss
- Constipation
- Abdominal pain
- Back pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Infection
- Meningitis like headache with fever, stiff neck, nausea, confusion, or sensitivity to light
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Chest pain
- Confusion
- Seizures
- Enlarged breasts
- Severe headache
- Severe nausea
- Vomiting
- Vision changes
- Wound healing impairment
- Depression
- Severe loss of strength and energy
- Painful urination
- Fast heartbeat
- Severe dizziness
- Passing out
- Severe injection site redness, swelling, burning, pain, or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.