Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Darzalex: 100 mg/5 mL (5 mL); 400 mg/20 mL (20 mL) [contains mouse (murine) and/or hamster protein]
Pharmacology
Mechanism of Action
Daratumumab is an IgG1κ human monoclonal antibody directed against CD38. CD38 is a cell surface glycoprotein which is highly expressed on myeloma cells, yet is expressed at low levels on normal lymphoid and myeloid cells (Lokhorst 2015). By binding to CD38, daratumumab inhibits the growth of CD38 expressing tumor cells by inducing apoptosis directly through Fc mediated cross linking as well as by immune-mediated tumor cell lysis through complement dependent cytotoxicity, antibody dependent cell mediated cytotoxicity, and antibody dependent cellular phagocytosis.
Pharmacokinetics/Pharmacodynamics
Distribution
Central: Monotherapy: 4.7 ± 1.3 L; Combination therapy: 4.4 ± 1.5 L
Excretion
Clearance: 171.4 ± 95.3 mL/day
Half-Life Elimination
18 ± 9 days
Use in Specific Populations
Special Populations Note
Body weight: Central volume of distribution and clearance increase with increasing body weight.
Use: Labeled Indications
Multiple myeloma (newly diagnosed):
Treatment of newly diagnosed multiple myeloma (in combination with bortezomib, thalidomide, and dexamethasone) in adults who are eligible for autologous stem cell transplant.
Treatment of newly diagnosed multiple myeloma (in combination with bortezomib, melphalan, and prednisone) in adults who are ineligible for autologous stem cell transplant.
Treatment of newly diagnosed multiple myeloma (in combination with lenalidomide and dexamethasone) in adults who are ineligible for autologous stem cell transplant.
Multiple myeloma (relapsed/refractory):
Treatment of multiple myeloma (in combination with dexamethasone and lenalidomide) in adults who have received at least 1 prior therapy.
Treatment of multiple myeloma (in combination with dexamethasone and bortezomib) in adults who have received at least 1 prior therapy.
Treatment of multiple myeloma (in combination with dexamethasone and pomalidomide) in adults who have received at least 2 prior therapies, including lenalidomide and a proteasome inhibitor.
Treatment of multiple myeloma (as monotherapy) in adults who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent or who are double refractory to a proteasome inhibitor and an immunomodulatory agent.
Contraindications
History of severe hypersensitivity (eg, anaphylactic reactions) to daratumumab or any component of the formulation.
Dosage and Administration
Dosing: Adult
Note: Premedicate 1 to 3 hours prior to each infusion with a corticosteroid, an oral antipyretic, and an oral or IV antihistamine (see Premedications below). Post-infusion, administer an oral corticosteroid to all patients to reduce the risk of delayed infusion reactions (see Postinfusion medications below). To prevent herpes zoster reactivation, initiate antiviral prophylaxis within 1 week after starting daratumumab and continue for 3 months following completion of treatment. Per the manufacturer, daratumumab dosing should be based on actual body weight.
The initial daratumumab dose (16 mg/kg on week 1) may be divided over 2 consecutive days (by administering 8 mg/kg/day on days 1 and 2 of week 1 of therapy) to facilitate administration.
Multiple myeloma (newly diagnosed): IV: Note: Refer to specific protocol or to dexamethasone, lenalidomide, thalidomide, bortezomib, melphalan, and/or prednisone monographs for dosing when used in combination with daratumumab.
In combination with bortezomib, melphalan, and prednisone (D-VMP regimen; in patients ineligible for autologous stem cell transplant) (Mateos 2018):
Weeks 1 to 6: 16 mg/kg once weekly for 6 doses
Weeks 7 to 54: 16 mg/kg once every 3 weeks for 16 doses
Weeks 55 and beyond: 16 mg/kg once every 4 weeks until disease progression
In combination with lenalidomide and low-dose dexamethasone (DRd regimen; in patients ineligible for autologous stem cell transplant) (Facon 2019):
Weeks 1 to 8: 16 mg/kg once weekly for 8 doses
Weeks 9 to 24: 16 mg/kg once every 2 weeks for 8 doses
Weeks 25 and beyond: 16 mg/kg once every 4 weeks until disease progression
In combination with thalidomide, bortezomib, and dexamethasone (DVTd regimen; in patients eligible for autologous stem cell transplant) (Moreau 2019):
Induction:
Weeks 1 to 8: 16 mg/kg once weekly for 8 doses.
Weeks 9 to 16: 16 mg/kg once every 2 weeks for 4 doses.
Consolidation (following autologous stem cell transplant):
Weeks 1 to 8: 16 mg/kg once every 2 weeks for 4 doses.
Multiple myeloma (relapsed/refractory): IV: Note: Refer to specific protocol or to dexamethasone, lenalidomide, bortezomib, and/or pomalidomide monographs for dosing when used in combination with daratumumab.
Monotherapy:
Weeks 1 to 8: 16 mg/kg once weekly for 8 doses
Weeks 9 to 24: 16 mg/kg once every 2 weeks for 8 doses
Weeks 25 and beyond: 16 mg/kg once every 4 weeks until disease progression
In combination with lenalidomide and low-dose dexamethasone (DRd regimen; Dimopoulos 2016):
Weeks 1 to 8: 16 mg/kg once weekly for 8 doses
Weeks 9 to 24: 16 mg/kg once every 2 weeks for 8 doses
Weeks 25 and beyond: 16 mg/kg once every 4 weeks until disease progression
In combination with pomalidomide and low-dose dexamethasone (DPd regimen; Chari 2017):
Weeks 1 to 8: 16 mg/kg once weekly for 8 doses
Weeks 9 to 24: 16 mg/kg once every 2 weeks for 8 doses
Weeks 25 and beyond: 16 mg/kg once every 4 weeks until disease progression
In combination with bortezomib and dexamethasone (DVd regimen; Palumbo 2016):
Weeks 1 to 9: 16 mg/kg once weekly for 9 doses
Weeks 10 to 24: 16 mg/kg once every 3 weeks for 5 doses
Weeks 25 and beyond: 16 mg/kg once every 4 weeks until disease progression
Missed dose: If a dose is missed, administer as soon as possible and adjust the schedule accordingly (maintain the treatment interval).
Premedications: Administer 1 to 3 hours prior to each infusion. If dexamethasone is the background regimen-specific corticosteroid, the dexamethasone treatment dose will serve as the corticosteroid premedication on daratumumab infusion days. Additional background regimen-specific corticosteroids (eg, prednisone) should NOT be administered on daratumumab infusion days when patients receive dexamethasone (or equivalent) as a premedication.
Corticosteroid:
Monotherapy: Methylprednisolone 100 mg IV or equivalent intermediate- or long-acting corticosteroid; following the second infusion, the dose may be decreased (eg, methylprednisolone 60 mg [IV or oral] or equivalent)
Combination therapy: Dexamethasone 20 mg (or equivalent) prior to each daratumumab infusion; administer IV prior to the first infusion; oral administration may be considered prior to subsequent infusions plus
Antipyretic: Oral: Acetaminophen 650 to 1,000 mg plus
Antihistamine: IV or Oral: Diphenhydramine 25 to 50 mg or equivalent
The following premedication regimen has also been reported (Hofmeister 2016):
First infusion: Acetaminophen 325 mg orally, diphenhydramine 25 mg orally or IV, dexamethasone 20 mg IV, montelukast 10 mg orally, and famotidine 20 mg IV.
Subsequent infusions: Acetaminophen 325 mg orally, diphenhydramine 25 mg IV, and dexamethasone 20 mg IV.
Postinfusion medication:
Monotherapy: Administer an oral intermediate- or long-acting corticosteroid (eg, methylprednisolone 20 mg or equivalent) on the first and second day after all daratumumab infusions.
Combination therapy: Consider administering low-dose oral methylprednisolone (≤20 mg) or equivalent on the first day after the daratumumab infusion. If dexamethasone or prednisone is administered the day after the daratumumab infusion as part of background combination chemotherapy regimen, additional postinfusion corticosteroid therapy may not be necessary.
In patients with a history of chronic obstructive pulmonary disease, also consider short- and long-acting bronchodilators and inhaled corticosteroids postinfusion. If no major infusion reactions occur during the first 4 daratumumab infusions, these additional inhaled postinfusion medications may be discontinued.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Note: Refer to specific protocol or to dexamethasone, prednisone, lenalidomide, thalidomide, bortezomib, melphalan, or pomalidomide monographs for dosing adjustment for toxicity when used in combination with daratumumab.
Hematologic toxicity: No dose reductions of daratumumab are recommended; delay of daratumumab infusion may be required to allow for neutrophil and/or platelet recovery. Supportive care with growth factors and/or platelet transfusions may be necessary.
Infusion reactions: Immediately interrupt infusion for reaction of any severity. Manage symptoms as clinically appropriate.
Grade 1 or 2 (mild to moderate) infusion reaction: Once symptoms resolve, resume the infusion at no more than 50% of the rate at which the reaction occurred. If no further reactions are observed, may escalate the infusion rate as appropriate up to the maximum rate of 200 mL/hour (see Administration).
Grade 3 (severe) infusion reaction: Once symptoms resolve, consider resuming the infusion at no more than 50% of the rate at which the reaction occurred. If no further reactions are observed, may escalate the infusion rate as appropriate (see Administration). If a grade 3 reaction recurs, repeat the steps above. Permanently discontinue if a grade 3 infusion reaction occurs for the third time.
Grade 4 (anaphylactic reaction or life-threatening) infusion reaction: Permanently discontinue.
Reconstitution
Determine the appropriate dose and volume of daratumumab required (based on patient's actual body weight); daratumumab should be colorless to pale yellow (do not use if opaque particles, discoloration, or other foreign particles are observed). Remove the volume of 0.9% sodium chloride injection from the infusion bag that is equal to the required volume of the daratumumab dose. Add the appropriate daratumumab volume to a 500 mL or 1,000 mL 0.9% sodium chloride bag; dilution volume depends on dose (single dose vs split dose, or if initial vs subsequent dose). Gently invert to mix (do not shake). Infusion bags/containers must be made of polyvinylchloride (PVC), polypropylene (PP), polyethylene (PE), or polyolefin blend (PP+PE). If the diluted solution is refrigerated prior to use, allow to come to room temperature before administration. After dilution, may develop very small translucent to white proteinaceous particles; do not use if discolored or if visibly opaque or foreign particles are observed.
Administration
IV: For IV infusion only. Do not administer IV push or as a bolus. Premedicate with a corticosteroid, acetaminophen, and an IV or oral antihistamine (see Dosing) 1 to 3 hours prior to administration. Infuse in an environment equipped to monitor for and manage infusion reactions. Administer with an infusion set fitted with a flow regulator and with an inline, sterile, non-pyrogenic, low protein-binding polyethersulfone filter (0.22 or 0.2 micrometer). Polyurethane, polybutadiene, polyvinylchloride, polypropylene, or polyethylene administration sets are required. Do not mix with or infuse with other medications.
The manufacturer recommends not exceeding first, second, and subsequent infusion rates listed below. Begin infusion immediately after infusion bag reaches room temperature (if refrigerated). Infusion should be completed within 15 hours. Interrupt infusion for any severity of infusion reaction; if the reaction resolves, may resume infusion (see Dosage Adjustment for Toxicity). If infusion cannot be completed, do not save unused portion for reuse. Postinfusion, administer an oral corticosteroid to all patients to reduce the risk of delayed infusion reactions (see Dosing). In patients with a history of obstructive pulmonary disorder, consider short- and long-acting bronchodilators and inhaled corticosteroids post-infusion.
Infusion rate:
Week 1 infusion (500 mL [split-dose infusion; 8 mg/kg/day over 2 consecutive days] or 1,000 mL volume [single-dose infusion; 16 mg/kg on day 1]): Infuse at 50 mL/hour for the first hour. If no infusion reactions occur, may increase the rate by 50 mL/hour every hour (maximum rate: 200 mL/hour).
Week 2 infusion (500 mL volume; 16 mg/kg): Use a dilution volume of 500 mL only if there were no infusion reactions during the previous week's infusion. Otherwise, continue to use a dilution volume of 1,000 mL. Infuse at 50 mL/hour for the first hour. If no infusion reactions occur, may increase the rate by 50 mL/hour every hour (maximum rate: 200 mL/hour).
Subsequent infusions (500 mL volume; 16 mg/kg): Use a modified initial rate for subsequent infusions (week 3 onwards) only if there were no infusion reactions during the previous infusion. Otherwise, continue to use instructions for the week 2 infusion. Infuse at 100 mL/hour for the first hour. If no infusion reactions occur, may increase the rate by 50 mL/hour every hour (maximum rate: 200 mL/hour).
Accelerated infusion rate (off-label) (Barr 2018): An accelerated infusion rate was studied (small, single-center study) in patients who have received 2 or more daratumumab doses at the standard infusion rate. Twenty percent of the dose was infused over 30 minutes (200 mL/hour) and the remaining 80% of the dose was then infused over 60 minutes (450 mL/hour), delivering the dose over a total of ~90 minutes. Standard existing premedications were continued (montelukast and famotidine were included in the premedication regimen), but may be tapered over subsequent infusions if tolerated (refer to protocol for details). Vital signs were monitored prior to infusion, every 15 minutes for the first hour, and then at the end of infusion; patients were observed for signs/symptoms of infusion reaction for 30 minutes after the initial accelerated infusion was completed. Prior to implementing the accelerated infusion rate, patients should demonstrate tolerability to a 500 mL infusion.
Storage
Store intact vials at 2°C to 8°C (36°F to 46°F). Do not freeze or shake; protect from light. Solutions diluted for infusion should be administered immediately at room temperature and in room light; diluted solution may be kept at room temperature for a maximum of 15 hours (including infusion time). If not used immediately, solutions diluted for infusion may be stored for up to 24 hours at 2°C to 8°C (36°F to 46°F) and protected from light; do not freeze. Discard any unused portion of the solution.
Drug Interactions
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Test Interactions
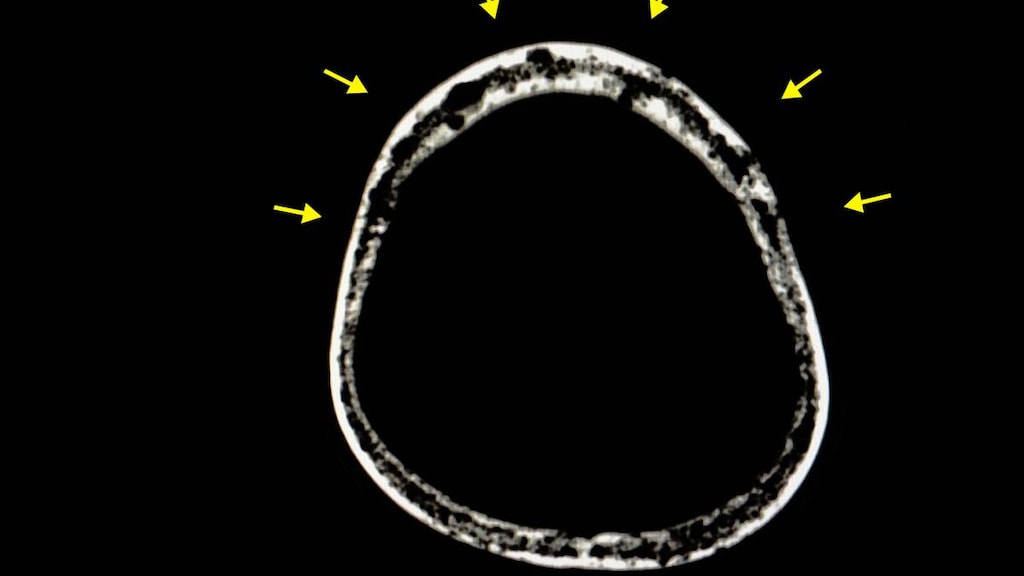
Daratumumab binds to CD38 on RBCs and interferes with compatibility testing, including antibody screening and cross matching. Mitigation methods include treating reagent RBCs with dithiothreitol (DTT) to disrupt daratumumab binding or genotyping. As the Kell blood group system is also sensitive to DTT, K-negative units should be supplied after ruling out or identifying alloantibodies using DTT-treated RBCs. If an emergency transfusion is required, non-cross-matched ABO/RhD-compatible RBCs can be used per local blood bank practices.
Daratumumab may be detected on both serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for monitoring multiple myeloma monoclonal immunoglobulins (M-proteins); false positive SPE and IFE assay results may occur for patients with IgG kappa myeloma protein, and may affect initial assessment of complete response criteria. In patients with persistent very good partial response where daratumumab interference is suspected, consider using a daratumumab-specific IFE assay to distinguish daratumumab from any residual endogenous M protein to evaluate the depth of treatment response.
Adverse Reactions
>10%:
Central nervous system: Fatigue (39%), headache (12%)
Gastrointestinal: Nausea (27%), diarrhea (16%), constipation (15%), decreased appetite (15%), vomiting (14%)
Hematologic & oncologic: Lymphocytopenia (72%; grade: 3: 30%; grade 4: 10%), neutropenia (60%; grade 3: 17%; grade 4: 3%), thrombocytopenia (48%; grade 3: 10%; grade 4: 8%), anemia (45%; grade 3: 19%)
Neuromuscular & skeletal: Back pain (23%), arthralgia (17%), limb pain (15%), musculoskeletal chest pain (12%)
Respiratory: Cough (21%), upper respiratory tract infection (20%), nasal congestion (17%), dyspnea (15%), nasopharyngitis (15%), pneumonia (11%)
Miscellaneous: Infusion related reaction (48%), fever (21%)
1% to 10%:
Cardiovascular: Hypertension (10%)
Central nervous system: Chills (10%)
Infection: Herpes zoster infection (3%)
Miscellaneous: Physical health deterioration (3%)
<1%: Antibody development, reactivation of HBV
Frequency not defined: Hematologic & oncologic: Positive indirect Coombs test
Postmarketing: Anaphylaxis
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Daratumumab may increase neutropenia and thrombocytopenia when used in combination with other chemotherapy agents for the treatment of multiple myeloma. Lymphopenia, neutropenia, thrombocytopenia, and anemia (including grade 3 and 4 toxicity) were commonly reported as treatment emergent adverse reactions in clinical trials. Monitor for signs/symptoms of infection and bleeding. Monitor CBCs periodically; may require delay of daratumumab infusion to allow for neutrophil and/or platelet recovery. Supportive care with growth factors and/or platelet transfusions may be necessary.
- Hepatitis B virus reactivation: Hepatitis B virus (HBV) reactivation has been reported rarely; some cases have been fatal. Monitor for signs/symptoms of HBV reactivation. Consider HBV screening prior to beginning therapy in patients with risk factors for HBV infection (eg, birthplace in a country with ≥2% HBV prevalence, household or sexual contact with HBV-infected patients, high-risk behaviors [eg, intravenous drug use], HIV infection) (ASCO [Hwang 2015]).
- Infusion reactions: Severe and/or serious infusion reactions may occur (including anaphylactic reactions, bronchospasm, hypoxia, dyspnea, hypertension, laryngeal edema, and pulmonary edema), mostly during the first infusion. Signs and symptoms include cough, throat irritation, and nasal congestion, as well as chills, vomiting, and nausea. Less commonly reported symptoms include wheezing, allergic rhinitis, pyrexia, chest discomfort, pruritus, and hypotension. Infusion reactions were reported in approximately 50% of patients in clinical trials, and most reactions were grade 1 or 2. Reactions may also be seen during subsequent infusions, and generally occur either during the infusion or within 4 hours of completion; some reactions occurred up to 48 hours after the infusion. Premedication with antihistamines, antipyretics, and corticosteroids is required; interrupt infusion for any reaction and manage as appropriate. The addition of montelukast and famotidine to the premedication regimen has also been reported (Barr 2018; Hofmeister 2016). Reduce the infusion rate for grade 1, 2, or 3 reaction; permanently discontinue therapy for an anaphylactic reaction or life-threatening grade 4 infusion reaction and treat with appropriate emergency care. Administer in a facility with immediate access to resuscitative measures (eg, glucocorticoids, epinephrine, bronchodilators, and/or oxygen). Administer oral corticosteroids to all patients after daratumumab infusion to reduce the risk of delayed infusion reactions. Also consider short- and long-acting bronchodilators and inhaled corticosteroids for patients with chronic obstructive pulmonary disease; monitor closely.
Disease-related concerns:
- Interference with determination of myeloma response: Daratumumab (a human IgG kappa monoclonal antibody) may be detected on serum protein electrophoresis and immunofixation assays that monitor for endogenous M-protein. Interference with these assays by daratumumab may affect the determination of complete response and disease progression in some patients with IgG kappa myeloma protein.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Interference with serological testing: Through binding to CD38 on red blood cells, daratumumab use may result in a positive indirect antiglobulin test (indirect Coombs test). Daratumumab-mediated Coombs test positivity may persist for up to 6 months after the last infusion. In addition, daratumumab (bound to red blood cells) masks antibody detection to minor antigens in the patient's serum; ABO and Rh blood type determination are not affected. Notify blood transfusion centers and blood banks that a patient has received daratumumab, and type and screen patients prior to therapy initiation.
Monitoring Parameters
CBCs periodically; type and screen (blood type) prior to initiating therapy. Consider hepatitis B virus (HBV) screening prior to beginning therapy in patients with risk factors for HBV infection (eg, birthplace in a country with ≥2% HBV prevalence, household or sexual contact with HBV-infected patients, high-risk behaviors [eg, IV drug use], HIV infection) (ASCO [Hwang 2015]). Monitor for signs/symptoms of anaphylactic reaction and infusion reactions. Monitor for signs/symptoms of HBV reactivation, infection, and bleeding.
Accelerated infusion rate (off-label): Monitor vital signs prior to infusion, every 15 minutes for the first hour, and then at the end of infusion; patients were observed for signs/symptoms of infusion reaction for 30 minutes after the initial accelerated infusion was completed (Barr 2018).
Pregnancy
Pregnancy Considerations
Daratumumab is a humanized monoclonal antibody (IgG1). Potential placental transfer of human IgG is dependent upon the IgG subclass and gestational age, generally increasing as pregnancy progresses. The lowest exposure would be expected during the period of organogenesis (Palmeira 2012; Pentsuk 2009).
Based on the mechanism of action, daratumumab may cause myeloid or lymphoid cell depletion and decreased bone density in the fetus. The administration of live vaccines should be deferred for neonates and infants exposed to daratumumab in utero until a hematology evaluation can be completed.
Females of reproductive potential should use effective contraception during therapy and for 3 months after treatment is complete.
Patient Education
What is this drug used for?
- It is used to treat multiple myeloma.
Frequently reported side effects of this drug
- Back pain
- Joint pain
- Painful extremities
- Common cold symptoms
- Nose irritation
- Throat irritation
- Diarrhea
- Vomiting
- Nausea
- Muscle spasms
- Constipation
- Trouble sleeping
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Infusion reaction
- Shortness of breath
- Dizziness
- Passing out
- Headache
- Stuffy nose
- Runny nose
- Chest pain
- Severe loss of strength and energy
- Swelling of arms or legs
- Burning or numbness feeling
- Bruising
- Bleeding
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.