Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Extended Release 24 Hour, Oral:
Enablex: 7.5 mg, 15 mg
Generic: 7.5 mg, 15 mg
Pharmacology
Mechanism of Action
Selective antagonist of the M3 muscarinic (cholinergic) receptor subtype. Blockade of the receptor limits bladder contractions, reducing the symptoms of bladder irritability/overactivity (urge incontinence, urgency and frequency).
Pharmacokinetics/Pharmacodynamics
Distribution
Vdss: ~163 L
Metabolism
Hepatic, via CYP3A4 and CYP2D6
Excretion
Urine (~60%), feces (40%); as metabolites (inactive)
Time to Peak
Plasma: ~7 hours
Half-Life Elimination
~13 to 19 hours
Protein Binding
~98% (primarily alpha1-acid glycoprotein)
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Unbound darifenacin exposure was estimated to be 4.7-fold higher in patients with moderate hepatic impairment.
Special Populations: Elderly
Clearance decreases 6% per decade relative to a median age of 44 years. Exposure at steady state was ~12% to 19% higher in subjects 45 to 65 years of age.
Special Populations: Gender
Cmax and AUC were ~57% to 79% and 61%to 73% higher, respectively, in women than in men.
Use: Labeled Indications
Overactive bladder: Treatment of overactive bladder with symptoms of urinary frequency, urgency, or urge incontinence.
Contraindications
Patients with or at risk of uncontrolled narrow-angle glaucoma, urinary retention, gastric retention
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to darifenacin or any component of the formulation.
Dosage and Administration
Dosing: Adult
Overactive bladder: Oral: Initial: 7.5 mg once daily. If response is not adequate after a minimum of 2 weeks, dosage may be increased to 15 mg once daily.
Dosage adjustment with concomitant potent CYP3A4 inhibitors (eg, ketoconazole, itraconazole, ritonavir, nelfinavir, clarithromycin, nefazodone): Maximum dose: 7.5 mg/day.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer with water without regard to food. Swallow tablet whole; do not chew, crush, or divide.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
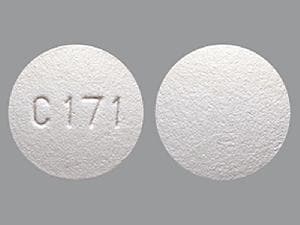
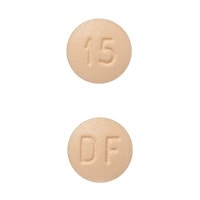
Darifenacin Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ajmaline: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Ajmaline. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amphetamines: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Amphetamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: If brexpiprazole is to be used together with both a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor, the brexpiprazole dose should be reduced to 25% of the usual dose. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of CloZAPine. Monitor therapy
Codeine: CYP2D6 Inhibitors (Moderate) may diminish the therapeutic effect of Codeine. These CYP2D6 inhibitors may prevent the metabolic conversion of codeine to its active metabolite morphine. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Moderate) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Tamoxifen. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Eliglustat: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a moderate CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Indoramin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Indoramin. Monitor therapy
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Metoprolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Metoprolol. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nebivolol: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Nebivolol. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Perhexiline: CYP2D6 Inhibitors may increase the serum concentration of Perhexiline. Management: Consider alternatives to this combination if possible. If combined, monitor for increased perhexiline serum concentrations and toxicities (eg, hypoglycemia, neuropathy, liver dysfunction). Perhexiline dose reductions will likely be required. Consider therapy modification
Pitolisant: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Pitolisant. Monitor therapy
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Propafenone: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tamoxifen: CYP2D6 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Management: Consider alternatives with less of an inhibitory effect on CYP2D6 activity when possible. Consider therapy modification
Tamsulosin: CYP2D6 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thioridazine: CYP2D6 Inhibitors may increase the serum concentration of Thioridazine. Avoid combination
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
TraMADol: CYP2D6 Inhibitors (Moderate) may diminish the therapeutic effect of TraMADol. These CYP2D6 inhibitors may prevent the metabolic conversion of tramadol to its active metabolite that accounts for much of its opioid-like effects. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
>10%: Gastrointestinal: Xerostomia (19% to 35%), constipation (15% to 21%)
1% to 10%:
Cardiovascular: Hypertension (≥1%), peripheral edema (≥1%)
Central nervous system: Headache (7%), dizziness (<2%), pain (≥1%)
Dermatological: Pruritus (≥1%), skin rash (≥1%), xeroderma (≥1%)
Endocrine & metabolic: Weight gain (≥1%)
Gastrointestinal: Dyspepsia (3% to 8%), abdominal pain (2% to 4%), nausea (2% to 4%), vomiting (≥1%)
Genitourinary: Urinary tract infection (4% to 5%), vaginitis (≥1%), urinary retention (acute)
Neuromuscular & skeletal: Weakness (<3%), arthralgia (≥1%), back pain (≥1%)
Ophthalmic: Dry eye syndrome (2%), visual disturbance (≥1%)
Respiratory: Flu-like symptoms (1% to 3%), bronchitis (≥1%), pharyngitis (≥1%), rhinitis (≥1%), sinusitis (≥1%)
Postmarketing and/or case reports: Anaphylaxis, angioedema, confusion, erythema multiforme, granuloma (annulare), hallucination, hypersensitivity reaction, palpitations
Warnings/Precautions
Concerns related to adverse effects:
- Angioedema: Angioedema involving the face, lips, tongue, and/or larynx have been reported; some cases have occurred after the first dose. May be life-threatening. Immediately discontinue and institute supportive care if tongue, hypopharynx, or larynx is involved.
- CNS effects: CNS effects have been reported (eg, headache, confusion, hallucinations, somnolence); monitor for CNS effects, particularly at treatment initiation or dose increase; reduce dose or discontinue if necessary. May cause drowsiness and/or blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Heat prostration: May occur in the presence of increased environmental temperature; use caution in hot weather and/or exercise.
Disease-related concerns:
- Bladder flow obstruction: Use with caution in patients with bladder flow obstruction; may increase the risk of urinary retention.
- Gastrointestinal disease: Use with caution in patients with decreased GI motility (severe constipation, ulcerative colitis) or GI obstructive disorders ( pyloric stenosis); may increase the risk of gastric retention.
- Glaucoma: Use with caution in patients with controlled (treated) narrow-angle glaucoma.
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage adjustment required in moderate hepatic impairment (Child-Pugh class B). Not recommended for use in severe hepatic impairment (Child-Pugh class C).
- Myasthenia gravis: Use with caution in patients with myasthenia gravis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Anticholinergic effects (eg, CNS effects [headache, confusion, hallucinations, somnolence], fixed and dilated pupils, blurred vision, tremors, dry skin); hepatic function.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat an overactive bladder.
Frequently reported side effects of this drug
- Heartburn
- Dry mouth
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Severe headache
- Dizziness
- Passing out
- Confusion
- Sensing things that seem real but are not
- Severe fatigue
- Severe constipation
- Severe abdominal pain
- Unable to pass urine
- Vision changes
- Lack of sweating
- Severe nausea
- Severe vomiting
- Loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.