Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and incomplete; reduced by food
Distribution
Vd: 5.99 L; increased in patients with ESRD on IHD (Nauta 1976); CSF penetration is low
Excretion
Feces; urine (as unchanged drug)
Neonates: Prolonged
CF patients: More rapid excretion than healthy patients (Jusko 1975)
Time to Peak
Serum: 1 to 1.5 hours
Half-Life Elimination
~0.7 hours; prolonged with renal impairment (Nauta 1976)
Protein Binding
95% to 99%
Use: Labeled Indications
Staphylococcal infections: Treatment of infections caused by penicillinase-producing staphylococci.
Use: Off Label
Bite wounds (animal)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), dicloxacillin, in combination with penicillin, is an effective and recommended option for treatment of animal bites.
Impetigoyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), dicloxacillin is an effective and recommended agent for treatment of impetigo IDSA [Stevens 2014.
Contraindications
Hypersensitivity to dicloxacillin, other penicillins, or any component of the formulation
Dosage and Administration
Dosing: Adult
Staphylococcal infections: Oral: 125 to 250 mg every 6 hours
Bite wounds (animal) (off-label use): Oral: 500 mg 4 times daily; in combination with penicillin (IDSA [Stevens 2014])
Impetigo (off-label use): Oral: 250 mg 4 times daily for 7 days, depending on response (IDSA [Stevens 2014])
Prosthetic joint infection: Chronic suppression therapy: Staphylococci (oxacillin-susceptible) (off-label dose): Oral: 500 mg every 6 to 8 hours (Osmon 2013)
Skin and soft tissue infection due to MSSA (off-label dose): Oral: 500 mg every 6 hours for 7 to 14 days (IDSA [Stevens 2014])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection (Bradley 2016; Red Book [AAP 2015]): Infants, Children, and Adolescents:
Mild to moderate infection: Oral: 12 to 25 mg/kg/day divided every 6 hours; maximum dose: 250 mg/dose
Severe infection (step-down therapy of bone and joint infection): Oral: 100 mg/kg/day divided every 6 hours; maximum dose: 500 mg/dose
Skin and soft tissue infection, methicillin-susceptible Staphylococcus aureus (MSSA): Infants, Children, and Adolescents: Oral: 25 to 50 mg/kg/day divided every 6 hours; maximum dose: 500 mg/dose (IDSA [Stevens 2014])
Administration
Oral: Administer 1 hour before or 2 hours after meals with at least 120 mL of water. Administer around-the-clock to promote less variation in peak and trough serum levels. Should not be administered in the supine position or immediately before going to bed.
Storage
Store at 20°C to 25°C (68°F to 77°F).
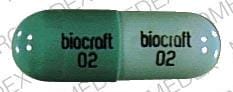
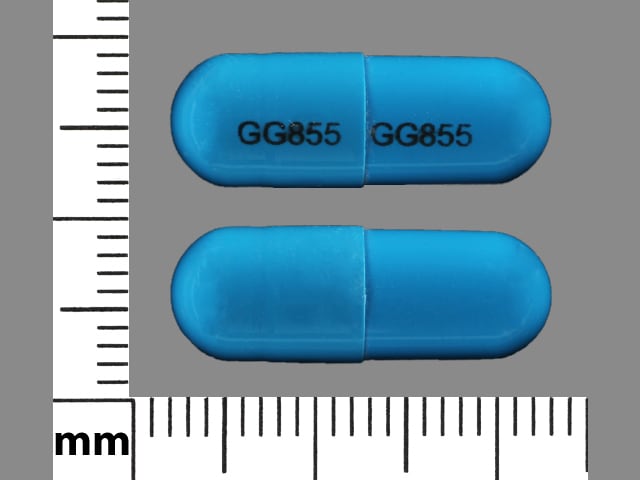
Dicloxacillin Images
Drug Interactions
Acemetacin: May increase the serum concentration of Penicillins. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CloZAPine: CYP3A4 Inducers (Weak) may decrease the serum concentration of CloZAPine. Monitor therapy
CYP2C19 Substrates (High risk with Inducers): CYP2C19 Inducers (Moderate) may decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Dichlorphenamide: Penicillins may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Methotrexate: Penicillins may increase the serum concentration of Methotrexate. Monitor therapy
Mycophenolate: Penicillins may decrease serum concentrations of the active metabolite(s) of Mycophenolate. This effect appears to be the result of impaired enterohepatic recirculation. Monitor therapy
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
Probenecid: May increase the serum concentration of Penicillins. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Tetracyclines: May diminish the therapeutic effect of Penicillins. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Dicloxacillin may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
False-positive urine and serum proteins; false-positive in uric acid, urinary steroids; may interfere with urinary glucose tests using cupric sulfate (Benedict's solution, Clinitest®); may inactivate aminoglycosides in vitro
Adverse Reactions
Frequency not defined.
1% to 10%: Gastrointestinal: Abdominal pain diarrhea, nausea
<1%, postmarketing, and/or case reports: Agranulocytosis, anemia, eosinophilia, fever, hematuria, hemolytic anemia, hepatotoxicity, hypersensitivity reaction, increased blood urea nitrogen, increased liver enzymes (transient), increased serum creatinine, interstitial nephritis, leukopenia, neutropenia, prolonged prothrombin time, pseudomembranous colitis, seizure (with extremely high doses and/or renal failure), serum sickness-like reaction, skin rash (maculopapular rash to exfoliative dermatitis), thrombocytopenia, vaginitis, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Hypersensitivity reactions: Serious and occasionally fatal hypersensitivity (anaphylactic shock with collapse) reactions have been reported in patients on penicillin therapy. Initiate therapy only after a comprehensive drug and allergy history; use with caution in patients with a history of significant allergies and/or asthma. Discontinue use and institute appropriate therapy if a hypersensitivity reaction occurs.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Neonates: Use with caution in neonates; elimination of drug is slow.
Monitoring Parameters
Baseline and periodic CBC with differential; periodic BUN, serum creatinine, AST and ALT (especially with prolonged therapy); prothrombin time if patient concurrently on warfarin; signs of anaphylaxis during first dose
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Dicloxacillin crosses the placenta (Depp 1970). Maternal use of penicillins has generally not resulted in an increased risk of birth defects.
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Shortness of breath
- Severe nausea
- Vomiting
- Mouth irritation
- Tongue discoloration
- Bruising
- Bleeding
- Sore throat
- Muscle pain
- Joint pain
- Joint swelling
- Severe dizziness
- Passing out
- Clostridium difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.