Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Sprycel: 20 mg, 50 mg, 70 mg, 80 mg, 100 mg, 140 mg
Pharmacology
Mechanism of Action
Dasatinib is a BCR-ABL tyrosine kinase inhibitor that targets most imatinib-resistant BCR-ABL mutations (except the T315I and F317V mutants) by distinctly binding to active and inactive ABL-kinase. Kinase inhibition halts proliferation of leukemia cells. It also inhibits SRC family (including SRC, LKC, YES, FYN); c-KIT, EPHA2 and platelet derived growth factor receptor (PDGFRβ).
Pharmacokinetics/Pharmacodynamics
Distribution
2,505 L
Metabolism
Hepatic (extensive); metabolized by CYP3A4 (primarily), flavin-containing mono-oxygenase-3 (FOM-3) and uridine diphosphate-glucuronosyltransferase (UGT) to an active metabolite and other inactive metabolites (the active metabolite plays only a minor role in the pharmacology of dasatinib)
Excretion
Feces (~85%, 19% as unchanged drug); urine (~4%, 0.1% as unchanged drug)
Time to Peak
0.5 to 6 hours
Half-Life Elimination
Terminal: 3 to 5 hours (adults); 2 to 5 hours (pediatrics)
Protein Binding
Dasatinib: ~96%; metabolite (active): 93%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Patients with moderate hepatic impairment (Child-Pugh class B) had decreases in dose-normalized Cmax and AUC by 47% and 8%, respectively, compared to subjects with normal hepatic function. Patients with severe hepatic impairment (Child-Pugh class C) had decreases in dose-normalized Cmax and AUC of 43% and 28%, respectively, compared with healthy controls.
Use: Labeled Indications
Acute lymphoblastic leukemia:
Adult: Treatment of Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL) in adult patients with resistance or intolerance to prior therapy.
Pediatric: Treatment of newly diagnosed Ph+ ALL (in combination with chemotherapy) in pediatric patients ≥1 year of age.
Chronic myeloid leukemia:
Adult: Treatment of newly diagnosed Ph+ chronic myeloid leukemia (CML) in chronic phase; treatment of chronic, accelerated, or myeloid or lymphoid blast phase Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
Pediatric: Treatment of Ph+ CML in chronic phase in pediatric patients ≥1 year of age.
Use: Off Label
Gastrointestinal stromal tumor (GIST)b
Data from two phase II studies support the use of dasatinib for the treatment of GIST Montemurro 2012, Trent 2011.
Contraindications
There are no contraindications listed in the manufacturer's US labeling.
Canadian labeling: Hypersensitivity to dasatinib or any other component of the formulation; breast-feeding
Dosage and Administration
Dosing: Adult
Note: The effect of discontinuation on long-term disease outcome after achieving cytogenetic response (including complete cytogenetic response) or major molecular response is not known.
Acute lymphoblastic leukemia (ALL), Philadelphia chromosome-positive (Ph+): Oral: 140 mg once daily until disease progression or unacceptable toxicity occurs. Consider a dose escalation to 180 mg once daily in patients not achieving hematologic or cytogenetic response at recommended initial dosage.
Chronic myelogenous leukemia (CML), Ph+, newly diagnosed in chronic phase: Oral: 100 mg once daily until disease progression or unacceptable toxicity occurs. Consider a dose escalation to 140 mg once daily in patients not achieving hematologic or cytogenetic response at recommended initial dosage.
CML, Ph+, resistant or intolerant: Oral:
Chronic phase: 100 mg once daily until disease progression or unacceptable toxicity occurs. Consider a dose escalation to 140 mg once daily in patients not achieving hematologic or cytogenetic response at recommended initial dosage.
Accelerated or blast phase: 140 mg once daily until disease progression or unacceptable toxicity occurs. Consider a dose escalation to 180 mg once daily in patients not achieving hematologic or cytogenetic response at recommended initial dosage.
Gastrointestinal stromal tumors (GIST; off-label use): Oral: 70 mg twice daily (Montemurro 2012; Trent 2011).
Missed doses: If a dose is missed, take the next regularly scheduled dose; 2 doses should not be taken at the same time.
Dosage adjustment for concomitant strong CYP3A4 inhibitors: Avoid concomitant administration with strong CYP3A4 inhibitors and grapefruit juice; if concomitant administration with a strong CYP3A4 inhibitor cannot be avoided, consider reducing dasatinib from 140 mg once daily to 40 mg once daily or from 100 mg once daily to 20 mg once daily or from 70 mg once daily to 20 mg once daily, with careful monitoring. If taking dasatinib 60 mg or 40 mg once daily, consider withholding dasatinib until the strong CYP3A4 inhibitor is discontinued; allow a washout period of ~1 week prior to reinitiating dasatinib. If reduced dasatinib dose is not tolerated, either discontinue the strong CYP3A4 inhibitor or interrupt dasatinib therapy temporarily until the concomitant inhibitor use is discontinued. When a strong CYP3A4 inhibitor is discontinued, allow a washout period of ~1 week prior to adjusting dasatinib dose upward.
Dosage adjustment for concomitant strong CYP3A4 inducers: Avoid concomitant administration with strong CYP3A4 inducers and St John's wort; if concomitant administration with a strong CYP3A4 inducer cannot be avoided, consider increasing the dasatinib dose with careful monitoring.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Acute lymphoblastic leukemia (ALL), Philadelphia chromosome-positive (Ph+), newly diagnosed: Note: Use in combination with chemotherapy; dose escalation is not recommended; initiate dasatinib on or before day 15 of induction chemotherapy. Continue treatment for 2 years. Recalculate the dose every 3 months or as clinically necessary based on changes in body weight.
Children weighing ≥10 kg and Adolescents: Oral:
10 to <20 kg: 40 mg once daily
20 to <30 kg: 60 mg once daily
30 to <45 kg: 70 mg once daily
≥45 kg: 100 mg once daily
Chronic myelogenous leukemia (CML), Philadelphia chromosome-positive (Ph+), chronic phase: Note: Continue dasatinib until disease progression or unacceptable toxicity. Recalculate the dose every 3 months or as clinically necessary based on changes in body weight.
Children weighing ≥10 kg and Adolescents: Oral:
10 to <20 kg: Initial: 40 mg once daily; may escalate to 50 mg once daily if hematologic or cytogenetic response is not achieved
20 to <30 kg: Initial: 60 mg once daily; may escalate to 70 mg once daily if hematologic or cytogenetic response is not achieved
30 to <45 kg: Initial: 70 mg once daily; may escalate to 90 mg once daily if hematologic or cytogenetic response is not achieved
≥45 kg: Initial: 100 mg once daily; may escalate to 120 mg once daily if hematologic or cytogenetic response is not achieved
Dosage adjustment for concomitant strong CYP3A4 inhibitors: Avoid concomitant administration with strong CYP3A4 inhibitors and grapefruit juice; if concomitant administration with a strong CYP3A4 inhibitor cannot be avoided, consider dasatinib dose reductions and careful monitoring (see following table); dosing adjustment based on pharmacokinetic data; specific clinical data area lacking; monitor patients closely. If reduced dasatinib dose is not tolerated, either discontinue the strong CYP3A4 inhibitor or interrupt dasatinib therapy temporarily until the concomitant inhibitor use is discontinued. When a strong CYP3A4 inhibitor is discontinued, allow a washout period of ~1 week prior to adjusting dasatinib dose upward.
|
Current dasatinib daily dose |
Recommended dosing adjustment |
|---|---|
|
40 mg or 60 mg |
Consider withholding therapy until strong CYP3A4 inhibitor discontinued; allow ~1 week washout period before restarting dasatinib. |
|
70 mg or 100 mg |
Decrease dose to 20 mg once daily |
|
140 mg |
Decrease dose to 40 mg once daily |
Table converted to following text:
If current dasatinib dose is 40 mg or 60 mg once daily, consider withholding dasatinib until the strong CYP3A4 inhibitor is discontinued; allow a washout period of ~1 week prior to reinitiating dasatinib.
If current dasatinib dose is 70 mg or 100 mg once daily, decrease dose to 20 mg once daily.
If current dasatinib dose if 140 mg once daily, decrease dose to 40 mg once daily.
Dosage adjustment for concomitant strong CYP3A4 inducers: Avoid concomitant administration with strong CYP3A4 inducers and St John's wort; if concomitant administration with a strong CYP3A4 inducer cannot be avoided, consider increasing the dasatinib dose with careful monitoring.
Dosing adjustment for toxicity:
Hematologic toxicity: Children and Adolescents: Adjustments are specific for indications. Note: Growth factor support may be considered in patients with resistant myelosuppression.
Acute lymphoblastic leukemia, Philadelphia chromosome-positive (Ph+ ALL): If neutropenia and/or thrombocytopenia result in a delay of the next block of treatment by >14 days, interrupt dasatinib treatment and resume at the same level once the next block of treatment is started. If neutropenia and/or thrombocytopenia persist and the next block of treatment is delayed another 7 days, perform a bone marrow assessment to assess cellularity and blast percentage. If marrow cellularity is <10%, interrupt dasatinib treatment until ANC >500/mm3 and then resume dasatinib at the full dose. If marrow cellularity is >10%, consider resuming dasatinib.
Chronic myelogenous leukemia, Philadelphia chromosome-positive (Ph+ CML):
If cytopenia (eg, neutropenia, thrombocytopenia) persists for >3 weeks, determine if cytopenia is due to leukemia by performing a marrow aspirate or biopsy.
If cytopenia is unrelated to leukemia, withhold dasatinib until ANC ≥1,000/mm3 and platelets ≥75,000/mm3 and resume dasatinib at the original starting dose or at a reduced dose.
If cytopenia recurs, repeat marrow aspirate/biopsy and resume dasatinib at a reduced dose.
Note: If ≥ grade 3 neutropenia or thrombocytopenia recurs during complete hematologic response, interrupt dasatinib therapy and resume at a reduced dose. Temporary dose reductions for intermediate degrees of cytopenia and disease response may be used as needed.
Recommended dose reductions for neutropenia and thrombocytopenia in Ph+ CML:
If the original starting dose is 40 mg daily, may reduce dose to 20 mg once daily (one-level dose reduction); further dose reductions cannot be made due to available tablet sizes
If the original starting dose is 60 mg once daily, may reduce dose to 40 mg once daily (one-level dose reduction), and then to 20 mg once daily (two-level dose reduction)
If the original starting dose is 70 mg once daily, may reduce dose to 60 mg once daily (one-level dose reduction), and then to 50 mg once daily (two-level dose reduction)
If the original starting dose is 100 mg once daily, may reduce dose to 80 mg once daily (one-level dose reduction), and then to 70 mg once daily (two-level dose reduction)
Nonhematologic toxicity: Recommendations exclude altered liver enzymes (see Dosing: Hepatic Impairment: Pediatric)
Ph+ ALL:
Grade 2 toxicity: If no recovery despite symptomatic management, consider interrupting dasatinib therapy; once recovered to ≤ grade 1, resume at the original starting dose. For recurrent events, resume dasatinib at a reduced dose (see the following dose reductions).
Grade ≥3 toxicity: Withhold dasatinib until recovered to grade 1 or lower, and then resume at a reduced dose (see the following dose reductions).
Recommended dose reductions for non-hematologic toxicities Ph+ ALL:
If the original starting dose is 40 mg daily, may reduce dose to 20 mg once daily (one-level dose reduction); further dose reductions cannot be made due to available tablet sizes.
If the original starting dose is 60 mg once daily, may reduce dose to 40 mg once daily (one-level dose reduction), and then to 20 mg once daily (two-level dose reduction).
If the original starting dose is 70 mg once daily, may reduce dose to 60 mg once daily (one-level dose reduction), and then to 50 mg once daily (two-level dose reduction).
If the original starting dose is 100 mg once daily, may reduce dose to 80 mg once daily (one-level dose reduction), and then to 70 mg once daily (two-level dose reduction).
Ph+ CML: Severe nonhematologic toxicity: Withhold treatment until toxicity improvement or resolution; if appropriate, resume treatment at a reduced dose based on the event severity and recurrence.
All indications:Management of other nonhematologic toxicities:
Dermatologic toxicities: Manage rash with antihistamines or topical or systemic steroids (Khoury 2009), or treatment interruption, dose reduction, or discontinuation. Discontinue if dasatinib-related severe mucocutaneous reaction occurs.
Fluid retention: Manage with diuretics, short courses of corticosteroids, and/or supportive care. Severe pleural effusions may require thoracentesis and oxygen therapy; consider dose reduction or treatment interruption.
Pleural effusion: For first episode of grade 3 pleural effusion, withhold treatment until resolves to grade 1 or lower and consider corticosteroids (eg, prednisone for 3 to 4 days), diuretics, thoracentesis, and/or pleurodesis; may resume dasatinib at a decreased dose (one-level dose reduction) when effusion resolves; if pleural effusion recurs, initiate supportive therapy, withhold therapy, and resume at next lower dose level (two-level dose reduction) or discontinue therapy (Khoury 2009).
Pulmonary arterial hypertension: Discontinue with confirmed pulmonary arterial hypertension.
Dosing: Adjustment for Toxicity
Hematologic toxicity: Note: Growth factor support may be considered in patients with resistant myelosuppression.
Chronic phase CML (100 mg daily starting dose): For ANC <500/mm3 or platelets <50,000/mm3, withhold treatment until ANC ≥1000/mm3 and platelets ≥50,000/mm3; then resume treatment at the original starting dose if recovery occurs in ≤7 days. If platelets <25,000/mm3 or recurrence of ANC <500/mm3 for >7 days, withhold treatment until ANC ≥1000/mm3 and platelets ≥50,000/mm3; then resume treatment at 80 mg once daily (second episode). For third episode, further reduce dose to 50 mg once daily (for newly diagnosed patients) or discontinue (for patients resistant or intolerant to prior therapy)
Accelerated or blast phase CML and Ph+ ALL (140 mg once daily starting dose): For ANC <500/mm3 or platelets <10,000/mm3, if cytopenia unrelated to leukemia, withhold treatment until ANC ≥1,000/mm3 and platelets ≥20,000/mm3; then resume treatment at the original starting dose. If cytopenia recurs, withhold treatment until ANC ≥1,000/mm3 and platelets ≥20,000/mm3; then resume treatment at 100 mg once daily (second episode) or 80 mg once daily (third episode). For cytopenias related to leukemia (confirm with marrow aspirate or biopsy), consider dose escalation to 180 mg once daily.
Nonhematologic toxicity:
Adults with Ph+ CML and ALL: Severe nonhematologic toxicity: Withhold treatment until toxicity improvement or resolution; if appropriate, resume treatment at a reduced dose based on the event severity and recurrence.
Management of other nonhematologic toxicities:
Dermatologic toxicities: Manage rash with antihistamines or topical or systemic steroids (Khoury 2009), or treatment interruption, dose reduction, or discontinuation. Discontinue if dasatinib-related severe mucocutaneous reaction occurs.
Fluid retention: Manage with diuretics, short courses of corticosteroids, and/or supportive care. Severe pleural effusions may require thoracentesis and oxygen therapy; consider dose reduction or treatment interruption. For grade 3 pleural effusion, withhold treatment until resolves to grade 1 or lower and consider corticosteroids (eg, prednisone 20 to 40 mg/day for 3 to 4 days), diuretics, thoracentesis and/or pleurodesis; may resume dasatinib at a decreased dose when effusion resolves (Khoury 2009).
Pulmonary arterial hypertension: Discontinue with confirmed pulmonary arterial hypertension.
Extemporaneously Prepared
An oral suspension may be prepared by dissolving dasatinib tablet(s) for one dose in 30 mL chilled orange or apple juice (without preservatives). After 5 minutes, swirl the contents for 3 seconds and repeat the process every 5 minutes for a total of 20 minutes following addition of tablet(s). Minimize time between end of 20 minutes and administration since suspension will taste more bitter if allowed to stand longer. Swirl contents of container one last time, then administer immediately. To ensure the full dose is administered, rinse container with 15 mL juice and administer residue. May be administered orally (or by nasogastric tube). Discard any unused portion after 60 minutes.
Sprycel data on file, Bristol-Myers Squibb
Administration
Oral: Administer once daily (morning or evening). May be taken without regard to food. Swallow whole; do not break, cut, crush, or chew tablets. Take with a meal if GI upset occurs (Khoury 2009). Do not administer proton pump inhibitors and H2 blockers concomitantly with dasatinib. If needed, may consider antacid administration, separated by at least 2 hours before or 2 hours after the dasatinib dose.
Dietary Considerations
Avoid grapefruit juice.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
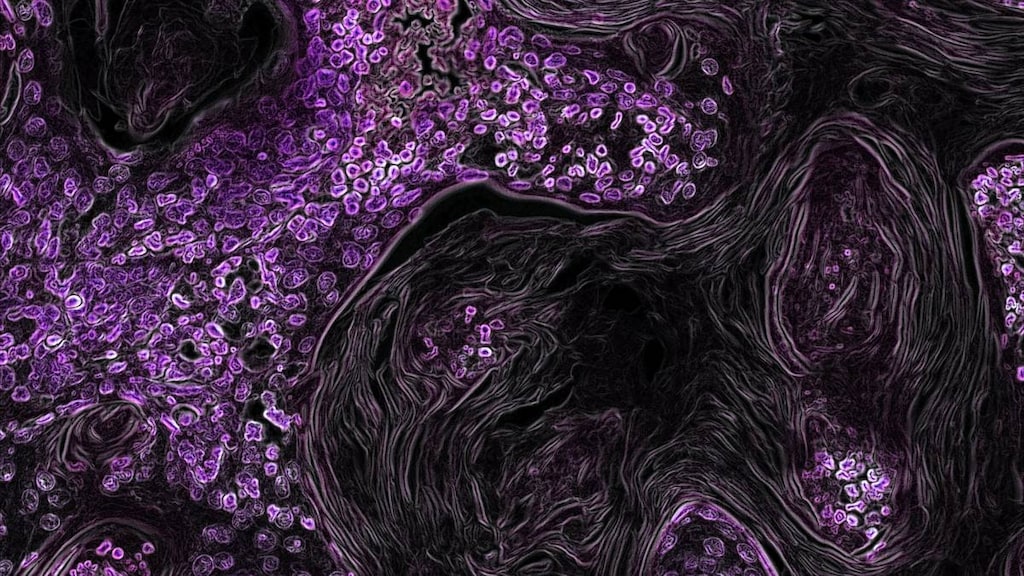
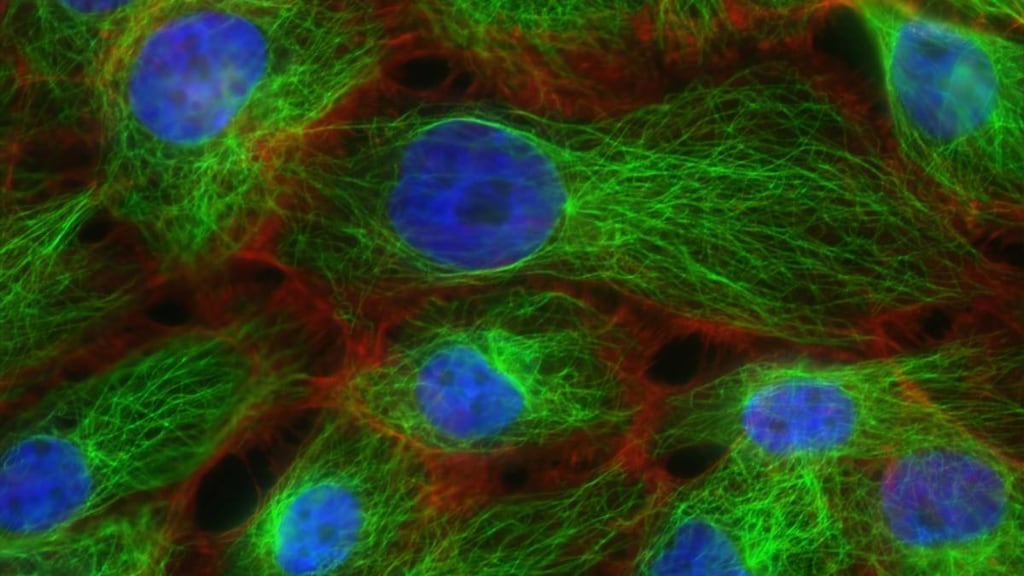
Dasatinib Images
Drug Interactions
Acetaminophen: May enhance the hepatotoxic effect of Dasatinib. Dasatinib may increase the serum concentration of Acetaminophen. Consider therapy modification
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): Dasatinib may enhance the anticoagulant effect of Agents with Antiplatelet Properties. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Citalopram; Escitalopram. Monitor therapy
Antacids: May decrease the serum concentration of Dasatinib. Management: Simultaneous administration of dasatinib and antacids should be avoided. Administer antacids 2 hours before or 2 hours after dasatinib. Consider therapy modification
Anticoagulants: Dasatinib may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitor clinical response and toxicity closely. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Dasatinib. Management: This combination should be avoided if possible. If combined, dasatinib dose reductions are recommended. See full monograph for details. Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Ceritinib; Clarithromycin; Saquinavir; Voriconazole. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
DexAMETHasone (Systemic): May decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitoring clinical response and toxicity closely. Consider therapy modification
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of Dasatinib. Avoid combination
Haloperidol: QT-prolonging Kinase Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Histamine H2 Receptor Antagonists: May decrease the absorption of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of H2-antagonists if some acid-reducing therapy is needed. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lefamulin: May enhance the QTc-prolonging effect of QT-prolonging CYP3A4 Substrates. Management: Do not use lefamulin tablets with QT-prolonging CYP3A4 substrates. Lefamulin prescribing information lists this combination as contraindicated. Avoid combination
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Posaconazole: May increase the serum concentration of QT-prolonging CYP3A4 Substrates. Such increases may lead to a greater risk for proarrhythmic effects and other similar toxicities. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Propacetamol: Dasatinib may enhance the hepatotoxic effect of Propacetamol. Dasatinib may increase serum concentrations of the active metabolite(s) of Propacetamol. Specifically, acetaminophen concentrations may increase. Consider therapy modification
Proton Pump Inhibitors: May decrease the serum concentration of Dasatinib. Management: Antacids (taken 2 hours before or after dasatinib administration) can be used in place of the proton pump inhibitor if some acid-reducing therapy is needed. Avoid combination
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of other QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): QT-prolonging Kinase Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Kinase Inhibitors (Moderate Risk). Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): Dasatinib may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Dasatinib. Management: Avoid concomitant use of dasatinib and strong CYP3A4 inhibitors that prolong the QTc interval whenever possible. If combined, dasatinib dose reductions are required. Monitor patients for dasatinib toxicities including QTc prolongation and arrhythmias. Exceptions: Saquinavir. Consider therapy modification
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Saquinavir: Dasatinib may enhance the QTc-prolonging effect of Saquinavir. Saquinavir may increase the serum concentration of Dasatinib. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
St John's Wort: May decrease the serum concentration of Dasatinib. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Adverse Reactions
Adverse reactions occurred in adults unless otherwise indicated.
≥10%:
Cardiovascular: Facial edema, peripheral edema
Central nervous system: Headache (adults and children: 12% to 33%), fatigue (adults: 8% to 26%; children: 10%), pain (11%)
Dermatologic: Skin rash (adults and children: 11% to 21%), pruritus (12%)
Endocrine & metabolic: Fluid retention (adults: 19% to 48%; children: 10%; cardiac-related: 9%)
Gastrointestinal: Diarrhea (adults: 17% to 31%; children: 21%), nausea (adults and children: 8% to 24%), vomiting (adults and children: 5% to 16%), abdominal pain (adults and children: 7% to 16%)
Hematologic & oncologic: Thrombocytopenia (grades 3/4: 22% to 85%), neutropenia (grades 3/4: 29% to 79%), anemia (grades 3/4: 13% to 74%), hemorrhage (8% to 26%; grades 3/4: 1% to 9%), febrile neutropenia (4% to 12%; grades 3/4: 4% to 12%)
Infection: Infection (9% to 14%)
Local: Localized edema (3% to 22%; superficial)
Neuromuscular & skeletal: Musculoskeletal pain (<22%), limb pain (children: 19%), myalgia (7% to 13%), arthralgia (adults and children: ≤13%)
Respiratory: Pleural effusion (5% to 28%), dyspnea (3% to 24%)
Miscellaneous: Fever (6% to 18%)
1% to <10%:
Cardiovascular: Cardiac conduction disturbance (7%), ischemic heart disease (4%), cardiac disorder (≤4%), edema (≤4%), pericardial effusion (≤4%), prolonged Q-T interval on ECG (≤1%), cardiac arrhythmia, chest pain, flushing, hypertension, palpitations, tachycardia
Central nervous system: Intracranial hemorrhage (≤3%), chills, depression, dizziness, drowsiness, insomnia, myasthenia, neuropathy, peripheral neuropathy
Dermatologic: Acne vulgaris, alopecia, dermatitis, eczema, hyperhidrosis, urticaria, xeroderma
Endocrine & metabolic: Growth suppression, hyperuricemia, weight gain, weight loss
Gastrointestinal: Constipation (10%), gastrointestinal hemorrhage (2% to 9%), abdominal distention, change in appetite, colitis (including neutropenic colitis), dysgeusia, dyspepsia, enterocolitis, gastritis, mucositis, stomatitis
Hematologic & oncologic: Bruise
Hepatic: Increased serum bilirubin (grades 3/4: ≤6%), increased serum alanine aminotransferase (grades 3/4: ≤5%), increased serum aspartate aminotransferase (grades 3/4: ≤4%), ascites (≤1%)
Infection: Herpes virus infection, sepsis
Neuromuscular & skeletal: Muscle spasm (5%), abnormal bone growth (children; epiphyses delayed fusion), asthenia, stiffness
Ophthalmic: Blurred vision, decreased visual acuity, dry eye syndrome, visual disturbance
Otic: Tinnitus
Renal: Increased serum creatinine (grades 3/4: ≤8%)
Respiratory: Pulmonary hypertension (≤5%), pulmonary edema (≤4%), cough, pneumonia, pneumonitis, pulmonary infiltrates, upper respiratory tract infection
Miscellaneous: Soft tissue injury (oral)
<1%, postmarketing, and/or case reports: Abnormal gait, abnormal platelet aggregation, abnormal T waves on ECG, acute coronary syndrome, acute pancreatitis, acute respiratory distress, amnesia, anal fissure, angina pectoris, anxiety, arthritis, asthma, ataxia, atrial fibrillation, atrial flutter, bronchospasm, bullous skin disease, cardiomegaly, cerebrovascular accident, cholecystitis, cholestasis, confusion, conjunctivitis, coronary artery disease, cor pulmonale, cranial nerve palsy (facial), decreased libido, deep vein thrombosis, dehydration, dementia, dermal ulcer, diabetes mellitus, dyschromia, dysphagia, embolism, emotional lability, epistaxis, equilibrium disturbance, erythema nodosum, esophagitis, fibrosis (dermal), fistula (anal), gastroesophageal reflux disease, gastrointestinal disease (protein wasting), gingival hemorrhage, gynecomastia (adults and children), hearing loss, hematoma, hematuria, hemoptysis, hemorrhage (ocular), hepatitis, hypercholesterolemia, hypersensitivity reaction, hypersensitivity angiitis, hyperthyroidism, hypoalbuminemia, hypotension, hypothyroidism, increased creatine phosphokinase, increased gamma-glutamyl transferase, increased lacrimation, increased pulmonary artery pressure, increased troponin, inflammation (panniculitis), interstitial pulmonary disease, intestinal obstruction, livedo reticularis, lymphadenopathy, lymphocytopenia, malaise, menstrual disease, myocarditis, nail disease, nephrotic syndrome, optic neuritis, osteonecrosis, osteopenia (children), ototoxicity (hemorrhage), palmar-plantar erythrodysesthesia, pancreatitis, pericarditis, petechia, photophobia, pleuropericarditis, prolongation P-R interval on ECG, proteinuria, pulmonary embolism, pure red cell aplasia, reactivation of HBV, renal failure syndrome, renal insufficiency, rhabdomyolysis, seizure, skin photosensitivity, Stevens-Johnson syndrome, Sweet's syndrome, syncope, tendonitis, thrombophlebitis, thrombosis, thrombotic microangiopathy, thyroiditis, transient ischemic attacks, tremor, tumor lysis syndrome, upper gastrointestinal tract ulcer, urinary frequency, uterine hemorrhage, vaginal hemorrhage, ventricular arrhythmia, ventricular tachycardia, vertigo, voice disorder
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Severe dose-related bone marrow suppression (thrombocytopenia, neutropenia, anemia) is associated with dasatinib treatment. Hematologic toxicity is usually reversible with dosage adjustment and/or temporary treatment interruption. The incidence of myelosuppression is higher in patients with advanced chronic myeloid leukemia (CML) and Ph+ acute lymphoblastic leukemia (ALL). Monitor blood counts every 2 weeks for 12 weeks and then every 3 months thereafter or as clinically indicated (for chronic phase CML) or weekly for the first 2 months, then monthly thereafter or as clinically necessary (for accelerated or blast phase CML or for ALL). In pediatric patients with Ph+ ALL, monitor blood counts prior to initiation of each block of chemotherapy and then as clinically indicated; monitor blood counts every 2 days until recovery during the consolidation blocks of chemotherapy.
- Cardiovascular adverse events: Dasatinib may cause cardiac dysfunction; cardiac ischemic events, cardiac fluid retention-related events, and conduction abnormalities (arrhythmia and palpitations) have been reported. Monitor for signs and symptoms of cardiac dysfunction. Monitor blood pressure routinely during dasatinib treatment; if indicated, initiate appropriate antihypertensive treatment to reduce the risk for cardiotoxicity (Armenian 2017).
- Dermatologic toxicity: Cases of severe mucocutaneous dermatologic reactions (including Stevens-Johnson syndrome and erythema multiforme) have been reported with dasatinib. Discontinue dasatinib if severe mucocutaneous reaction occurs and other etiologies have been ruled out.
- Fluid retention: Dasatinib may cause fluid retention, including pleural and pericardial effusions, pulmonary hypertension, and generalized or superficial edema. A prompt chest x-ray (or other appropriate diagnostic imaging) is recommended for symptoms suggestive of effusion (new or worsening dyspnea on exertion or at rest, pleuritic chest pain, or dry cough). Fluid retention may be managed with supportive care (diuretics or corticosteroids); thoracentesis and oxygen therapy may be necessary for severe fluid retention; consider dose reduction or treatment interruption. Utilizing once-daily dosing is associated with a decreased frequency of fluid retention. The risk for pleural effusion is increased in patients with hypertension, prior cardiac history and a twice a day administration schedule; interrupt treatment for grade ≥2 effusion; may consider reinitiating at a reduced dose after resolution (Quintás-Cardama 2007). Grade 3 or 4 fluid retention/pleural effusion was observed in adults and grade 1 or 2 fluid retention was observed in pediatric patients. Use with caution in patients where fluid accumulation may be poorly tolerated, such as in cardiovascular disease (HF or hypertension) and pulmonary disease.
- Hemorrhage: Dasatinib may cause serious and fatal bleeding, including grades 3 and higher CNS hemorrhage. The most frequent hemorrhage site was gastrointestinal. Grades 3 or 4 hemorrhage usually required treatment interruptions and transfusions. Most bleeding events in clinical studies were associated with severe thrombocytopenia, although dasatinib may also cause platelet dysfunction. Concomitant medications that inhibit platelet function or anticoagulants may increase the risk of bleeding.
- Pulmonary arterial hypertension: Dasatinib may increase the risk for pulmonary arterial hypertension (PAH) in both adult and pediatric patients. PAH may occur at any time after starting treatment, including after >12 months of therapy. Evaluate for underlying cardiopulmonary disease prior to therapy initiation and during therapy; evaluate and rule out alternative etiologies in patients with symptoms suggestive of PAH (eg, dyspnea, fatigue, hypoxia, fluid retention) and interrupt therapy if symptoms are severe. Discontinue permanently with confirmed PAH diagnosis (may be reversible upon discontinuation).
- QT prolongation: Dasatinib may increase the risk for QT interval prolongation; there are reports of patients with QTcF >500 msec. Use caution in patients at risk for QT prolongation, including patients with long QT syndrome, patients taking antiarrhythmic medications or other medications that lead to QT prolongation or potassium-wasting diuretics, patients with cumulative high-dose anthracycline therapy, and conditions which cause hypokalemia or hypomagnesemia. Correct hypokalemia and hypomagnesemia prior to and during dasatinib therapy.
- Tumor lysis syndrome: Tumor lysis syndrome (TLS) has been reported in patients with resistance to imatinib therapy, usually in patients with advanced phase disease. Risk for TLS is higher in patients with advanced stage disease and/or a high tumor burden; monitor patients at risk more frequently. Maintain adequate hydration and correct uric acid levels prior to treatment; monitor electrolyte levels.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment due to extensive hepatic metabolism.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information. Use with caution in patients taking anticoagulants or medications interfering with platelet function; not studied in clinical trials. Avoid concomitant use with CYP3A4 inducers and inhibitors; if concomitant use cannot be avoided, consider dasatinib dosage adjustments.
- Drugs that affect gastric pH: Elevated gastric pH may reduce dasatinib bioavailability; do not administer proton pump inhibitors and H2 blockers concomitantly with dasatinib. If needed, may consider antacid administration separated by at least 2 hours before or 2 hours after the dasatinib dose.
Special populations:
- Elderly: Patients 65 years of age and older are more likely to experience toxicity (compared with younger patients).
- Pediatric: Adverse reactions associated with bone growth and development have been reported in pediatric studies of chronic phase CML (including a report of severe [grade 3] growth retardation). Cases have included epiphyses delayed fusion, osteopenia, growth retardation, and gynecomastia; some cases resolved during treatment. Monitor bone growth/development in pediatric patients.
Monitoring Parameters
CBC with differential every 2 weeks for 12 weeks and then every 3 months thereafter or as clinically indicated (for chronic phase chronic myeloid leukemia [CML]) or weekly for 2 months, then monthly or as clinically necessary (for accelerated or blast phase CML or for acute lymphoblastic leukemia [ALL]); CBC with differential prior to initiation of each block of chemotherapy and then as clinically indicated and every 2 days until recovery during consolidation blocks of chemotherapy (pediatric patients with Ph+ ALL); bone marrow biopsy; liver function tests, electrolytes including calcium, phosphorus, magnesium; monitor for fluid retention; monitor for signs/symptoms of cardiac dysfunction; ECG monitoring if at risk for QTc prolongation; chest x-ray is recommended for symptoms suggestive of pleural effusion (eg, cough, dyspnea); signs/symptoms of tumor lysis syndrome and dermatologic reactions. Monitor bone growth/development in pediatric patients. Monitor blood pressure routinely (Armenian 2017). Monitor adherence.
Thyroid function testing recommendations (Hamnvik 2011):
Preexisting levothyroxine therapy: Obtain baseline TSH levels, then monitor every 4 weeks until levels and levothyroxine dose are stable, then monitor every 2 months
Without preexisting thyroid hormone replacement: TSH at baseline, then monthly for 4 months, then every 2 to 3 months
Pregnancy
Pregnancy Considerations
Dasatinib crosses the placenta, with fetal plasma and amniotic concentrations comparable to maternal concentrations. Adverse effects, including hydrops fetalis and fetal leukopenia and thrombocytopenia have been reported following maternal exposure to dasatinib. Females of reproductive potential should use effective contraception during treatment and for 30 days after the final dasatinib dose. Pregnant females are advised to avoid exposure to crushed or broken tablets.
Patient Education
What is this drug used for?
- It is used to treat a type of leukemia.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Lack of appetite
- Muscle pain
- Joint pain
- Constipation
- Painful extremities
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Low phosphate like vision changes, confusion, mood changes, muscle pain, muscle weakness, difficulty breathing, or difficulty swallowing.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Shortness of breath
- Edema
- Weight gain
- Swelling of arms or legs
- Difficulty breathing
- Chest pain
- Fast heartbeat
- Passing out
- Abnormal heartbeat
- Severe dizziness
- Severe abdominal pain
- Severe nausea
- Vomiting
- Severe diarrhea
- Severe loss of strength and energy
- Numbness or tingling of hands or feet
- Seizure
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; unable to pass urine; muscle weakness or cramps; nausea, vomiting, diarrhea or lack of appetite; or feeling sluggish.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.