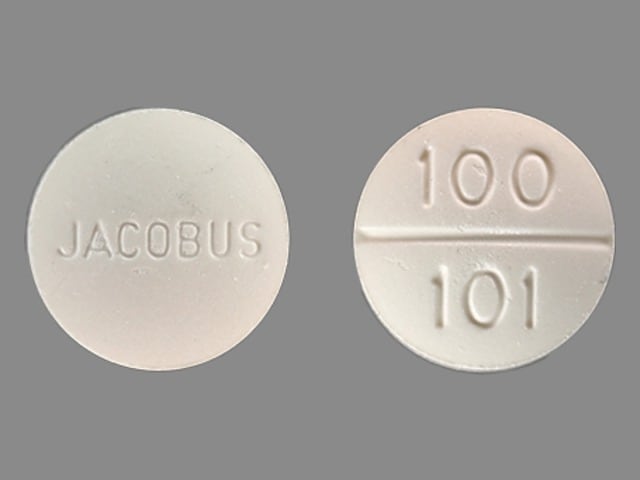
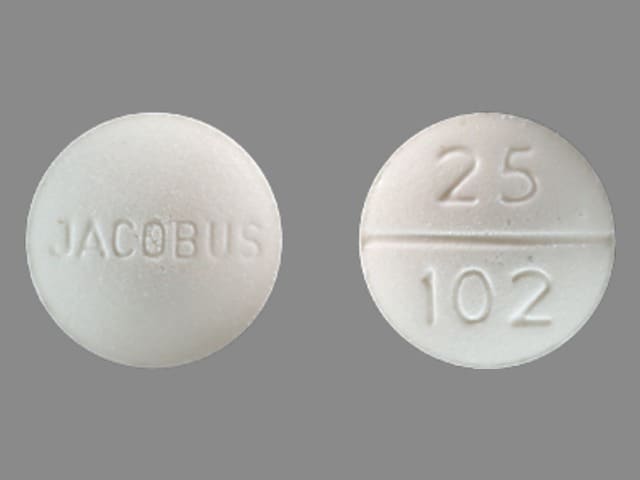
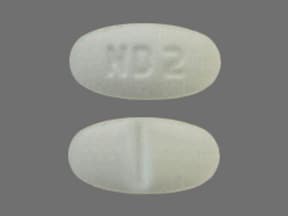
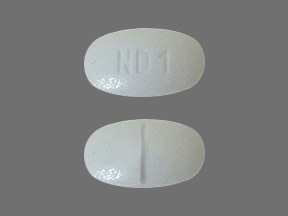
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: 25 mg, 100 mg
Pharmacology
Mechanism of Action
Competitive antagonist of para-aminobenzoic acid (PABA) and prevents normal bacterial utilization of PABA for the synthesis of folic acid
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and almost complete
Distribution
Vd: 1.5 L/kg (Zuidema 1986)
Metabolism
Hepatic (acetylation and hydroxylation); forms multiple metabolites (Zuidema 1986)
Excretion
Urine (~85% as metabolites)
Time to Peak
4 to 8 hours
Half-Life Elimination
Children: 15.1 hours (Mirochnick 1993); Adults: 28 hours (range: 10 to 50 hours)
Protein Binding
Dapsone: 70% to 90%; Metabolite: ~99% (Zuidema 1986)
Use: Labeled Indications
Treatment of leprosy (due to susceptible strains of Mycobacterium leprae) and dermatitis herpetiformis
Use: Off Label
Aphthous ulcers (severe)c
Data from a retrospective review of patients with complex aphthosis treated with either dapsone, colchicine, or the combination Lynde 2009 and a small case series of patients with cicatricial (benign mucous membrane) pemphigoid Rogers 1982 suggest that dapsone may be beneficial for the treatment of severe aphthous ulcers. Additional trials may be necessary to further define the role of dapsone in the treatment of patients with this condition.
Bullous systemic lupus erythematosusc
Clinical experience suggests the utility of dapsone for the treatment of bullous systemic lupus erythematosus Fabbri 2003. Additional data may be necessary to further define the role of dapsone in the treatment of this condition.
Immune thrombocytopeniacyes
Dapsone in the management of refractory or relapsed ITP has been primarily evaluated in noncontrolled settings, demonstrating benefit in approximately half of patients either as complete or partial response. In consensus guidelines, dapsone is recommended as second-line therapy.
Pemphigus vulgaris (oral)c
Data from a small prospective clinical trial in patients with pemphigus vulgaris Azizi 2008 and data from a retrospective review of patients with pemphigus vulgarus Gurcan 2009 suggest that dapsone may be beneficial for the treatment of this condition. Additional data may be necessary to further define the role of dapsone in this condition.
Pneumocystis pneumonia (PCP) prophylaxis in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, dapsone (as monotherapy or in combination with pyrimethamine and leucovorin) is effective and recommended as an alternative agent for primary or secondary prophylaxis of Pneumocystis pneumonia (PCP) in adolescent and adult HIV-infected patients.
Pneumocystis pneumonia (PCP) treatment in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, dapsone is effective and recommended as an alternative agent for mild to moderate Pneumocystis pneumonia (PCP) treatment (in combination with trimethoprim) in adolescent and adult HIV-infected patients.
Relapsing polychondritisc
Data from a limited number of patients (case reports) suggest that dapsone may be beneficial for the treatment of relapsing polychondritis Damiani 1979, Ridgway 1979. Additional data may be necessary to further define the role of dapsone in this condition.
Toxoplasma gondii encephalitis prophylaxis in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, dapsone in combination with pyrimethamine and leucovorin is an effective and recommended alternative regimen for primary prophylaxis of Toxoplasma gondii encephalitis in adolescent and adult HIV-infected patients.
Contraindications
Hypersensitivity to dapsone or any component of the formulation
Dosage and Administration
Dosing: Adult
Dermatitis herpetiformis: Oral: Start at 50 mg daily, increase to 300 mg daily, or higher to achieve full control, reduce to minimum maintenance dosage as soon as possible
Leprosy: Oral:
Tuberculoid (paucibacillary):
National Hansen's Disease Program: 100 mg daily in combination with rifampin for 12 months (NHDP [HRSA 2016]).
World Health Organization: 100 mg daily in combination with rifampin for 6 months (WHO 2012).
Lepromatous (multibacillary):
National Hansen's Disease Program: 100 mg daily in combination with rifampin and clofazimine for 24 months (NHDP [HRSA 2016]).
World Health Organization: 100 mg daily in combination with rifampin and clofazimine for 12 months (WHO 2012).
Aphthous ulcers, severe (off-label use): Oral:
Initial: 25 mg daily for 3 days; increase dose in increments of 25 mg daily every 3 days up to 100 mg daily for 3 days, then increase by 25 mg daily every 7 days up to 150 mg daily. Administer in 2 divided doses (75 mg dose is administered in 3 divided doses).
Maintenance: 100 to 150 mg daily in 2 divided doses with or without concomitant colchicine (Lynde 2009; Rogers 1982)
Bullous systemic lupus erythematosus (off-label use): Oral: 100 mg once daily with or without prednisone (Fabbri 2003).
Immune thrombocytopenia (ITP) (off-label use): Oral: 75 to 100 mg daily or 1 to 2 mg/kg/day; duration of therapy is ≥21 days (Damodar 2005; Godeau 1997; Provan 2010).
Pemphigus vulgaris (off-label use): Oral: 25 mg daily for 7 days, then increase dose in increments of 25 mg daily every 7 days up to 100 mg daily for 7 days (4 weeks total therapy) with concomitant prednisone. Administer in 2 divided doses (a 75 mg dose is administered in 3 divided doses) (Azizi 2008). Note: If patient becomes lesion free, taper and discontinue gradually by decreasing dose 25 mg daily over 7 days. If no new lesions are seen, gradual taper is continued. If lesions recur, dose is increased by 25 mg daily at 7-day intervals until the patient develops no new lesions. Taper is usually ~4 weeks total.
Pneumocystis pneumonia (PCP) in HIV-infected patients (off-label use; HHS [OI adult 2015]): Oral:
Prophylaxis (primary or secondary; alternative to preferred therapy): 100 mg daily once daily or in 2 divided doses as monotherapy or 50 mg daily in combination with weekly pyrimethamine and leucovorin or 200 mg weekly in combination with weekly pyrimethamine and leucovorin
Treatment (mild to moderate disease; alternative to preferred therapy): 100 mg once daily in combination with trimethoprim for 21 days
Toxoplasma gondii encephalitis in HIV-infected patients (alternative to preferred therapy) (off-label use): Primary prophylaxis: Oral: 50 mg daily, in combination with weekly pyrimethamine and leucovorin or 200 mg weekly in combination with weekly pyrimethamine and leucovorin (HHS [OI adult 2015])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Dermatitis herpetiformis: Infants, Children, and Adolescents: Oral: Initial: 0.5 to 2 mg/kg/day in 1 to 2 divided doses (Ermacora 1986; Kliegman 2016); maximum initial daily dose in adults: 50 mg/day; increase dose as needed to achieve control; usual adult dose: 300 mg/dose; once lesions controlled, some have reported that dose may be decreased as tolerated for chronic therapy to a reported range: 0.125 to 0.5 mg/kg/day (Ermacora 1986; Reunala 1984)
Idiopathic thrombocytopenic purpura (ITP), refractory: Limited data available: Children ≥3 years and Adolescents: Oral: 1 to 2 mg/kg/day for at least 2 months. Dosing based on two retrospective reviews. The first was a retrospective cohort analysis of adult and pediatric (age range: 3 to 61 years, including 35 patients <16 years) with chronic ITP (>6 months with diagnosis) who failed steroid therapy and observed an overall similar response rate for children (65.7%) and adults (Damodar 2005). Adverse effects occurred in three patients (one with acute hemolysis and two with an erythematous rash). The second was a small retrospective report of seven pediatric patients with acute or chronic refractory, symptomatic ITP (age range: 6 to 15 years) which also showed a similar response rate (60%); however, a higher incidence (two of seven patients [29%]) of methemoglobinemia was observed (Meeker 2003).
Leprosy (Hansen's disease): Note: Treatment should be managed in consultation with a leprosy expert; use of multidrug therapy is important to prevent drug resistance (Red Book [AAP 2018]). Recommended duration varies:
Paucibacillary (Tuberculoid) leprosy (1 to 5 patches):
National Hansen's Disease Program Recommendations: Infants, Children, and Adolescents: Oral: 1 mg/kg/dose once daily for 12 months; maximum dose: 100 mg/dose; use in combination with rifampin (NHDP [HRSA 2018]).
WHO Recommendations (WHO 2016):
Infants and Children <10 years and weighing <20 kg: Oral: 2 mg/kg/dose once daily for 6 months; use in combination with rifampin
Children ≥10 years and Adolescents ≤14 years:
20 to 40 kg: Oral: 25 mg once daily for 6 months; use in combination with rifampin
>40 kg: Oral: 50 mg once daily for 6 months; use in combination with rifampin
Adolescents >14 years: Oral: 100 mg once daily for 6 months; use in combination with rifampin
Multibacillary (Lepromatous) leprosy (≥6 patches):
National Hansen's Disease Program Recommendations: Infants, Children, and Adolescents: Oral: 1 mg/kg/dose once daily for 24 months; maximum dose: 100 mg/dose; use in combination with rifampin and clofazimine (NHDP [HRSA 2018]).
WHO Recommendations (WHO 2016):
Infants and Children <10 years and weighing <20 kg: Oral: 2 mg/kg/dose once daily for 12 months; use in combination with rifampin and clofazimine
Children ≥10 years and Adolescents ≤14 years:
20 to 40 kg: Oral: 25 mg once daily for 12 months; use in combination with rifampin and clofazimine
>40 kg: Oral: 50 mg once daily for 12 months; use in combination with rifampin and clofazimine
Adolescents >14 years: Oral: 100 mg once daily for 12 months; use in combination with rifampin and clofazimine
Linear IgA bullous dermatosis (LABD): Limited data available: Infants, Children, and Adolescents: Oral: 0.5 to 2 mg/kg/day in 1 to 2 divided doses with or without prednisone (Kenani 2009; Kliegman 2016; Thappa 2003); may increase if needed at weekly intervals until symptoms controlled; maximum reported daily dose: 4 mg/kg/day (Thappa 2003); usual adult dose: 25 to 150 mg/day (Fortuna 2012).
Pneumocystis jirovecii pneumonia (PCP), alternative agent (patients unable to take trimethoprim/sulfamethoxazole):
Prophylaxis (primary or secondary): Multiple regimens (daily or weekly dosing) and combinations presented
HIV-exposed/-positive: Oral:
Infants and Children: 2 mg/kg/dose once daily (maximum daily dose: 100 mg/day) or 4 mg/kg/dose once weekly (maximum weekly dose: 200 mg/week) (HHS [OI pediatric 2016])
Adolescents: 100 mg/day in 1 or 2 divided doses as monotherapy or 50 mg once daily in combination with weekly pyrimethamine and leucovorin or 200 mg once weekly in combination with weekly pyrimethamine and leucovorin; monotherapy should not be used in patients who are seropositive for Toxoplasma gondii (HHS [OI adult 2018])
Hematopoietic stem cell transplant recipient (CDC/IDSA [Tomblyn 2009]): Oral:
Infants and Children: 2 mg/kg/dose once daily; maximum dose: 100 mg/dose
Adolescents: 100 mg/day in 1 or 2 divided doses
Treatment, mild to moderate disease: Limited data available: Infants, Children, and Adolescents (HIV-positive/-exposed): Oral: 2 mg/kg/dose once daily in combination with trimethoprim for 21 days; maximum dose: 100 mg/dose (HHS [OI adult 2018]; HHS [OI pediatric 2016])
Toxoplasma gondii, primary prophylaxis (HIV-exposed/-positive patients); alternative agent (patients unable to tolerate trimethoprim/sulfamethoxazole): Note: Multiple regimens (daily or weekly dosing), combinations, and dosing units (mg/kg, mg/m2) presented; use caution.
Infants and Children: Oral: 2 mg/kg/dose or 15 mg/m2/dose once daily in combination with pyrimethamine and leucovorin; maximum dose: 25 mg/dose (HHS [OI pediatric 2016])
Adolescents: Oral: 50 mg once daily in combination with weekly pyrimethamine and leucovorin or 200 mg once weekly in combination with weekly pyrimethamine and leucovorin (HHS [OI adult 2018])
Extemporaneously Prepared
A 2 mg/mL oral suspension may be made with tablets and a 1:1 mixture of Ora-Sweet® and Ora-Plus®. Crush eight 25 mg tablets in a mortar and reduce to a fine powder. Add small portions of vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 100 mL. Label "shake well". Stable for 90 days at room temperature or refrigerated.
Jacobus Pharmaceutical Company makes a 2 mg/mL proprietary liquid formulation available under an IND for the prophylaxis of Pneumocystis jirovecii pneumonia.
Nahata MC, Morosco RS, and Trowbridge JM, "Stability of Dapsone in Two Oral Liquid Dosage Forms," Ann Pharmacother, 2000, 34(7-8):848-50.10928393
Administration
Oral: Administer with meals if GI upset occurs.
Storage
Store at 20°C to 25°C (68°F to 76°F). Protect from light.
Dapsone (Systemic) Images
Drug Interactions
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Antimalarial Agents: May enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Atazanavir: Dapsone (Systemic) may enhance the adverse/toxic effect of Atazanavir. Specifically, the risk of hyperbilirubinemia may be increased. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Probenecid: May increase the serum concentration of Dapsone (Systemic). Monitor therapy
Rifabutin: May decrease the serum concentration of Dapsone (Systemic). Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Dapsone (Systemic). Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Trimethoprim: May increase the serum concentration of Dapsone (Systemic). Dapsone (Systemic) may increase the serum concentration of Trimethoprim. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Test Interactions
May artificially lower HbA1C by reducing erythrocyte survival time through hemolysis (Lai 2012).
Adverse Reactions
Frequency not always defined.
>10%: Hematologic: Reticulocyte increase (2% to 12%), hemolysis (>10%; dose related; seen in patients with and without G6PD deficiency), hemoglobin decrease (>10%; 1-2 g/dL; almost all patients), methemoglobinemia (>10%), red cell life span shortened (>10%), Agranulocytosis, anemia, leukopenia, pure red cell aplasia (case report)
Cardiovascular: Tachycardia
Central nervous system: Fever, headache, insomnia, psychosis, vertigo
Dermatologic: Bullous and exfoliative dermatitis, erythema nodosum, exfoliative dermatitis, morbilliform and scarlatiniform reactions, phototoxicity, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Hypoalbuminemia (without proteinuria), male infertility
Gastrointestinal: Abdominal pain, nausea, pancreatitis, vomiting
Hepatic: Cholestatic jaundice, hepatitis
Neuromuscular & skeletal: Lower motor neuron toxicity (prolonged therapy), lupus-like syndrome, peripheral neuropathy (rare, nonleprosy patients)
Ophthalmic: Blurred vision
Otic: Tinnitus
Renal: Albuminuria, nephrotic syndrome, renal papillary necrosis
Respiratory: Interstitial pneumonitis, pulmonary eosinophilia
Miscellaneous: Infectious mononucleosis-like syndrome (rash, fever, lymphadenopathy, hepatic dysfunction)
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: Aplastic anemia, agranulocytosis and other severe blood dyscrasias (some fatal) have been reported; monitor for signs/symptoms (eg, fever, sore throat, pallor, purpura, jaundice). Closely monitor CBC and discontinue therapy if a significant reduction in leukocytes, platelets, or hemopoiesis is seen.
- Dermatologic reactions: Serious dermatologic reactions, including toxic erythema, erythema multiforme, toxic epidermal necrolysis, morbilliform and scarlatiniform reactions, urticaria, and erythema nodosum have been reported rarely. Discontinue therapy if new or severe dermatologic reactions occur; leprosy reactional states (eg, erythema nodosum leprosum) do not require discontinuation.
- Hepatic effects: Toxic hepatitis and cholestatic jaundice have been reported; hyperbilirubinemia may occur more frequently in G6PD deficient patients. Monitor liver function; discontinue use if abnormalities occur.
- Peripheral neuropathy: Motor loss and muscle weakness have been reported; discontinue use if symptoms of peripheral neuropathy develop. Recovery after discontinuation is usually complete; some patients may tolerate retreatment at reduced doses.
- Sulfonamide allergy: Use with caution in patients with hypersensitivity to other sulfonamides; sulfone reactions may also occur as potentially fatal hypersensitivity reactions, requiring drug discontinuation.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Anemia: Use with caution in patients with severe anemia; treat prior to therapy.
- Diabetes mellitus: Dapsone may artificially lower HbA1C by reducing erythrocyte survival time through hemolysis (Lai 2012).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- G6PD deficiency: Use with caution in patients with G6PD deficiency; dose-related hemolysis and methemoglobinemia may occur.
- Hemoglobin M deficiency: Use with caution in patients with hemoglobin M deficiency.
- Methemoglobin reductase deficiency: Use with caution in patients with methemoglobin reductase deficiency.
Monitoring Parameters
Check G6PD levels (prior to initiation); CBC (weekly for first month, monthly for 6 months and semiannually thereafter); reticulocyte counts; liver function tests (baseline and periodic). Monitor patients for signs of jaundice, hemolysis, and blood dyscrasias. If the patient is diabetic, consider alternative methods to monitor diabetes control other than HbA1C.
May artificially lower HbA1C by reducing erythrocyte survival time through hemolysis (Lai 2012).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Dapsone crosses the placenta (Brabin 2004). Per the manufacturer, dapsone has not shown an increased risk of congenital anomalies when given during all trimesters of pregnancy. Several reports have described adverse effects in the newborn after in utero exposure to dapsone, including neonatal hemolytic disease, methemoglobinemia, and hyperbilirubinemia (Hocking 1968; Kabra 1998; Thornton 1989). Dapsone may be used in pregnant women requiring maintenance therapy of either leprosy or dermatitis herpetiformis. Dapsone may be used as an alternative agent for management of Pneumocystis jirovecii pneumonia (PCP) or Toxoplasma gondii encephalitis in pregnant, HIV-infected patients (HHS [OI Adult] 2016). Because of the theoretical increased risk for hyperbilirubinemia and kernicterus, neonatal care providers should be informed if maternal dapsone is used near term (HHS [OI Adult] 2016).
Patient Education
What is this drug used for?
- It is used to treat a skin problem called dermatitis herpetiformis.
- It is used to treat leprosy.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Headache
- Abdominal pain
- Trouble sleeping
- Dizziness
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Kidney problems like not able to pass urine, blood in your urine, change in amount of urine passed, or weight gain
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Severe loss of strength and energy
- Burning or numbness feeling
- Muscle weakness
- Difficulty moving
- Blurred vision
- Noise or ringing in the ears
- Mood changes
- Bruising
- Bleeding
- Pale skin
- Fast heartbeat
- Purple spots or redness of skin
- Toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.