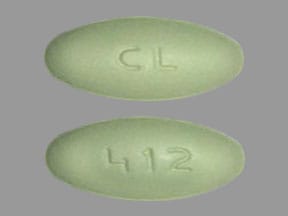
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Sensipar: 30 mg, 60 mg, 90 mg
Generic: 30 mg, 60 mg, 90 mg
Pharmacology
Mechanism of Action
Increases the sensitivity of the calcium-sensing receptor on the parathyroid gland thereby, concomitantly lowering parathyroid hormone (PTH), serum calcium, and serum phosphorus levels, preventing progressive bone disease and adverse events associated with mineral metabolism disorders.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~1,000 L
Metabolism
Hepatic (extensive) via CYP3A4, 2D6, 1A2; forms inactive metabolites
Excretion
Urine ~80% (as metabolites); feces ~15%
Time to Peak
~2 to 6 hours; increased with food
Half-Life Elimination
Terminal: 30 to 40 hours; moderate hepatic impairment: 65 hours; severe hepatic impairment: 84 hours
Protein Binding
~93% to 97%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
In patients with moderate or severe hepatic impairment, the AUCs were 2.4 and 4.2 times higher, respectively, than in healthy subjects; the half-life is increased to 65 hours and 84 hours in patients with moderate and severe hepatic impairment, respectively.
Use: Labeled Indications
Hyperparathyroidism, primary: Treatment of hypercalcemia in adults with primary hyperparathyroidism for whom parathyroidectomy would be indicated on the basis of serum calcium levels, but who are unable to undergo parathyroidectomy.
Hyperparathyroidism, secondary: Treatment of secondary hyperparathyroidism in adults with chronic kidney disease (CKD) on dialysis.
Parathyroid carcinoma: Treatment of hypercalcemia in adults with parathyroid carcinoma.
Contraindications
Serum calcium less than the lower limit of normal range
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to any component of the formulation
Dosage and Administration
Dosing: Adult
Hyperparathyroidism, primary: Oral: Initial: 30 mg twice daily; increase dose incrementally every 2 to 4 weeks (to 60 mg twice daily, 90 mg twice daily, and 90 mg 3 or 4 times daily) as necessary to normalize serum calcium levels.
Hyperparathyroidism, secondary: Oral: Initial: 30 mg once daily; increase dose incrementally every 2 to 4 weeks (to 60 mg once daily, 90 mg once daily, 120 mg once daily, and 180 mg once daily) as necessary to maintain intact parathyroid hormone (iPTH) level between 150 to 300 pg/mL. May be used alone or in combination with vitamin D and/or phosphate binders.
Conversion from etelcalcetide: Discontinue etelcalcetide for at least 4 weeks prior to initiating cinacalcet.
Parathyroid carcinoma: Oral: Initial: 30 mg twice daily; increase dose incrementally every 2 to 4 weeks (to 60 mg twice daily, 90 mg twice daily, and 90 mg 3 to 4 times daily) as necessary to normalize serum calcium levels.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Hyperparathyroidism, secondary: Note: Should only be used when standard therapies have proven ineffective. Ensure calcium is in normal range before initiating therapy and monitor closely throughout treatment. Dosing based on patient's dry weight.
Children ≥3 years and Adolescents: Limited data available, optimal dosage not established in pediatric patients: Oral:
Weight-based dosing: Initial: ≤0.2 mg/kg/dose once daily; may titrate every 4 weeks to reach target range of intact parathyroid hormone (iPTH) of 100 to 300 pg/mL. Maximum daily dose: 180 mg/day or 2.5 mg/kg/dose (whichever is lower) (Warady 2019; Mimpara prescribing information [European Union] 2018). Dosing based on a randomized, double-blind study (n=43) with an open-label phase (n=12) with secondary hyperparathyroidism on hemodialysis or peritoneal dialysis. Cinacalcet was started at ≤0.2 mg/kg/day in 22 patients (mean age: 13.3 ± 3.6 years) and titrated every 4 weeks to goal iPTH. For the efficacy endpoint phase, the mean weight adjusted dose was 1.54 mg/kg/day which corresponded to 50.4 mg/day. iPTH was decreased by ≥30% in 54% of patients receiving cinacalcet compared to 19% with placebo. Serum calcium was significantly reduced in patients receiving cinacalcet compared to placebo and severe hypocalcemia (<7.5 mg/dL) occurred in 3 patients, including 1 death where treatment-related cause could not be ruled out (corrected calcium was 5.3 mg/dL). This study was placed on hold following the reported death and ultimately terminated after 14 months. Despite the limited number of patients enrolled due to study termination, efficacy was still demonstrated (Warady 2019). Note: Cinacalcet use in children <3 years and infants as young as 8 months has been described; however, variable dosing strategies were used or only single doses were administered (Muscheites 2008; Platt 2010; Sohn 2019).
Weight-band dosing (Mimpara prescribing information [European Union] 2018):
|
Weight Band |
Initial Dose |
Suggested Adjustment Doses |
|---|---|---|
|
≥10 to <12.5 kg |
1 mg once daily |
1 mg, 2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg |
|
≥12.5 to <25 kg |
2.5 mg once daily |
2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 30 mg |
|
≥25 to <36 kg |
5 mg once daily |
5 mg, 10 mg, 15 mg, 30 mg, 60 mg |
|
≥36 to <50 kg |
5 mg once daily |
5 mg, 10 mg, 15 mg, 30 mg, 60 mg, 90 mg |
|
≥50 to <75 kg |
10 mg once daily |
10 mg, 15 mg, 30 mg, 60 mg, 90 mg, 120 mg |
|
≥75 kg |
15 mg once daily |
15 mg, 30 mg, 60 mg, 90 mg, 120 mg, 180 mg |
Table converted to the following text:
≥10 to <12.5 kg: 1 mg once daily; suggested adjustment doses: 1 mg, 2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg.
≥12.5 to <25 kg: 2.5 mg once daily; suggested adjustment doses: 2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg, 30 mg.
≥25 to <36 kg: 5 mg once daily; suggested adjustment doses: 5 mg, 10 mg, 15 mg, 30 mg, 60 mg.
≥36 to <50 kg: 5 mg once daily; suggested adjustment doses: 5 mg, 10 mg, 15 mg, 30 mg, 60 mg, 90 mg.
≥50 to <75 kg: 10 mg once daily; suggested adjustment doses: 10 mg, 15 mg, 30 mg, 60 mg, 90 mg, 120 mg.
≥75 kg: 15 mg once daily; suggested adjustment doses: 15 mg, 30 mg, 60 mg, 90 mg, 120 mg, 180 mg.
Dosing adjustment for toxicity:
Dosage adjustment for hypocalcemia (Mimpara prescribing information [European Union] 2018): Children ≥3 years and Adolescents:
Corrected serum calcium at or below age-specific lower limit or symptoms of hypocalcemia (regardless of calcium concentration): Temporarily discontinue cinacalcet and administer calcium supplements, calcium-containing phosphate binders, and/or vitamin D to raise calcium.
Corrected serum calcium above age-specific lower limit and resolution of hypocalcemia symptoms: Re-initiate cinacalcet at a lower dose. If treatment is stopped for ≥14 days, restart at initial dose.
Dose adjustment based on iPTH (Mimpara prescribing information [European Union] 2018): Children ≥3 years and Adolescents:
If iPTH is ≥100 to <150 pg/mL: Reduce dose.
If iPTH <100 pg/mL: Discontinue cinacalcet until iPTH is >150 pg/mL; restart at lower dose; if treatment has been stopped for >14 days, restart at initial dose.
Dosing: Adjustment for Toxicity
Dosage adjustment for hypocalcemia:
If iPTH <150 pg/mL: Reduce dose or discontinue cinacalcet and/or vitamin D.
Hyperparathyroidism, secondary:
If serum calcium >7.5 mg/dL but <8.4 mg/dL or if hypocalcemia symptoms occur: Use calcium-containing phosphate binders and/or vitamin D to raise calcium levels.
If serum calcium <7.5 mg/dL or if hypocalcemia symptoms persist and the dose of vitamin D cannot be increased: Withhold cinacalcet until serum calcium ≥8 mg/dL and/or symptoms of hypocalcemia resolve. Reinitiate cinacalcet at the next lowest dose.
Extemporaneously Prepared
5 mg/mL Oral Suspension
A 5 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet and Ora-Plus or a 1:1 mixture of Ora-Sweet SF and Ora-Plus. Crush five 30 mg tablets in a glass mortar and reduce to a fine powder. Add 15 mL of Ora-Plus in parts and triturate into a smooth suspension. Transfer to a calibrated 2 oz amber bottle. Rinse mortar with Ora-Sweet or Ora-Sweet SF and add to bottle for a final volume of 30 mL and shake suspension. Label “shake well”. Stable for 64 days refrigerated or at room temperature (Thomson 2018).
Thomson K, Hutchinson DJ, Chablani L. Stability of extemporaneously prepared cinacalcet oral suspensions. Am J Health Syst Pharm. 2018;75(9):e236-e240. doi: 10.2146/ajhp170072.29691267
Administration
Administer with food or shortly after a meal. Do not chew, crush, or divide tablet; administer whole.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Cinacalcet Images
Drug Interactions
Ajmaline: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Ajmaline. Monitor therapy
Amphetamines: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Amphetamines. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: If brexpiprazole is to be used together with both a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor, the brexpiprazole dose should be reduced to 25% of the usual dose. Monitor therapy
CloZAPine: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of CloZAPine. Monitor therapy
Codeine: CYP2D6 Inhibitors (Moderate) may diminish the therapeutic effect of Codeine. These CYP2D6 inhibitors may prevent the metabolic conversion of codeine to its active metabolite morphine. Monitor therapy
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Moderate) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Tamoxifen. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Cinacalcet. Monitor therapy
Denosumab: May enhance the hypocalcemic effect of Calcimimetic Agents. Monitor therapy
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Eliglustat: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Etelcalcetide: Cinacalcet may enhance the hypocalcemic effect of Etelcalcetide. Avoid combination
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
Indoramin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Indoramin. Monitor therapy
Metoprolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Metoprolol. Monitor therapy
Nebivolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Nebivolol. Monitor therapy
Perhexiline: CYP2D6 Inhibitors may increase the serum concentration of Perhexiline. Management: Consider alternatives to this combination if possible. If combined, monitor for increased perhexiline serum concentrations and toxicities (eg, hypoglycemia, neuropathy, liver dysfunction). Perhexiline dose reductions will likely be required. Consider therapy modification
Pitolisant: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Pitolisant. Monitor therapy
Propafenone: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Siponimod: Calcimimetic Agents may increase the serum concentration of Siponimod. Management: Coadministration of siponimod with drugs which are both moderate inhibitors of CYP2C9 and moderate or strong inhibitors of CYP3A4 is not recommended. Consider therapy modification
Tacrolimus (Systemic): Cinacalcet may decrease the serum concentration of Tacrolimus (Systemic). Monitor therapy
Tamoxifen: CYP2D6 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Management: Consider alternatives with less of an inhibitory effect on CYP2D6 activity when possible. Consider therapy modification
Tamsulosin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Thioridazine: CYP2D6 Inhibitors may increase the serum concentration of Thioridazine. Avoid combination
TraMADol: CYP2D6 Inhibitors (Moderate) may diminish the therapeutic effect of TraMADol. These CYP2D6 inhibitors may prevent the metabolic conversion of tramadol to its active metabolite that accounts for much of its opioid-like effects. Monitor therapy
Tricyclic Antidepressants: Cinacalcet may increase the serum concentration of Tricyclic Antidepressants. Management: Seek alternatives when possible. If these combinations are used, monitor closely for increased effects/toxicity and/or elevated serum concentrations (when testing is available) of the tricyclic antidepressant. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Hypotension (12%)
Central nervous system: Paresthesia (14% to 29%), headache (≤21%), fatigue (12% to 21%), depression (10% to 18%)
Endocrine & metabolic: Hypocalcemia (<8.4 mg/dL: 6% to 75%; <7.5 mg/dL: 29% to 33%), dehydration (≤24%), hypercalcemia (12% to 21%), hypoparathyroidism (intact parathyroid hormone <100 pg/mL: ≤11%)
Gastrointestinal: Nausea (30% to 66%), vomiting (26% to 52%), diarrhea (21%), anorexia (6% to 21%), constipation (5% to 18%), abdominal pain (11%)
Hematologic & oncologic: Anemia (6% to 17%)
Neuromuscular & skeletal: Bone fracture (12% to 21%), muscle spasm (11% to 18%), arthralgia (6% to 17%), weakness (5% to 17%), myalgia (15%), back pain (12%), limb pain (10% to 12%)
Respiratory: Dyspnea (13%), cough (12%), upper respiratory tract infection (8% to 12%)
1% to 10%:
Cardiovascular: Hypertension (7%)
Central nervous system: Dizziness (7% to 10%), noncardiac chest pain (6%), seizure (≤3%)
Endocrine & metabolic: Hyperkalemia (8%)
Gastrointestinal: Upper abdominal pain (8%), dyspepsia (7%), decreased appetite (6%)
Hypersensitivity: Hypersensitivity reaction (9%)
Infection: Localized infection (dialysis access site; 5%)
Frequency not defined: Hematologic & oncologic: Upper gastrointestinal hemorrhage
<1%, postmarketing, and/or case reports: Adynamic bone disease, angioedema, cardiac arrhythmia, cardiac failure, gastrointestinal hemorrhage, hypotension (idiosyncratic), prolonged Q-T interval on ECG (secondary to hypocalcemia), skin rash, urticaria, ventricular arrhythmia (secondary to hypocalcemia)
Warnings/Precautions
Concerns related to adverse effects:
- Adynamic bone disease: May develop if intact parathyroid hormone (iPTH) levels are suppressed <100 pg/mL; reduce dose or discontinue use of cinacalcet and/or vitamin D if iPTH levels decrease below 150 pg/mL.
- Cardiovascular effects: QT prolongation and ventricular arrhythmia secondary to hypocalcemia may occur. Patients with congenital long QT syndrome, history of QT interval prolongation, family history of long QT syndrome or sudden cardiac death, and other conditions that predispose to QT interval prolongation and ventricular arrhythmia may be at increased risk. Closely monitor corrected serum calcium and QT interval. Cases of idiosyncratic hypotension, worsening of heart failure, and/or arrhythmia have been reported in patients with impaired cardiovascular function; may correlate with decreased serum calcium.
- GI effects: GI bleeding, mostly upper GI bleeding, have been reported (exact cause unknown); patients with risk factors for upper GI bleeding (eg, gastritis, esophagitis, ulcers, severe vomiting) may be at increased risk. Monitor for worsening of common GI adverse reactions of nausea and vomiting and for signs and symptoms of GI bleeding and ulcerations during therapy.
- Hypocalcemia: Life-threatening and fatal events associated with hypocalcemia have occurred. Monitor serum calcium and for symptoms of hypocalcemia (eg, muscle spasms, myalgia, paresthesia, seizure, tetany). Use with caution in patients receiving concomitant therapies known to lower serum calcium concentrations. May require treatment interruption, dose reduction, or initiation (or dose increases) of calcium-based phosphate binder and/or vitamin D to raise serum calcium depending on calcium levels or symptoms of hypocalcemia. Do not initiate therapy if the corrected serum calcium is less than the lower limit of normal; corrected serum calcium must be at or above the lower limit of normal prior to initiation, dose increase, or reinitiation.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with moderate-to-severe hepatic impairment (Child-Pugh classes B and C); cinacalcet exposure and half-life are increased; monitor serum calcium, serum phosphorus and iPTH closely.
- Seizure disorder: Use with caution in patients with a history of seizure disorder; seizure threshold is lowered by significant serum calcium reductions. Monitor calcium levels closely.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Not indicated for chronic kidney disease (CKD) patients not receiving dialysis. In the US, the long-term safety and efficacy of cinacalcet has not been evaluated in CKD patients with hyperparathyroidism not requiring dialysis. Although possibly related to lower baseline calcium levels, clinical studies have shown an increased incidence of hypocalcemia (<8.4 mg/dL) in patients not requiring dialysis.
Monitoring Parameters
Monitor for signs/symptoms of hypocalcemia. Monitor serum calcium and iPTH concentrations closely in patients on concurrent CYP3A4 inhibitors or with seizure disorders; monitor serum calcium, iPTH, and serum phosphorous concentrations closely in patients with hepatic moderate to severe hepatic impairment.
Hyperparathyroidism, secondary: Serum calcium and phosphorus levels prior to initiation and within a week of initiation and frequently during dose titration; iPTH should be measured 1 to 4 weeks after initiation or dosage adjustment (wait at least 12 hours after dose before drawing iPTH levels). After the maintenance dose is established, obtain serum calcium levels monthly.
Parathyroid carcinoma and hyperparathyroidism, primary: Serum calcium levels prior to initiation and within a week of initiation or dosage adjustment; once maintenance dose is established, obtain serum calcium every 2 months.
Pregnancy
Pregnancy Considerations
Information related to the use of cinacalcet in pregnant women is limited (Edling 2014; Horjus 2009; Nadarasa 2014; Rey 2016; Vera 2016).
Patient Education
What is this drug used for?
- It is used to treat high parathyroid hormone levels in certain patients.
- It is used to treat high calcium levels in patients with parathyroid disease.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Constipation
- Abdominal pain
- Diarrhea
- Back pain
- Cough
- Common cold symptoms
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low calcium like muscle cramps or spasms, numbness and tingling, or seizures.
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- Dehydration like dry skin, dry mouth, dry eyes, increased thirst, fast heartbeat, dizziness, fast breathing, or confusion.
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Bowel bleeding like black, tarry, or bloody stools; vomiting blood; severe abdominal pain; severe nausea; or vomiting.
- Chest pain
- Depression
- Joint pain
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Bone pain
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.