Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Clolar: 1 mg/mL (20 mL)
Generic: 1 mg/mL (20 mL)
Pharmacology
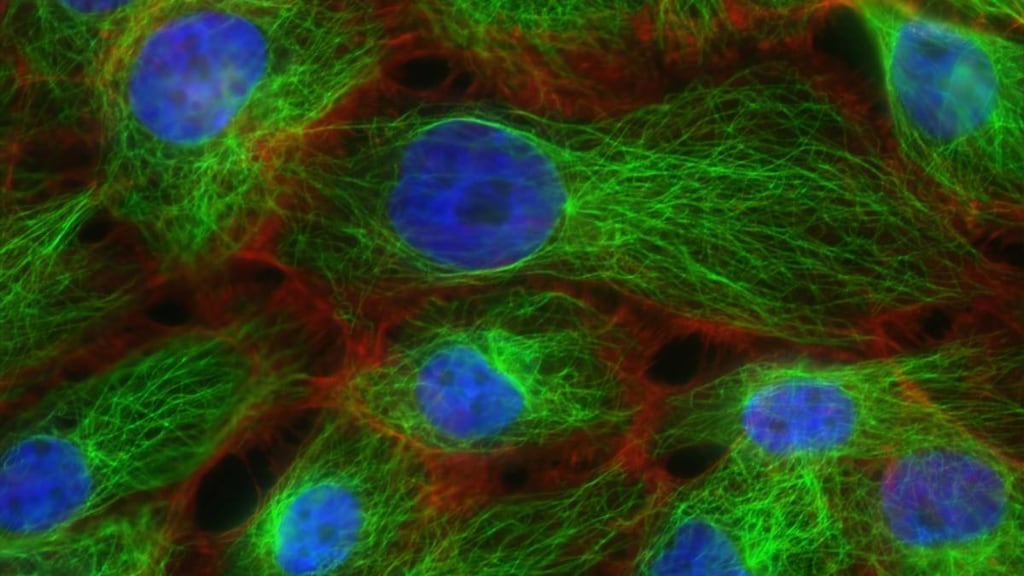
Mechanism of Action
Clofarabine, a purine (deoxyadenosine) nucleoside analog, is metabolized to clofarabine 5'-triphosphate. Clofarabine 5'-triphosphate decreases cell replication and repair as well as causing cell death. To decrease cell replication and repair, clofarabine 5'-triphosphate competes with deoxyadenosine triphosphate for the enzymes ribonucleotide reductase and DNA polymerase. Cell replication is decreased when clofarabine 5'-triphosphate inhibits ribonucleotide reductase from reacting with deoxyadenosine triphosphate to produce deoxynucleotide triphosphate which is needed for DNA synthesis. Cell replication is also decreased when clofarabine 5'-triphosphate competes with DNA polymerase for incorporation into the DNA chain; when done during the repair process, cell repair is affected. To cause cell death, clofarabine 5'-triphosphate alters the mitochondrial membrane by releasing proteins, an inducing factor and cytochrome C.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: Decreased with increasing age, based on pharmacokinetic simulations: 5.8 L/kg (3 years old); 3.1 L/kg (30 years old); 2.7 L/kg (82 years old) (Bonate 2011); Children and Adolescents 2 to 19 years: 172 L/m2
Metabolism
Intracellulary by deoxycytidine kinase and mono- and diphosphokinases to active metabolite clofarabine 5′-triphosphate; limited hepatic metabolism (0.2%)
Excretion
Urine (49% to 60%, as unchanged drug)
Half-Life Elimination
Children and Adolescents 2 to 19 years: 5.2 hours; Children and Adults: 7 hours; may be prolonged in in the elderly and in patients with renal impairment (Bonate, 2011)
Protein Binding
47%, primarily to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
Clofarabine undergoes renal elimination and exposure is increased as creatinine clearance decreases (Bonate 2011). In patients with CrCl 60 to <90 mL/minute, the AUC was increased by 60% and in patients with CrCl 30 to <60 mL/minute, the AUC was increased by 140%.
Use: Labeled Indications
Acute lymphoblastic leukemia, relapsed or refractory: Treatment of relapsed or refractory acute lymphoblastic leukemia (ALL) in patients 1 to 21 years of age (after at least 2 prior regimens)
Use: Off Label
Acute lymphoblastic leukemia, refractory or relapsed (adults)c
Data from a phase II study in adults with refractory or relapsed acute leukemia supports the use of clofarabine as monotherapy in the treatment of patients with acute lymphoblastic leukemia Kantarjian 2003. Additional data may be necessary to further define the role of clofarabine in this condition.
Acute myeloid leukemia, refractory (patients <70 years of age)b
Data from a phase I/II clinical trial in patients 18 to 70 years of age with refractory acute myeloid leukemia (AML) supports the use of clofarabine (in combination with cytarabine and filgrastim) in the treatment of this condition Becker 2011. Additional data may be necessary to further define the role of clofarabine in this condition.
Contraindications
There are no contraindications listed in the manufacturer’s US labeling.
Canadian labeling: Hypersensitivity to clofarabine or any component of the formulation; symptomatic CNS involvement; history of serious heart, liver, kidney, or pancreas disease; severe hepatic impairment (AST and/or ALT >5 x ULN, and/or bilirubin >3 x ULN); severe renal impairment (CrCl <30 mL/minute)
Dosage and Administration
Dosing: Adult
Note: Calculate body surface area (BSA) prior to each cycle, utilizing actual body weight.
Premedications: Clofarabine is associated with a moderate emetic potential; antiemetics are recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016). Consider prophylactic corticosteroids (hydrocortisone 100 mg/m2 on days 1 to 3) to prevent signs/symptoms of capillary leak syndrome or systemic inflammatory response syndrome (SIRS), and hydration and antihyperuricemic therapy (to reduce the risk of tumor lysis syndrome/hyperuricemia).
Acute lymphoblastic leukemia (ALL), relapsed or refractory: Adults ≤21 years: IV: 52 mg/m2/day days 1 through 5; repeat every 2 to 6 weeks; subsequent cycles should begin no sooner than 14 days from day 1 of the previous cycle (subsequent cycles may be administered when ANC ≥750/mm3)
Off-label dosing: IV: 20 to 30 mg/m2 once daily on days 1 through 5 (in combination with cyclophosphamide and etoposide [CLOVE regimen]) as a bridging regimen to hematopoietic stem cell transplant in patients with relapsed or very high risk disease (Gossai 2014)
Acute lymphoblastic leukemia, relapsed/refractory (ALL; off-label population): IV:
Induction: 40 mg/m2 once daily for 5 days; may repeat induction cycle once in 3 to 6 weeks if needed (depending on marrow response and recovery) (Kantarjian 2003)
Consolidation: 30 mg/m2 once daily for 5 days (or last tolerated induction dose, whichever is lower); repeat every 4 weeks for up to a maximum of 6 consolidation cycles (Kantarjian 2003)
Acute myeloid leukemia (AML), refractory (off-label use): Adults <70 years: IV:
Induction: 25 mg/m2/day for 5 days (in combination with cytarabine and filgrastim) may repeat one time after 21 days if needed (Becker 2011)
Consolidation: 20 mg/m2/day for 5 days (in combination with cytarabine and filgrastim) for 1 or 2 cycles (Becker 2011)
Dosing: Pediatric
Dosing and frequency may vary by protocol and/or treatment phase; refer to specific protocol.
Note: Consider prophylactic corticosteroids (hydrocortisone 100 mg/m2 on days 1 to 3) to prevent signs/symptoms of capillary leak syndrome or systemic inflammatory response syndrome (SIRS). Provide IV hydration, antihyperuricemic therapy, and alkalinize the urine to reduce the risk of tumor lysis syndrome/hyperuricemia. Calculate body surface area (BSA) prior to each cycle utilizing actual body weight. Clofarabine is associated with a moderate emetic potential; antiemetics are recommended to prevent nausea and vomiting (Dupuis 2011).
Acute lymphocytic leukemia (ALL), relapsed or refractory:
Monotherapy: Children and Adolescents: IV infusion: 52 mg/m2/day once daily for days 1 to 5 of each cycle; repeat cycle every 2 to 6 weeks following recovery or return to baseline organ function; subsequent cycles should begin no sooner than 14 days from the start of the previous cycle and when ANC ≥750/mm3
Combination therapy: Limited data available: IV Infusion:
Infants: Dosing regimens variable with very limited data available:
Weight-directed dosing: 1.33 mg/kg/day for 5 days in combination with cyclophosphamide and etoposide (O’Connor 2011)
BSA-directed dosing: 40 mg/m2/day for 5 days in combination with cyclophosphamide and etoposide (Inaba 2012); and with topotecan, vinorelbine, thiotepa (TVTC regimen), and dexamethasone in a Phase I trial (Steinherz 2010)
Children and Adolescents: Usual dose: 40 mg/m2/day for 5 days in combination with cyclophosphamide and etoposide has been most frequently studied (Hijiya 2011; Hijiya 2012; Inaba 2012; Locatelli 2009; O’Connor 2011); and with topotecan, vinorelbine, thiotepa (TVTC regimen), and dexamethasone in a Phase I trial (Steinherz 2010). In one trial, the protocol included 5 days of clofarabine therapy during induction and 4 days of therapy for consolidation; this study was also amended to exclude patients with prior hematopoietic stem cell transplantation due to a high incidence of veno-occlusive disease (Hijiya 2011).
Acute myeloid leukemia (AML), relapsed or refractory: Limited data available: Children and Adolescents: IV infusion:
Monotherapy: 52 mg/m2/day once daily for days 1 to 5 of each cycle; repeat cycle every 2 to 6 weeks for up to 12 cycles following recovery or return to baseline organ function; subsequent cycles should begin no sooner than 14 days from the start of the previous cycle and when ANC ≥750/mm3; the trial did not have minimum exclusion age (patient age ≤21 years at time of diagnosis); the youngest patient was 2 years of age (Jeha 2009)
Combination therapy: 40 mg/m2/day once daily for days 1 to 5 of each cycle in combination with cyclophosphamide and etoposide (Inaba 2012)
Langerhans cell histiocytosis, refractory: Limited data available: Children and Adolescents: IV: 25 mg/m2/day days 1 through 5; repeat every 28 days for 2 to 8 cycles (Simko 2014).
Dosing adjustment for toxicity: Children and Adolescents:
Hematologic toxicity: ANC <500/mm3 lasting ≥4 weeks: Reduce clofarabine dose by 25% for next cycle
Nonhematologic toxicity:
Clinically significant infection: Withhold treatment until infection is under control, then restart clofarabine at full dose
Grade 3 toxicity, excluding infection, nausea, and vomiting, and transient elevations in transaminases and bilirubin: Withhold treatment; may reinitiate clofarabine with a 25% dose reduction with resolution or return to baseline
Grade ≥3 increase in creatinine or bilirubin: Discontinue clofarabine; may reinitiate with 25% dosage reduction when creatinine or bilirubin return to baseline and patient is stable; administer antihyperuricemic therapy for elevated uric acid
Grade 4 toxicity (noninfectious): Discontinue clofarabine treatment
Capillary leak or systemic inflammatory response syndrome (SIRS) early signs/symptoms (eg, hypotension, tachycardia, tachypnea, pulmonary edema): Discontinue clofarabine; institute supportive measures. May consider reinitiating with a 25% dose-reduction after patient is stable and after organ function recovers to baseline.
Dermatologic toxicity: Exfoliative or bullous rash, or suspected Stevens-Johnson syndrome or toxic epidermal necrolysis: Discontinue clofarabine.
Hypotension (during the 5 days of infusion): Discontinue clofarabine. If hypotension is transient and resolves (without pharmacologic intervention), some have suggested that may reinitiate with 25% dosage reduction (Clolar Canadian prescribing information 2014).
Dosing: Adjustment for Toxicity
Hematologic toxicity: ANC <500/mm3 lasting ≥4 weeks: Reduce dose by 25% for next cycle
Nonhematologic toxicity:
Clinically significant infection: Withhold treatment until infection is under control, then restart at full dose
Grade 3 toxicity excluding infection, nausea and vomiting controlled by antiemetics, or transient elevations in transaminases and bilirubin: Withhold treatment; may reinitiate with a 25% dose reduction with resolution or return to baseline
Grade 4 toxicity (noninfectious): Discontinue clofarabine.
Capillary leak or systemic inflammatory response syndrome (SIRS) early signs/symptoms (eg, hypotension, tachycardia, tachypnea, pulmonary edema): Discontinue clofarabine; institute supportive measures. May consider reinitiating with a 25% dose reduction after patient is stable and organ function recovers to baseline.
Dermatologic toxicity: Exfoliative or bullous rash, or suspected Stevens-Johnson syndrome or toxic epidermal necrolysis: Discontinue clofarabine.
Hypotension (during the 5 days of infusion): Discontinue clofarabine.
Dosing: Obesity
American Society for Blood and Marrow Transplantation (ASBMT) practice guideline committee position statement on chemotherapy dosing in obesity: Utilize actual body weight (full weight) for calculation of body surface area in clofarabine dosing for hematopoietic stem cell transplant conditioning regimens (Bubalo 2014).
Reconstitution
Clofarabine should be diluted with NS or D5W to a final concentration of 0.15 to 0.4 mg/mL. Manufacturer recommends the product be filtered through a 0.2 micron filter prior to dilution.
Administration
Clofarabine is associated with a moderate emetic potential; antiemetics are recommended to prevent nausea and vomiting (Hesketh 2017; Roila 2016).
IV infusion: Infuse over 2 hours for relapsed/refractory ALL. May be infused over 1 hour for some off-label protocols (Becker 2011; Kantarjian 2003). Continuous IV fluids are encouraged to decrease adverse events and tumor lysis effects. Hypotension may be a sign of capillary leak syndrome or systemic inflammatory response syndrome (SIRS). Discontinue if the patient becomes hypotensive during administration; may consider therapy reinitiation with a 25% dose reduction after return to baseline. Do not administer any other medications through the same intravenous line.
Storage
Store intact vials at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Solutions diluted for infusion in D5W or NS may be stored for up to 24 hours at room temperature (use within 24 hours of preparation).
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lenograstim: Antineoplastic Agents may diminish the therapeutic effect of Lenograstim. Management: Avoid the use of lenograstim 24 hours before until 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lipegfilgrastim: Antineoplastic Agents may diminish the therapeutic effect of Lipegfilgrastim. Management: Avoid concomitant use of lipegfilgrastim and myelosuppressive cytotoxic chemotherapy. Lipegfilgrastim should be administered at least 24 hours after the completion of myelosuppressive cytotoxic chemotherapy. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitisinone: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Palifermin: May enhance the adverse/toxic effect of Antineoplastic Agents. Specifically, the duration and severity of oral mucositis may be increased. Management: Do not administer palifermin within 24 hours before, during infusion of, or within 24 hours after administration of myelotoxic chemotherapy. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pretomanid: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Teriflunomide: May increase the serum concentration of OAT1/3 Substrates. Monitor therapy
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Tolvaptan: May increase the serum concentration of OAT1/3 Substrates. Management: Patients being treated with the Jynarque brand of tolvaptan should avoid concomitant use of OAT1/3 substrates. Concentrations and effects of the OAT1/3 substrate would be expected to increase with any combined use. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Incidences include off-label use in the treatment of AML.
>10%:
Cardiovascular: Tachycardia (35%), hypotension (29%), flushing (19%), hypertension (13%), edema (12%)
Central nervous system: Headache (43%), chills (34%), fatigue (34%), anxiety (21%), pain (15%)
Dermatologic: Pruritus (43%), skin rash (38%), palmar-plantar erythrodysesthesia (16%), erythema (11%)
Gastrointestinal: Vomiting (78%), nausea (73%), diarrhea (56%), abdominal pain (35%), anorexia (30%), gingival bleeding (17%), mucosal inflammation (16%), oral candidiasis (11%)
Genitourinary: Hematuria (13%)
Hematologic & oncologic: Leukopenia (88%; grades 3/4: 88%), anemia (83%; grades 3/4: 75%), lymphocytopenia (82%; grades 3/4: 82%), thrombocytopenia (81%; grades 3/4: 80%), neutropenia (10% to 64%; grades 3/4: 64%; grade 4: 7%), febrile neutropenia (55%; grade 3: 51%; grade 4: 3%), petechia (26%; grade 3: 6%)
Hepatic: Increased serum ALT (81%), increased serum AST (74%), increased bilirubin (45%)
Infection: Infection (83%; includes bacterial, fungal, and viral), sepsis (including septic shock; 17%)
Local: Catheter infection (12%)
Neuromuscular & skeletal: Limb pain (30%), myalgia (14%)
Renal: Increased serum creatinine (50%)
Respiratory: Epistaxis (27%), dyspnea (13%), pleural effusion (12%)
Miscellaneous: Fever (39%)
1% to 10%:
Cardiovascular: Pericardial effusion (8%), capillary leak syndrome (4%)
Central nervous system: Drowsiness (10%), irritability (10%), lethargy (10%), agitation (5%), mental status changes (1% to 4%)
Dermatologic: Cellulitis (8%), pruritic rash (8%)
Gastrointestinal: Rectal pain (8%), upper abdominal pain (8%), pseudomembranous colitis (7%), stomatitis (7%), pancreatitis (1% to 4%), typhlitis (1% to 4%)
Hematologic & oncologic: Tumor lysis syndrome (6%; grade 3: 6%), oral mucosal petechiae (5%; grade 3: 4%)
Hepatic: Jaundice (8%), hyperbilirubinemia (1% to 4%), hepatic sinusoidal obstruction syndrome (formerly known as hepatic veno-occlusive disease: 2%)
Hypersensitivity: Hypersensitivity (1% to 4%)
Infection: Herpes simplex infection (10%), bacteremia (9%), candidiasis (7%), herpes zoster (7%), staphylococcal bacteremia (6%), staphylococcal sepsis (5%), influenza (1% to 4%), sepsis syndrome (2%)
Neuromuscular & skeletal: Back pain (10%), ostealgia (10%), weakness (10%), arthralgia (9%)
Renal: Acute renal failure
Respiratory: Pneumonia (10%), respiratory distress (10%), tachypnea (9%), upper respiratory tract infection (5%), pulmonary edema (1% to 4%), sinusitis (1% to 4%)
<1%, postmarketing, and/or case reports: Enterocolitis (occurs more frequently within 30 days of treatment and with combination chemotherapy), exfoliative dermatitis, gastrointestinal hemorrhage, hallucination (Jeha 2006), hepatic failure, hepatitis, hepatomegaly (Jeha 2006), hypokalemia (Jeha 2006), hyponatremia, hypophosphatemia, increased right ventricular pressure (Jeha 2006), left ventricular systolic dysfunction (Jeha 2006), major hemorrhage (including cerebral and pulmonary; majority of cases associated with thrombocytopenia), Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Dose-dependent, reversible myelosuppression (neutropenia, thrombocytopenia, and anemia) is common; may be severe and prolonged. Monitor blood counts and platelets. May be at increased risk for infection due to neutropenia. Monitor for signs and symptoms of infection and treat promptly if infection develops; may require discontinuation.
- Capillary leak syndrome/systemic inflammatory response syndrome (SIRS): Cytokine release syndrome (eg, tachypnea, tachycardia, hypotension, pulmonary edema) may develop into capillary leak syndrome/SIRS, and organ dysfunction; immediately discontinue with signs/symptoms of SIRS or capillary leak syndrome (rapid-onset respiratory distress, hypotension, pleural/pericardial effusion, and multiorgan failure) and manage appropriately. Consider supportive treatment with diuretics, corticosteroids, and/or albumin. Prophylactic corticosteroids may prevent or diminish the signs/symptoms of cytokine release. May require dosage reduction.
- Dermatologic reactions: Serious and fatal cases of Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported. Discontinue clofarabine for exfoliative or bullous rash, or if SJS or TEN are suspected.
- Gastrointestinal toxicity: Clofarabine is associated with a moderate emetic potential; antiemetics are recommended to prevent nausea and vomiting (Dupuis 2011; Hesketh 2017; Roila 2016). Serious and fatal enterocolitis (including neutropenic colitis, cecitis, and C. difficile colitis) has been reported, usually occurring within 30 days of treatment, and when used in combination with other chemotherapy. May lead to necrosis, perforation, hemorrhage or sepsis complications. Monitor for signs/symptoms of enterocolitis and manage promptly.
- Hemorrhage: Serious and fatal hemorrhages (including cerebral, gastrointestinal, and pulmonary hemorrhage) have occurred, usually associated with thrombocytopenia. Monitor and manage coagulation parameters.
- Hepatotoxicity: Transaminases and bilirubin may be increased during treatment; hepatitis and hepatic failure have been reported. Transaminase elevations generally occur within 10 days of administration and persist for ≤15 days. In some cases, hepatotoxicity was severe and fatal. The risk for hepatotoxicity, including hepatic sinusoidal obstruction syndrome (SOS; formerly called veno-occlusive disease [VOD]), is increased in patients who have previously undergone a hematopoietic stem cell transplant; discontinue if SOS is suspected. Avoid the concomitant use of drugs that may cause hepatotoxicity. Monitor liver function closely; discontinue immediately for grade ≥ 3 elevations in hepatic enzymes and/or bilirubin.
- Hypotension: Monitor blood pressure during 5 days of treatment; discontinue if hypotension develops. Monitor if on concurrent medications known to affect blood pressure.
- Infection: The risk for infections, including opportunistic infection or sepsis (may be severe or fatal), is increased due to prolonged neutropenia and immunocompromised state. Monitor for signs and symptoms of infection and treat promptly if infection develops; may require therapy discontinuation.
- Renal toxicity: Elevated creatinine, acute renal failure, and hematuria were observed in clinical studies. Infection, sepsis, or tumor lysis syndrome may cause an increased risk of renal toxicity in patients receiving clofarabine. Monitor renal function closely; may require dosage reduction or therapy discontinuation.
- Tumor lysis syndrome/hyperuricemia: Tumor lysis syndrome may occur as a consequence of leukemia treatment, including treatment with clofarabine, usually occurring in the first treatment cycle. May lead to life-threatening acute renal failure; adequate hydration and prophylactic antihyperuricemic therapy throughout treatment will reduce the risk/effects of tumor lysis syndrome; monitor closely.
Disease-related concerns:
- Renal impairment: A pharmacokinetic study demonstrated that systemic exposure increases as creatinine clearance decreases (CrCl <60 mL/minute) (Bonate 2011). Dosage reduction required for CrCl 30 to 60 mL/minute; use with caution in patients with CrCl <30 mL/minute (has not been studied). Minimize the use of drugs known to cause renal toxicity during the 5-day treatment period.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
CBC with differential and platelets (daily during treatment, then 1 to 2 times weekly or as necessary); liver and kidney function (during 5 days of clofarabine administration); coagulation parameters, blood pressure, cardiac function, and respiratory status during infusion; signs and symptoms of tumor lysis syndrome, infection, hepatic sinusoidal obstruction syndrome, enterocolitis, and cytokine release syndrome (tachypnea, tachycardia, hypotension, pulmonary edema); hydration status
Pregnancy
Pregnancy Considerations
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to clofarabine may cause fetal harm.
Evaluate pregnancy status prior to use in females of reproductive potential. Females of reproductive potential should use effective contraception during therapy and for ≥6 months after the last clofarabine dose. Males with female partners of reproductive potential should use effective contraception during therapy and for ≥3 months after the last dose of clofarabine.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience fatigue, nausea, vomiting, diarrhea, flushing, lack of appetite, skin irritation, itching, anxiety, bone pain, muscle pain, joint pain, back pain, painful extremities, mouth irritation, or mouth sores. Have patient report immediately to prescriber signs of infection, signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of bowel problems (black, tarry, or bloody stools; fever; mucus in stools; vomiting; vomiting blood; severe abdominal pain; constipation; or diarrhea), signs of kidney problems (unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain), signs of bleeding (vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding); signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes); shortness of breath, fast breathing, chest pain, fast heartbeat, severe dizziness, passing out, confusion, severe loss of strength and energy, severe headache, vision changes, mood changes, pale skin, redness or irritation of palms or soles of feet, severe abdominal pain, signs of tumor lysis syndrome (fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish), or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.