Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as hydrochloride:
Generic: 150 mg, 300 mg
Pharmacology
Mechanism of Action
Inhibits protein synthesis by binding with the 30S and possibly the 50S ribosomal subunit(s) of susceptible bacteria; may also cause alterations in the cytoplasmic membrane; inhibits the action of ADH in patients with chronic SIADH
Pharmacokinetics/Pharmacodynamics
Absorption
66% (Agwuh 2006); extent of absorption is reduced by food and by certain antacids and dairy products containing aluminum, calcium, magnesium, or iron
Distribution
1.7 L/kg (Agwuh 2006)
Metabolism
None
Excretion
Urine (44% as unchanged drug); feces (13% to 46% as unchanged drug)
Onset of Action
SIADH: 2 to 5 days (Sherlock 2010)
Time to Peak
Serum: ~4 hours
Half-Life Elimination
10 to 16 hours
Protein Binding
~40% to 90%
Use: Labeled Indications
Note: Use of demeclocycline as an antibacterial agent is uncommon; alternative tetracycline agents (eg, doxycycline, minocycline, tetracycline) are generally preferred.
Acne: Adjunctive therapy in severe acne.
Actinomycosis: Treatment of actinomycosis caused by Actinomyces israelii when penicillin is contraindicated.
Acute intestinal amebiasis: Adjunct to amebicides in acute intestinal amebiasis.
Anthrax: Treatment of anthrax due to Bacillus anthracis when penicillin is contraindicated.
Cholera: Treatment of cholera caused by Vibrio cholerae.
Clostridium: Treatment of clostridial disease caused by Clostridium spp. when penicillin is contraindicated.
Gram-negative infections: Treatment of infections caused by Escherichia coli, Enterobacter aerogenes, Shigella species, and Acinetobacter species.
Listeriosis: Treatment of listeriosis due to Listeria monocytogenes when penicillin is contraindicated.
Ophthalmic infections: Treatment of inclusion conjunctivitis or trachoma caused by Chlamydia trachomatis.
Plague: Treatment of plague due to Yersinia pestis.
Relapsing fever: Treatment of relapsing fever caused by Borrelia recurrentis.
Respiratory tract infections: Treatment of respiratory tract infections caused by Haemophilus influenzae, Klebsiella species, or Mycoplasma pneumoniae; treatment of upper respiratory tract infections caused by Streptococcus pneumoniae.
Rickettsial infections: Treatment of Rocky Mountain spotted fever, typhus fever, and the typhus group, Q fever, rickettsialpox and tick fevers caused by Rickettsiae.
Sexually transmitted diseases:
Treatment of lymphogranuloma venereum caused by Chlamydia trachomatis; granuloma inguinale caused by Klebsiella granulomatis; chancroid caused by Haemophilus ducreyi; nongonococcal urethritis caused by Ureaplasma urealyticum or Chlamydia trachomatis; when penicillin is contraindicated, uncomplicated urethritis in men caused by Neisseria gonorrhea and other uncomplicated gonococcal infections, infections in women caused by N. gonorrhea, and syphilis caused by Treponema pallidum subspecies pallidum.
Demeclocycline is not a recommended alternative for gonorrhea according to the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases guidelines. Consult current guidelines for recommendations (Workowski 2015).
Skin and skin structure infections: Treatment of skin and skin structure infections caused by Staphylococcus aureus.
Urinary tract infections: Treatment of urinary tract infections caused by Klebsiella species
Vincent infection: Treatment of Vincent infection caused by Fusobacterium fusiforme when penicillin is contraindicated.
Yaws: Treatment of yaws caused by Treponema pallidum subspecies pertenue when penicillin is contraindicated.
Zoonotic infections: Treatment of psittacosis (ornithosis) caused by Chlamydophila psittaci; tularemia caused by Francisella tularensis; brucellosis caused by Brucella species (in conjunction with streptomycin); bartonellosis caused by Bartonella bacilliformis; infections caused by Campylobacter fetus.
Use: Off Label
Chronic syndrome of inappropriate secretion of antidiuretic hormone (SIADH)cyes
Data from a limited number of patients (case reports) with symptomatic chronic SIADH suggest that demeclocycline may be beneficial for the treatment of this condition Cherrill 1975, De Troyer 1975. Clinical experience also suggests the utility of demeclocycline in managing chronic SIADH Goh 2004, Gross 2008, Pasquale 2005, Sherlock 2010. Additional data may be necessary to further define the role of demeclocycline in this condition.
Conflicting recommendations exist in guidelines on the use of demeclocycline for SIADH. European clinical practice guidelines recommend against the use of demeclocycline in the treatment of moderate or profound hyponatremia (serum sodium 125 to 129 mmol/L or <125 mmol/L, respectively) in patients with SIADH, and further advise against the use of demeclocycline for the management of any degree of chronic hyponatremia in patients with SIADH due to some evidence of potential harm Spasovski 2014. Conversely, recommendations from an Expert Panel on the Diagnosis, Evaluation, and Treatment of Hyponatremia suggest that demeclocycline may be used as a second-line pharmacologic treatment option in non-acute or asymptomatic hyponatremia in patients with SIADH where first line therapy of fluid restriction is ineffective, impractical, or unpalatable Verbalis 2013.
Contraindications
Hypersensitivity to demeclocycline, tetracyclines, or any component of the formulation
Dosage and Administration
Dosing: Adult
Susceptible infections: Oral: 150 mg 4 times daily or 300 mg twice daily
SIADH (off-label use): Oral: 600 to 1,200 mg/day (Goh 2004; Gross 2008, Verbalis 2013). Note: Limited high quality evidence exists to define the clinical role, if any, of demeclocycline in this condition. European clinical practice guidelines recommend against the use of demeclocycline for the management of hyponatremia in patients with SIADH (Spasovski 2014).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Susceptible infections: Note: Although FDA approved, use of demeclocycline as an antibacterial agent is uncommon and rarely used; alternative tetracyclines are recommended (eg, doxycycline, minocycline, tetracycline).
Children ≥8 years and Adolescents: Oral: 7 to 13 mg/kg/day divided every 6 to 12 hours; maximum daily dose: 600 mg/day
Administration
Administer 1 hour before or 2 hours after food or milk. Administer with adequate amounts of fluid to decrease the risk of esophageal irritation and ulceration.
Dietary Considerations
Due to potential for decreased absorption, administer 1 hour before or 2 hours after food or milk.
Storage
Store at 20°C to 25°C (68°F to 77°F).
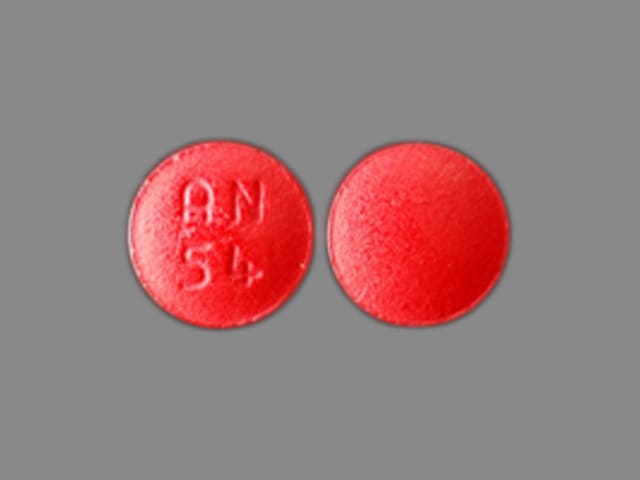
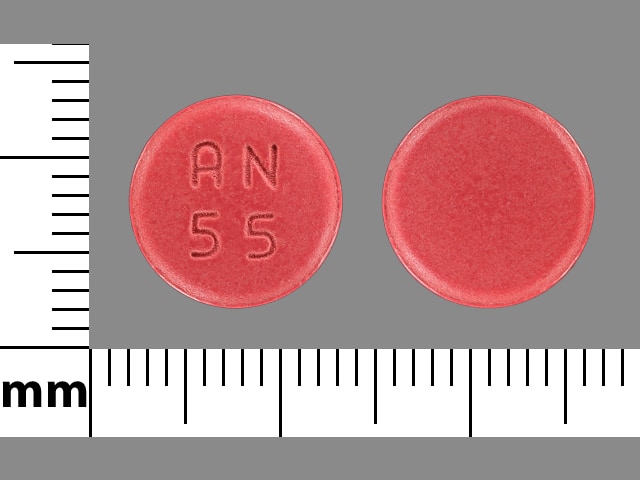
Demeclocycline Images
Drug Interactions
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Antacids: May decrease the absorption of Tetracyclines. Management: Separate administration of antacids and oral tetracycline derivatives by several hours when possible to minimize the extent of this potential interaction. Consider therapy modification
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Tetracyclines. Consider therapy modification
Bismuth Subcitrate: May decrease the serum concentration of Tetracyclines. Management: Avoid administration of oral tetracyclines within 30 minutes of bismuth subcitrate administration. This is of questionable significance for at least some regimens intended to treat H. pylori infections. Consider therapy modification
Bismuth Subsalicylate: May decrease the serum concentration of Tetracyclines. Management: Consider dosing tetracyclines 2 hours before or 6 hours after bismuth. The need to separate doses during Helicobacter pylori eradication regimens is questionable. Consider therapy modification
Calcium Salts: May decrease the serum concentration of Tetracyclines. Management: If coadministration of oral calcium with oral tetracyclines can not be avoided, consider separating administration of each agent by several hours. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Desmopressin: Demeclocycline may diminish the therapeutic effect of Desmopressin. Monitor therapy
Iron Preparations: Tetracyclines may decrease the absorption of Iron Preparations. Iron Preparations may decrease the serum concentration of Tetracyclines. Management: Avoid this combination if possible. Administer oral iron preparations at least 2 hours before, or 4 hours after, the dose of the oral tetracycline derivative. Monitor for decreased therapeutic effect of oral tetracycline derivatives. Exceptions: Ferric Carboxymaltose; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lanthanum: May decrease the serum concentration of Tetracyclines. Management: Administer oral tetracycline antibiotics at least two hours before or after lanthanum. Consider therapy modification
Magnesium Dimecrotate: May interact via an unknown mechanism with Tetracyclines. Monitor therapy
Magnesium Salts: May decrease the absorption of Tetracyclines. Only applicable to oral preparations of each agent. Consider therapy modification
Mecamylamine: Tetracyclines may enhance the neuromuscular-blocking effect of Mecamylamine. Avoid combination
Methoxyflurane: Tetracyclines may enhance the nephrotoxic effect of Methoxyflurane. Avoid combination
Mipomersen: Tetracyclines may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Tetracyclines. Management: If coadministration of a polyvalent cation-containing multivitamin with oral tetracyclines can not be avoided, separate administration of each agent by several hours. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Tetracyclines. Management: If coadministration of a polyvalent cation-containing multivitamin with oral tetracyclines can not be avoided, separate administration of each agent by several hours. Consider therapy modification
Neuromuscular-Blocking Agents: Tetracyclines may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Monitor therapy
Penicillins: Tetracyclines may diminish the therapeutic effect of Penicillins. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Quinapril: May decrease the serum concentration of Tetracyclines. Management: Separate doses of quinapril and oral tetracycline derivatives by at least 2 hours in order to reduce the risk of interaction. Monitor for reduced efficacy of the tetracycline if these products are used concomitantly. Consider therapy modification
Retinoic Acid Derivatives: Tetracyclines may enhance the adverse/toxic effect of Retinoic Acid Derivatives. The development of pseudotumor cerebri is of particular concern. Exceptions: Adapalene; Bexarotene (Topical); Tretinoin (Topical). Avoid combination
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Strontium Ranelate: May decrease the serum concentration of Tetracyclines. Management: In order to minimize any potential impact of strontium ranelate on tetracycline antibiotic concentrations, it is recommended that strontium ranelate treatment be interrupted during tetracycline therapy. Avoid combination
Sucralfate: May decrease the absorption of Tetracyclines. Management: Administer most tetracycline derivatives at least 2 hours prior to sucralfate in order to minimize the impact of this interaction. Administer oral omadacycline 4 hours prior to sucralfate. Consider therapy modification
Sucroferric Oxyhydroxide: May decrease the serum concentration of Tetracyclines. Management: Administer oral/enteral doxycycline at least 1 hour before sucroferric oxyhydroxide. Specific dose separation guidelines for other tetracyclines are not presently available. No interaction is anticipated with parenteral administration of tetracyclines. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Tetracyclines may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zinc Salts: May decrease the absorption of Tetracyclines. Only a concern when both products are administered orally. Management: Consider doxycycline as a noninteracting tetracycline derivative. Separate dose administration of oral tetracycline derivative and oral zinc salts by at least 2 hours to minimize interaction. Exceptions: Zinc Chloride. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Pericarditis
Central nervous system: Bulging fontanel (infants), dizziness, headache, pseudotumor cerebri (adults)
Dermatologic: Erythema multiforme, erythematous rash, maculopapular rash, skin photosensitivity, skin pigmentation, urticaria
Endocrine & metabolic: Microscopic thyroid discoloration (brown/black), nephrogenic diabetes insipidus
Gastrointestinal: Anorexia, dental discoloration (children <8 years, rare in adults), diarrhea, dysphagia, enterocolitis, esophageal ulcer, glossitis, nausea, pancreatitis, vomiting
Genitourinary: Balanitis, inflammatory anogenital lesion (with monilial overgrowth)
Hematologic & oncologic: Eosinophilia, hemolytic anemia, IgA vasculitis, neutropenia, thrombocytopenia
Hepatic: Increased liver enzymes
Hypersensitivity: Anaphylaxis, angioedema
Infection: Superinfection
Neuromuscular & skeletal: Exacerbation of systemic lupus erythematosus, Lambert-Eaton syndrome, lupus-like syndrome, polyarthralgia
Ophthalmic: Visual disturbance
Otic: Tinnitus
Renal: Acute renal failure, increased blood urea nitrogen
Respiratory: Pulmonary infiltrates
<1%, postmarketing, and/or case reports: Exfoliative dermatitis, fixed drug eruption, hepatic failure, hepatitis, hepatotoxicity, Stevens-Johnson syndrome, thyroid dysfunction
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May cause dizziness, blurred vision, or lightheadedness, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Diabetes insipidus syndrome: Dose-dependent nephrogenic diabetes insipidus is common with use (reversible on discontinuation); however, this adverse event of demeclocycline has been used as a therapeutic advantage in the off-label use of hyponatremia associated with SIADH.
- Increased BUN: May be associated with increases in BUN secondary to antianabolic effects; use caution in patients with renal impairment.
- Intracranial hypertension (eg, pseudotumor cerebri): Intracranial hypertension (headache, blurred vision) has been associated with use. Usually resolves after discontinuation of treatment; however, permanent sequelae are possible.
- Photosensitivity: May cause photosensitivity; discontinue if skin erythema occurs. Use skin protection and avoid prolonged exposure to sunlight; do not use tanning equipment.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment; dose adjustment and/or adjustment to interval frequency recommended. Hepatotoxicity and hepatic failure have been reported rarely with use.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment and/or adjustment to interval frequency recommended. Nephrotoxicity has also been reported with use, particularly in the setting of cirrhosis (Sherlock 2010).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: May cause tissue hyperpigmentation, enamel hypoplasia, or permanent tooth discoloration; use of tetracyclines should be avoided during tooth development (children <8 years of age) unless other drugs are not likely to be effective or are contraindicated.
- Pregnancy: Do not use during pregnancy. In addition to affecting tooth development, tetracycline use has been associated with retardation of skeletal development and reduced bone growth.
Monitoring Parameters
CBC, renal and hepatic function
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Demeclocycline crosses the placenta (Gibbons 1960). Tetracyclines accumulate in developing teeth and long tubular bones (Mylonas 2011). Permanent discoloration of teeth (yellow, gray, brown) can occur following in utero exposure and is more likely to occur following long-term or repeated exposure.
As a class, tetracyclines are generally considered second-line antibiotics in pregnant women and their use should be avoided (Mylonas 2011). Demeclocycline is not recommended for the treatment of Rocky Mountain Spotted Fever (Biggs 2016), Q fever (Anderson 2013), or anthrax infection (Meaney-Delman 2014) in pregnant women. When systemic antibiotics are needed for dermatologic conditions in pregnant women, other agents are preferred (Kong 2013; Murase 2014).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections. It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Dizziness
- Nausea
- Vomiting
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Chills
- Sore throat
- Bruising
- Bleeding
- Headache
- Blurred vision
- Double vision
- Vision loss
- Passing a lot of urine
- Increased thirst
- Weight loss
- Noise or ringing in the ears
- Severe loss of strength and energy
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.