Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension Reconstituted, Oral:
Generic: 50 mg/5 mL (50 mL, 100 mL); 100 mg/5 mL (50 mL, 100 mL)
Tablet, Oral:
Generic: 100 mg, 200 mg
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and well absorbed (50%); tablet AUC increased 21% to 33% with food
Distribution
Good tissue penetration, including lung and tonsils; penetrates into pleural fluid
Metabolism
De-esterified in GI tract to active metabolite, cefpodoxime
Excretion
Urine (~29% to 33% as unchanged drug) in 12 hours
Time to Peak
Tablets: Within 2 to 3 hours; Oral suspension: Slower in presence of food, 48% increase in Tmax
Half-Life Elimination
~2 to 3 hours; prolonged with renal impairment (~10 hours for CrCl <30 mL/minute)
Protein Binding
Serum: 22% to 33%; Plasma: 21% to 29%
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination is reduced in those with CrCl less than 50 mL/minute.
Special Populations: Elderly
The half-life is increased to about 4.2 hours.
Use: Labeled Indications
Chronic bronchitis, acute bacterial exacerbation: Treatment of acute bacterial exacerbation of chronic bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae (non-beta-lactamase-producing strains only), or Moraxella catarrhalis.
Cystitis, acute uncomplicated: Treatment of acute uncomplicated cystitis caused by Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, or Staphylococcus saprophyticus.
Gonorrhea:
Acute, uncomplicated anorectal infections in women: Treatment of acute, uncomplicated anorectal infections in women due to N. gonorrhoeae (including penicillinase-producing strains). Note: Due to issues of resistance, cefpodoxime is no longer recommended for the treatment of acute, uncomplicated anorectal infections in women.
Acute, uncomplicated urethral and cervical: Treatment of acute, uncomplicated urethral and cervical gonorrhea caused by Neisseria gonorrhoeae (including penicillinase-producing strains). Note: Due to issues of resistance, cefpodoxime is no longer recommended for the treatment of acute, uncomplicated urethral and cervical gonorrhea.
Otitis media, acute: Treatment of acute otitis media caused by S. pneumoniae, (excluding penicillin-resistant strains), Streptococcus pyogenes, H. influenzae (including beta-lactamase-producing strains), or M. catarrhalis (including beta-lactamase producing strains).
Pharyngitis or tonsillitis: Treatment of pharyngitis or tonsillitis caused by S. pyogenes.
Pneumonia, community-acquired: Treatment of community-acquired pneumonia caused by S. pneumoniae or H. influenzae (including beta-lactamase-producing strains).
Rhinosinusitis, acute bacterial: Treatment of acute bacterial rhinosinusitis caused by H. influenzae (including beta-lactamase producing strains), S. pneumoniae, and M. catarrhalis. Note: According to the Infectious Diseases Society of America (IDSA) guidelines for acute bacterial rhinosinusitis, cefpodoxime is recommended in combination with clindamycin due to concern for pneumococcal resistance.
Skin and skin structure infections, uncomplicated: Treatment of uncomplicated skin and skin structure infections caused by S. aureus (including penicillinase-producing strains) or S. pyogenes.
Use: Off Label
Urinary tract infections, complicated (including pyelonephritis)c
Clinical experience suggests the utility of cefpodoxime as an alternative agent in treatment of acute complicated urinary tract infections (including pyelonephritis) after administration of an appropriate parenteral agent Hooton 2018b, Johnson 2018.
Contraindications
Hypersensitivity to cefpodoxime, any component of the formulation, or other cephalosporins
Dosage and Administration
Dosing: Adult
Bronchitis (chronic), bacterial exacerbation: Oral: 200 mg every 12 hours for 10 days
Pneumonia, community acquired: Oral: 200 mg every 12 hours for 14 days. Note: For outpatient empiric therapy in adults, IDSA guidelines recommend use in combination with a macrolide (preferred) or doxycycline and a shortened duration of treatment (ie, minimum of 5 days [patient should be afebrile for ≥48 hours and clinically stable before discontinuation of therapy]) (Mandell 2007).
Rhinosinusitis, acute bacterial (alternative agent for penicillin-allergic patients able to tolerate cephalosporins): Oral: 200 mg every 12 hours (manufacturer's labeling) for 5 to 7 days; if concern for pneumococcal resistance, add clindamycin (IDSA [Chow 2012]; Patel 2018). Note: In uncomplicated acute bacterial rhinosinusitis, initial observation and symptom management without antibiotic therapy is appropriate in most patients (AAO-HNS [Rosenfeld 2015]; Harris 2016).
Skin and skin structure: Oral: 400 mg every 12 hours for 7 to 14 days
Streptococcal pharyngitis (group A) (alternative agent for mild [non-anaphylactic] penicillin allergy): Oral: 100 mg every 12 hours for 5 to 10 days (Pichichero 2018; manufacturer's labeling)
Urinary tract infection (UTI) (alternative agent):
Note: Evidence is limited, but some experts recommend the use of cefpodoxime in this setting. Use with caution and only when recommended agents cannot be used (due to decreased efficacy of oral beta-lactams compared to other agents) (ESMID/IDSA [Gupta 2011]; Hooton 2018a). Closely monitor patient.
Cystitis, acute uncomplicated: Oral: 100 mg twice daily (Hooton 2012; Kavatha 2003) for 5 to 7 days (ESMID/IDSA [Gupta 2011]; Hooton 2018a).
UTI, complicated (including pyelonephritis) (off-label use): Oral: 200 mg twice daily for 10 to 14 days (ESMID/IDSA [Gupta 2011]; Hooton 2018b, Johnson 2018). Note: Oral therapy should follow appropriate parenteral therapy. For outpatient treatment of mild infection, a single dose of a long-acting parenteral agent is acceptable; for outpatients who are more ill or are at risk for more severe illness, consider continuing parenteral therapy until culture and susceptibility results are available (ESMID/IDSA [Gupta 2011]; Hooton 2018b).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection: Mild to moderate infections: Infants, Children, and Adolescents: Oral: 5 mg/kg/dose every 12 hours; usual maximum dose: 200 mg/dose; however, in patients ≥12 years, higher doses (ie, 400 mg/dose) may be required for some types of infection (Bradley 2015; Red Book [AAP 2015])
Bronchitis, bacterial exacerbation of chronic: Children ≥12 years and Adolescents: Oral: 200 mg every 12 hours for 10 days
Otitis media, acute: Infants and Children 2 months to 12 years: Oral: 5 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose. Variable duration of therapy; the manufacturer suggests 5-day course in all patients; however, AAP guidelines recommend duration based on patient age: If <2 years of age or severe symptoms (any age): 10-day course; if 2 to 5 years of age with mild to moderate symptoms: 7-day course; if ≥6 years of age with mild to moderate symptoms: 5- to 7-day course (AAP [Lieberthal 2013]).
Pharyngitis/tonsillitis:
Infants ≥2 months and Children <12 years: Oral: 5 mg/kg/dose every 12 hours for 5 to 10 days; maximum dose: 100 mg/dose
Children ≥12 years and Adolescents: Oral: 100 mg every 12 hours for 5 to 10 days
Pneumonia, acute community-acquired:
Infants >3 months and Children <12 years: Limited data available: Oral: 5 mg/kg/dose every 12 hours; maximum dose: 200 mg/dose (Bradley 2015; IDSA [Bradley 2011])
Children ≥12 years and Adolescents: Oral: 200 mg every 12 hours for 14 days
Rhinosinusitis, acute maxillary:
Infants ≥2 months and Children <12 years: Oral: 5 mg/kg/dose every 12 hours for 10 days; maximum dose: 200 mg/dose; Note: IDSA recommends use in combination with clindamycin for 10 to 14 days in patients with nontype 1 penicillin allergy, after failure of initial therapy or in patients at risk for antibiotic resistance (eg, daycare attendance, age <2 years, recent hospitalization, antibiotic use within the past month) (Chow 2012).
Children ≥12 years and Adolescents: Oral: 200 mg every 12 hours for 10 days
Skin and skin structure: Children ≥12 years and Adolescents: Oral: 400 mg every 12 hours for 7 to 14 days
Urinary tract infection, uncomplicated: Children ≥12 years and Adolescents: Oral: 100 mg every 12 hours for 7 days
Reconstitution
Suspension: Refer to manufacturer’s product labeling for reconstitution instructions.
Administration
Oral: Administer around-the-clock to promote less variation in peak and trough serum levels. Administer tablets with food; suspension may be administered without regard to food. Shake suspension well before using.
Dietary Considerations
Take tablets with food.
Storage
Suspension: Store at 20°C to 25°C (68°F to 77°F); after reconstitution, suspension may be stored in refrigerator for 14 days.
Tablet: Store at 20°C to 25°C (68°F to 77°F); protect from light.
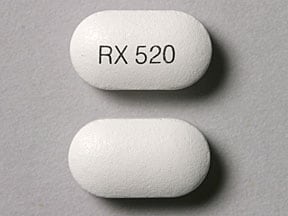
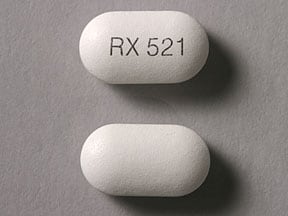
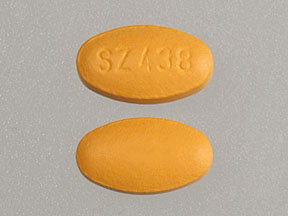
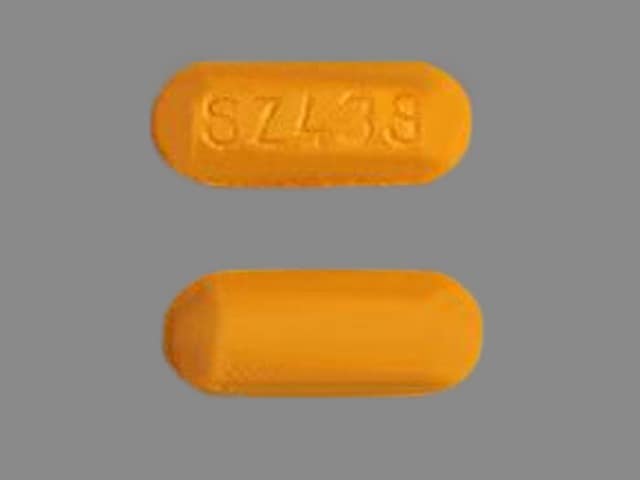
Cefpodoxime Images
Drug Interactions
Aminoglycosides: Cephalosporins (3rd Generation) may enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Antacids: May decrease the serum concentration of Cefpodoxime. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Histamine H2 Receptor Antagonists: May decrease the absorption of Cefpodoxime. Separate oral doses by at least 2 hours. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Probenecid: May increase the serum concentration of Cephalosporins. Monitor therapy
Proton Pump Inhibitors: May decrease the serum concentration of Cefpodoxime. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Cephalosporins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
Positive direct Coombs', false-positive urinary glucose test using cupric sulfate (Benedict's solution, Clinitest®, Fehling's solution), false-positive serum or urine creatinine with Jaffé reaction
Adverse Reactions
>10%:
Dermatologic: Diaper rash (12%)
Gastrointestinal: Diarrhea (infants and toddlers 15%)
1% to 10%:
Central nervous system: Headache (1%)
Dermatologic: Skin rash (1%)
Gastrointestinal: Diarrhea (7%), nausea (4%), abdominal pain (2%), vomiting (1% to 2%)
Genitourinary: Vaginal infection (3%)
<1%: Anaphylaxis, anxiety, chest pain, cough, decreased appetite, dizziness, dysgeusia, epistaxis, eye pruritus, fatigue, fever, flatulence, flushing, fungal skin infection, hypotension, insomnia, malaise, nightmares, pruritus, pseudomembranous colitis, purpuric nephritis, tinnitus, vulvovaginal candidiasis, weakness, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Beta-lactam allergy: Use with caution in patients with a history of beta-lactam allergy, especially IgE-mediated reactions (eg, anaphylaxis, angioedema, urticaria).
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment; modify dosage in severe impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Monitoring Parameters
Monitor renal function. Observe for signs and symptoms of anaphylaxis during first dose.
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Adverse events were not observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Seizures
- Clostridioides (formerly Clostridium) difficile colitis (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.