Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Liquid, Oral, as maleate:
Ed ChlorPed: 2 mg/mL (60 mL [DSC]) [contains fd&c red #40, propylene glycol, saccharin sodium, sodium benzoate; cotton candy flavor]
Syrup, Oral, as maleate:
Aller-Chlor: 2 mg/5 mL (120 mL [DSC]) [contains alcohol, usp, fd&c yellow #6 (sunset yellow), menthol, methylparaben, propylene glycol, propylparaben]
Chlor-Trimeton: 2 mg/5 mL (120 mL) [contains alcohol, usp]
Ed Chlorped Jr: 2 mg/5 mL (118 mL [DSC], 473 mL) [alcohol free, sugar free; contains fd&c red #40, methylparaben, propylene glycol, propylparaben; cherry flavor]
Tablet, Oral, as maleate:
Aller-Chlor: 4 mg [scored; contains fd&c yellow #10 aluminum lake]
Allergy: 4 mg [scored; contains corn starch, fd&c yellow #10 aluminum lake]
Allergy Relief: 4 mg [contains fd&c yellow #10 aluminum lake]
Allergy-Time: 4 mg [contains fd&c yellow #10 aluminum lake]
Chlor-Trimeton: 4 mg [scored]
Ed-Chlortan: 4 mg [DSC] [scored; contains fd&c yellow #10 aluminum lake]
Pharbechlor: 4 mg
Generic: 4 mg
Tablet Extended Release, Oral, as maleate:
Chlor-Trimeton Allergy: 12 mg [contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Chlor-Trimeton Allergy: 12 mg [contains fd&c yellow #6 (sunset yellow), fd&c yellow #6 aluminum lake]
Generic: 12 mg
Pharmacology
Mechanism of Action
Competes with histamine for H1-receptor sites on effector cells in the gastrointestinal tract, blood vessels, and respiratory tract
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: Children and Adolescents 6 to 16 years: 7 ± 2.8 L/kg (Simons 1982); Adults: 6-12 L/kg (Paton 1985)
Metabolism
Hepatic via CYP450 enzymes (including CYP2D6 and other unidentified enzymes) to active and inactive metabolites; significant first-pass effect (Sharma 2003)
Excretion
Urine (Sharma 2003)
Time to Peak
Children and Adolescents 6 to 16 years: Oral : 2.5 ± 1.5 hours (range: 1 to 6 hours) (Simons 1982); Adults: 2-3 hours (Sharma 2003)
Half-Life Elimination
Serum: Children and Adolescents 6 to 16 years: 13.1 ± 6.6 hours (range: 6.3 to 23.1 hours) (Simons 1982); Adults: 14-24 hours (Paton 1985)
Protein Binding
33% (range: 29% to 37%) (Martínez-Gómez 2007)
Use: Labeled Indications
Allergic symptoms, allergic rhinitis, urticaria, pruritus: Perennial and seasonal allergic rhinitis and other allergic symptoms including urticaria, pruritus
Use: Off Label
Motion sicknessc
Data from a limited number of patients studied suggests that chlorpheniramine may be beneficial in the treatment of motion sickness Buckey 2004. Additional data may be necessary to further define its role in this condition.
Contraindications
Hypersensitivity to chlorpheniramine maleate or any component of the formulation; narrow-angle glaucoma; bladder neck obstruction; symptomatic prostate hypertrophy; during acute asthmatic attacks; stenosing peptic ulcer; pyloroduodenal obstruction. Avoid use in premature and term newborns due to possible association with SIDS.
OTC labeling: When used for self-medication, do not use to make a child sleep
Dosage and Administration
Dosing: Adult
Allergic symptoms, allergic rhinitis, urticaria, pruritus: Oral: Chlorpheniramine maleate:
Immediate release: 4 mg every 4 to 6 hours; do not exceed 24 mg/24 hours
Extended release: 12 mg every 12 hours; do not exceed 24 mg/24 hours
Motion sickness (off-label use): Immediate release: 4 to 12 mg administered 3 hours prior to initiating stimulus for motion sickness (Buckey 2004). Note: Avoid use if it is unsafe for patient to be sedated.
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Note: Safety and efficacy for the use of cough and cold products in infants and young children is limited; the AAP warns against the use of these products for respiratory illnesses in infants and young children; the FDA does not recommend OTC use in infants and children <2 years of age due to the risk of serious and life-threatening adverse effects (including death) and recommends to use with caution in pediatric patients ≥2 years of age (AAP 2018; FDA 2017).
Allergic symptoms: Oral:
Immediate release:
Oral liquid (2 mg/5 mL):
Children 2 to <6 years: 1 mg every 4 to 6 hours; maximum daily dose: 6 mg/day.
Children 6 to <12 years: 2 mg every 4 to 6 hours; maximum daily dose: 12 mg/day.
Children ≥12 years and Adolescents: 4 mg every 4 to 6 hours; maximum daily dose: 24 mg/day.
Tablets:
Children 6 to <12 years: 2 mg every 4 to 6 hours; maximum daily dose: 12 mg/day.
Children ≥12 years and Adolescents: 4 mg every 4 to 6 hours; maximum daily dose: 24 mg/day.
Extended-release tablet: Children ≥12 years and Adolescents: 12 mg every 12 hours; maximum dose: 24 mg in 24 hours.
Administration
May be administered with food or water. Timed release oral forms are to be swallowed whole, not crushed or chewed. If used for motion sickness, administer 3 hours before stimulus.
Storage
Protect from light.
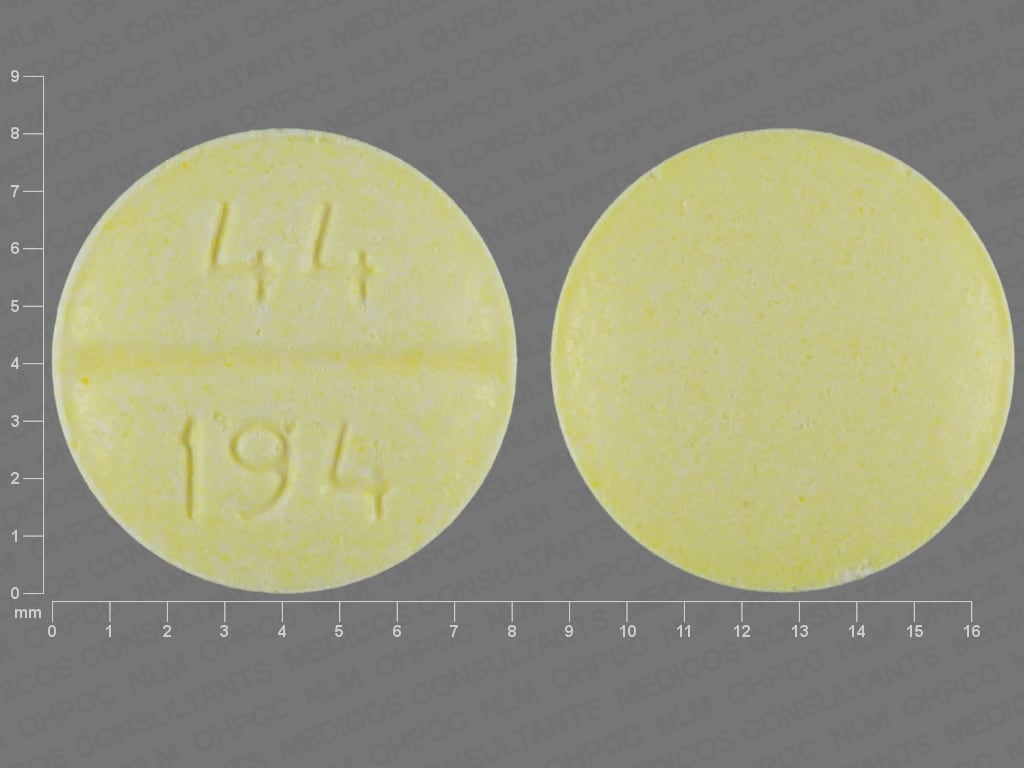
Chlorpheniramine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amezinium: Antihistamines may enhance the stimulatory effect of Amezinium. Monitor therapy
Amphetamines: May diminish the sedative effect of Antihistamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Benzylpenicilloyl Polylysine: Antihistamines may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Suspend systemic H1 antagonists for benzylpenicilloyl-polylysine skin testing and delay testing until systemic antihistaminic effects have dissipated. A histamine skin test may be used to assess persistent antihistaminic effects. Consider therapy modification
Betahistine: Antihistamines may diminish the therapeutic effect of Betahistine. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin-Phenytoin: Chlorpheniramine may increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Hyaluronidase: Antihistamines may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Antihistamines may diminish the therapeutic effect of Pitolisant. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thioridazine: Chlorpheniramine may enhance the arrhythmogenic effect of Thioridazine. Thioridazine may increase the serum concentration of Chlorpheniramine. Management: Avoid this combination when possible. If used, monitor closely for arrhythmia as well as general toxicity of chlorpheniramine. Consider therapy modification
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May suppress the wheal and flare reactions to skin test antigens.
Adverse Reactions
>10%:
Central nervous system: Drowsiness (slight to moderate)
Respiratory: Thickening of bronchial secretions
1% to 10%:
Central nervous system: Dizziness, excitability, fatigue, headache, nervousness
Endocrine & metabolic: Weight gain
Gastrointestinal: Abdominal pain, diarrhea, increased appetite, nausea, xerostomia
Genitourinary: Urinary retention
Neuromuscular & skeletal: Arthralgia, weakness
Ophthalmic: Diplopia
Renal: Polyuria
Respiratory: Pharyngitis
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiovascular disease (including hypertension and ischemic heart disease).
- Increased intraocular pressure: Use with caution in patients with increased intraocular pressure.
- Prostatic hyperplasia/urinary obstruction: Use with caution in patients with prostatic hyperplasia and/or GU obstruction.
- Respiratory disease: Use with caution in patients with asthma or other chronic breathing disorders.
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Pediatric: Antihistamines may cause excitation in young children. Not for OTC use in children <2 years of age.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated with hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Pregnancy
Pregnancy Considerations
Maternal chlorpheniramine use has generally not resulted in an increased risk of birth defects (Aselton 1985; Gilboa 2009; Heinonen 1977; Jick 1981). Antihistamines may be used for the treatment of rhinitis, urticaria, and pruritus with rash in pregnant women (although second generation antihistamines may be preferred) (Angier 2010; Murase 2014; Wallace 2008; Zuberbier 2014). Antihistamines are not recommended for treatment of pruritus associated with intrahepatic cholestasis in pregnancy (Ambros-Rudolph 2011; Kremer 2011).
Patient Education
What is this drug used for?
- It is used to ease allergy signs.
Frequently reported side effects of this drug
- Fatigue
- Anxiety
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.