Boxed Warning
Mortality:
In the National Heart, Lung, and Blood Institute's Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multicenter, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had an MI more than 6 days but less than 2 years previously, an excessive mortality or nonfatal cardiac arrest rate (7.7%) was seen in patients treated with encainide or flecainide compared with that seen in patients assigned to carefully matched placebo-treated groups (3%). The average duration of treatment with encainide or flecainide in this study was 10 months.
The applicability of the CAST results to other populations (eg, those without recent MI) is uncertain. Considering the known proarrhythmic properties of disopyramide and the lack of evidence of improved survival for any antiarrhythmic drug in patients without life-threatening arrhythmias, the use of disopyramide as well as other antiarrhythmic agents should be reserved for patients with life-threatening ventricular arrhythmias.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
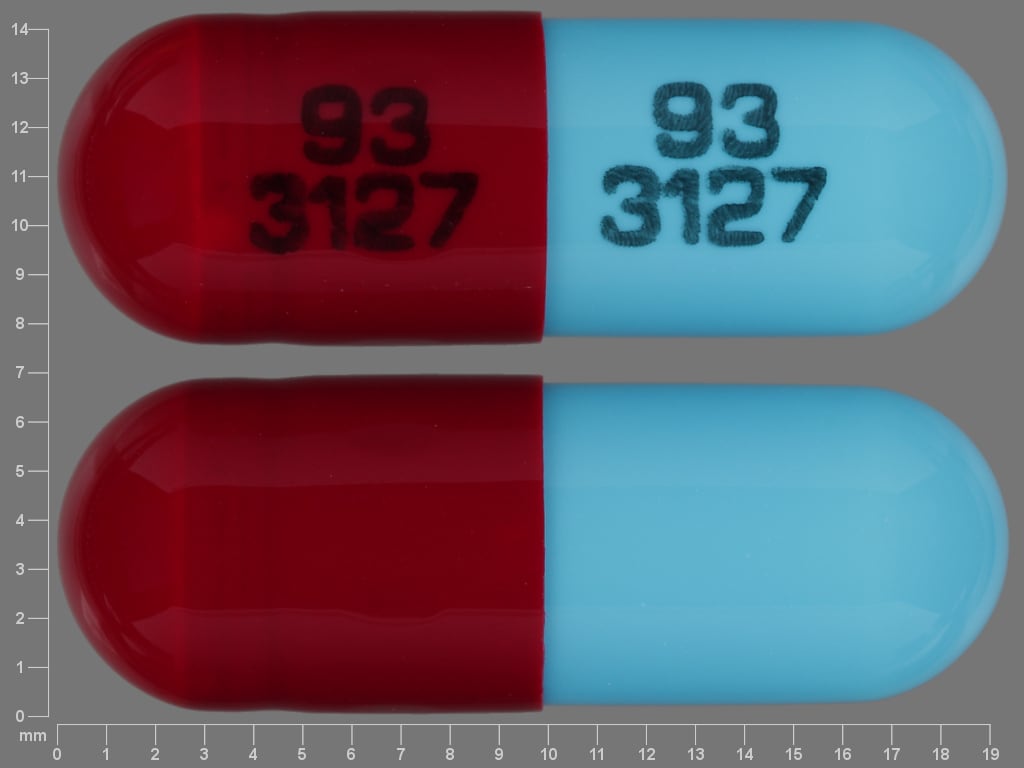
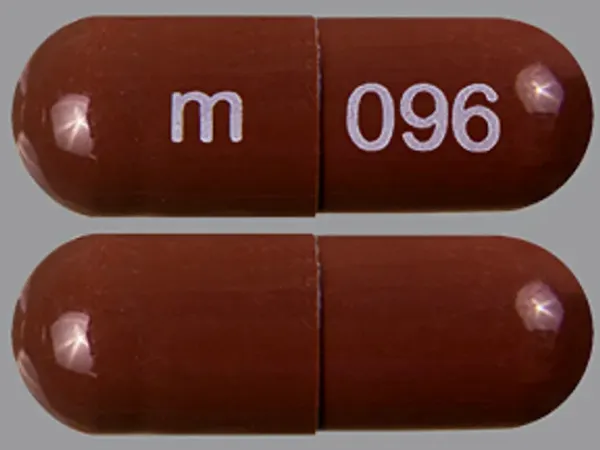
Capsule, Oral:
Norpace: 100 mg, 150 mg
Generic: 100 mg, 150 mg
Capsule Extended Release 12 Hour, Oral:
Norpace CR: 100 mg, 150 mg
Pharmacology
Mechanism of Action
Class Ia antiarrhythmic: Decreases myocardial excitability and conduction velocity; reduces disparity in refractory between normal and infarcted myocardium; possesses anticholinergic, peripheral vasoconstrictive, and negative inotropic effects
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and almost complete
Distribution
Vd: Children 5 to 12 years: 1.02 ± 0.2 L/kg (Chiba 1992); Adults: 0.8 to 2 L/kg
Metabolism
Hepatic; N-dealkylation to the active metabolite N-despropyldisopyramide (or mono-N-dealkylated [MND] metabolite) and other inactive metabolites
Excretion
Urine (~50% as unchanged drug; ~20% as MND; 10% other metabolites); feces (10% to 15%)
Clearance: Children 5 to 12 years: 3.79 ± 0.82 mL/minute/kg (Chiba 1992) (greater than adults)
Onset of Action
0.5 to 3.5 hours
Time to Peak
Serum: Immediate release: Within 2 hours; Controlled release: 4 to 7 hours
Duration of Action
Immediate release: 1.5 to 8.5 hours
Half-Life Elimination
Children 5 to 12 years: 3.15 ± 0.64 hours (Chiba 1992); Adults: 4 to 10 hours; prolonged with heart failure and hepatic or renal impairment
Protein Binding
Concentration dependent: 50% to 65%
Use in Specific Populations
Special Populations Note
Heart failure: Tmax and Cmax are increased.
Use: Labeled Indications
Ventricular arrhythmias: Life-threatening ventricular arrhythmias (eg, sustained ventricular tachycardia).
Use: Off Label
Atrial fibrillation (maintenance of sinus rhythm)yes
Based on the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with atrial fibrillation (AF), the use of disopyramide for maintenance of sinus rhythm in patients with AF or atrial flutter can be considered, especially in patients with vagally induced AF or when associated with hypertrophic cardiomyopathy (combined with a beta blocker or a non-dihydropyridine calcium channel blocker). Disopyramide is not recommended for use in patients with structural heart disease (other than hypertrophic cardiomyopathy).
Obstructive hypertrophic cardiomyopathybyes
Data from a prospective clinical registry in patients with obstructive hypertrophic cardiomyopathy (HCM) demonstrated reduced resting gradients with relief of symptoms associated with this condition and supports the use of disopyramide in the treatment of obstructive HCM Sherrid 2005. Data from one of the centers involved in this prospective registry further supports the role of added disopyramide in reducing resting gradients and relieving symptoms resistant to beta-blocker or verapamil therapy Sherrid 2013. Additional trials may be necessary to further define the role of disopyramide in the treatment of this condition.
Based on the 2011 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guideline for the diagnosis and treatment of hypertrophic cardiomyopathy, when patients do not respond to beta-blockers or verapamil alone, disopyramide may be used in the treatment of symptoms associated with obstructive HCM in combination with rate controlling agents (ie, beta blockers or verapamil) as it significantly reduces the left ventricular outflow gradient and improves symptoms. Some patients may not tolerate the anticholinergic effects (eg, dry mouth, urinary retention) and some patients may not improve with disopyramide and will require other nonpharmacologic interventions. When treating atrial fibrillation (AF) in patients with HCM, it is important to use disopyramide with either a beta blocker or verapamil since disopyramide enhances AV conduction during episodes of AF. Consideration should be given to discontinuing disopyramide when the HCM patient develops systolic dysfunction.
Contraindications
Hypersensitivity to disopyramide or any component of the formulation; cardiogenic shock; preexisting second- or third-degree heart block (except in patients with a functioning artificial pacemaker); congenital long QT syndrome
Canadian labeling: Additional contraindications (not in US labeling): Renal failure, severe intraventricular conduction defects (ie, bundle-branch block associated with first-degree atrioventricular block, double block [left posterior or anterior hemiblock and right bundle-branch block]); severe sinus node dysfunction; decompensated or inadequately compensated heart failure; concurrent use with other antiarrhythmics or other drugs capable of provoking ventricular arrhythmias (especially torsade de pointes); glaucoma; urinary retention
Dosage and Administration
Dosing: Adult
Atrial fibrillation (maintenance of sinus rhythm) (off-label use): Oral: Note: May be more desirable for patients with vagally-induced AF or hypertrophic cardiomyopathy associated with dynamic outflow tract obstruction; use in combination with a beta blocker or a non-dihydropyridine calcium channel blocker (AHA/ACC/HRS [January 2014]).
Immediate release: Usual dose: 100 to 200 mg every 6 hours
Controlled release: Usual dose: 200 to 400 mg every 12 hours
Hypertrophic cardiomyopathy (obstructive physiology) with or without atrial fibrillation (off-label use): Oral: Initial: Controlled release: 200 to 250 mg twice daily. If symptoms do not improve, increase by 100 mg/day at 2-week intervals to a maximum daily dose of 600 mg (ACC/AHA [Gersh 2011]; Sherrid 2005; Sherrid 2013). May consider the use of pyridostigmine to mitigate anticholinergic adverse effects (eg, urinary retention, constipation, dry mouth) associated with disopyramide (Sherrid 2013; Teichman 1987).
Ventricular arrhythmias: Oral: Note: Since newer agents with less toxicity are available, the use of disopyramide for this indication has fallen out of favor. Controlled release formulation is not to be used when rapid achievement of disopyramide plasma concentrations is desired. A maximum dose up to 400 mg every 6 hours (immediate release) may be required for patients with severe refractory ventricular tachycardia. Avoid loading dose in patients with cardiomyopathy or possible cardiac decompensation.
<50 kg:
Immediate release: An initial loading dose of 200 mg may be administered if rapid onset is required. Maintenance dose: 100 mg every 6 hours
Controlled release: Maintenance dose: 200 mg every 12 hours
≥50 kg:
Immediate release: An initial loading dose of 300 mg may be administered if rapid onset is required. Maintenance dose: 150 mg every 6 hours. If rapid control is necessary and no response seen within 6 hours of loading dose, may increase maintenance dose to 200 mg every 6 hours.
Controlled release: Maintenance dose: 300 mg every 12 hours
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Ventricular arrhythmias: Note: Patient should be hospitalized during the initial treatment and dose initiated at the lower end of dose range.
Immediate release: Oral:
Infants: 10 to 30 mg/kg/day in divided doses every 6 hours
Children 1 to 4 years: 10 to 20 mg/kg/day in divided doses every 6 hours
Children >4 to 12 years: 10 to 15 mg/kg/day in divided doses every 6 hours
Children >12 and Adolescents ≤18 years: 6 to 15 mg/kg/day in divided doses every 6 hours; adult maximum daily dose: 1,600 mg/day
Extemporaneously Prepared
10 mg/mL Oral Suspension
A 10 mg/mL suspension may be prepared using the 100 mg immediate-release capsules. Empty the contents of ten 100 mg capsules into a mortar. Triturate with cherry syrup and transfer mixture to graduated amber glass bottle. Rinse mortar with cherry syrup and add sufficient quantity of cherry syrup to make 100 mL. Label as “shake well” and “refrigerate.” Stable for 4 weeks in amber glass bottles stored at 5°C (41°F), 30°C (86°F), or at room temperature. Note: Do not use extended release capsules for this suspension.
Mathur LK, Lai PK, Shively CD. Stability of disopyramide phosphate in cherry syrup. Am J Hosp Pharm. 1982;39(2):309-310.7058805
Administration
Do not break or chew controlled release capsules. Administer around-the-clock rather than 4 times/day (ie, 12-6-12-6, not 9-1-5-9) to promote less variation in peak and trough serum levels. Should be taken on an empty stomach.
Dietary Considerations
Should be taken on an empty stomach.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Disopyramide Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ajmaline: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). QT-prolonging Class IA Antiarrhythmics (Highest Risk) may increase the serum concentration of Ajmaline. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amiodarone: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Beta-Blockers: Disopyramide may enhance the bradycardic effect of Beta-Blockers. Beta-Blockers may enhance the negative inotropic effect of Disopyramide. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Ceritinib: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ceritinib. Ceritinib may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Crizotinib: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Crizotinib. Crizotinib may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Crizotinib may increase the serum concentration of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Disopyramide. Exceptions: Crizotinib; Dronedarone; Erythromycin (Systemic); Fluconazole; Nilotinib; Ribociclib. Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erythromycin (Systemic): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Erythromycin (Systemic) may increase the serum concentration of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Etravirine: May decrease the serum concentration of Disopyramide. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Flecainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flecainide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fluconazole: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Disopyramide may enhance the QTc-prolonging effect of Fosphenytoin. Fosphenytoin may decrease the serum concentration of Disopyramide. Management: Seek alternatives when possible. Monitor patients receiving this combination closely for evidence of QT interval prolongation or changes in cardiac rhythm, as well as for decreased serum concentrations/therapeutic effects of disopyramide. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Gemifloxacin: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Halofantrine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Haloperidol: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Itraconazole: May increase the serum concentration of Disopyramide. Avoid combination
Ketoconazole (Systemic): May increase the serum concentration of Disopyramide. Avoid combination
Lacosamide: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lefamulin: May enhance the QTc-prolonging effect of QT-prolonging CYP3A4 Substrates. Management: Do not use lefamulin tablets with QT-prolonging CYP3A4 substrates. Lefamulin prescribing information lists this combination as contraindicated. Avoid combination
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Avoid combination
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lidocaine (Systemic): Disopyramide may enhance the arrhythmogenic effect of Lidocaine (Systemic). Disopyramide may increase the serum concentration of Lidocaine (Systemic). Specifically, the unbound/free fraction of lidocaine. Monitor therapy
Lidocaine (Topical): Disopyramide may enhance the arrhythmogenic effect of Lidocaine (Topical). Disopyramide may increase the serum concentration of Lidocaine (Topical). Specifically, the unbound/free fraction of lidocaine. Monitor therapy
Lofexidine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Lofexidine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lurasidone: May enhance the QTc-prolonging effect of Disopyramide. Management: Consider alternatives to disopyramide in patients with acute lurasidone overdose. If disopyramide treatment cannot be avoided, monitor for excessive QTc interval prolongation. Consider therapy modification
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Methadone: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ondansetron: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
PHENobarbital: May decrease the serum concentration of Disopyramide. Monitor therapy
Phenytoin: May decrease the serum concentration of Disopyramide. Monitor therapy
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Posaconazole: May increase the serum concentration of QT-prolonging CYP3A4 Substrates. Such increases may lead to a greater risk for proarrhythmic effects and other similar toxicities. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Propafenone: May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of other QT-prolonging Class IA Antiarrhythmics (Highest Risk). Exceptions: Ajmaline. Avoid combination
QT-prolonging Class III Antiarrhythmics (Highest Risk): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
RifAMPin: May decrease the serum concentration of Disopyramide. Monitor therapy
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Saquinavir: May enhance the QTc-prolonging effect of Disopyramide. Saquinavir may increase the serum concentration of Disopyramide. Avoid combination
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Telithromycin: May enhance the QTc-prolonging effect of Disopyramide. Telithromycin may increase the serum concentration of Disopyramide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Verapamil: May enhance the adverse/toxic effect of Disopyramide. Of particular concern is the potential for profound depression of myocardial contractility. Management: Concurrent use of disopyramide within 48 hours prior to or 24 hours after verapamil should be avoided. Avoid combination
Voriconazole: QT-prolonging Class IA Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Voriconazole. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Adverse Reactions
Frequency not always defined. The most common adverse effects are related to cholinergic blockade. The most serious adverse effects of disopyramide are hypotension and cardiac failure.
>10%:
Gastrointestinal: Xerostomia (32%), constipation (11%)
Genitourinary: Urinary hesitancy (14% to 23%)
1% to 10%:
Cardiovascular: Cardiac conduction disturbance, cardiac failure, chest pain, edema, hypotension, syncope
Central nervous system: Dizziness, fatigue, headache, malaise, myasthenia, nervousness
Dermatologic: Generalized dermatosis, pruritus, skin rash
Endocrine & metabolic: Hypokalemia, increased serum cholesterol, increased serum triglycerides, weight gain
Gastrointestinal: Abdominal distention, anorexia, bloating, diarrhea, flatulence, nausea, vomiting
Genitourinary: Impotence (1% to 3%), urinary frequency, urinary retention, urinary urgency
Neuromuscular & skeletal: Myalgia
Ophthalmic: Blurred vision, xerophthalmia
Respiratory: Dry throat, dyspnea
<1%, postmarketing, and/or case reports: Agranulocytosis, atrioventricular block, cardiac arrhythmia (new or worsened; proarrhythmic effect), cholestatic jaundice, decreased hematocrit, decreased hemoglobin, depression, dysuria, fever, gynecomastia, hepatotoxicity, hypoglycemia, increased blood urea nitrogen, increased serum creatinine, increased serum transaminases, insomnia, mydriasis, numbness, paresthesia, peripheral neuropathy, psychosis, psychotic reaction, respiratory distress, skin blister (toxic), systemic lupus erythematosus (rare; generally in patients previously receiving procainamide), thrombocytopenia, tingling sensation
Warnings/Precautions
Concerns related to adverse effects:
- Hypotension: May occur during the initiation of therapy; monitor closely.
- Proarrhythmic effects: Monitor for proarrhythmic effects; may cause QTc prolongation and subsequent torsade de pointes; avoid use in patients with diagnosed or suspected congenital long QT syndrome. Monitor and adjust dose to prevent QTc prolongation. Increases in QTc >25% over baseline should result in cessation or reduction in disopyramide dosing. Because of the risk of QTc prolongation and arrhythmias, disopyramide should be initiated within the hospital with cardiac monitoring. In patients with preexisting cardiovascular disease, the incidence of proarrhythmic effects and mortality may be increased with Class Ia antiarrhythmic agents.
Disease-related concerns:
- Atrial fibrillation/flutter: May increase ventricular response rate in patients with atrial fibrillation or flutter; control AV conduction before initiating.
- BPH/urinary retention: Do not use in patients with BPH and/or urinary retention due to significant anticholinergic effects.
- Conduction disturbances: Use with caution in patients with bundle branch block or heart block.
- Electrolyte imbalance: Correct electrolyte disturbances, especially hypokalemia or hypomagnesemia, prior to use and throughout therapy.
- Glaucoma: Do not use in patients with glaucoma due to significant anticholinergic effects.
- Heart failure: Use with caution or avoid in patients with any degree of left ventricular dysfunction or history of heart failure; may precipitate or exacerbate condition.
- Hepatic impairment: Use with caution in patients with hepatic impairment; reduced dosage recommended.
- Myasthenia gravis: Do not use in patients with myasthenia gravis due to significant anticholinergic effects.
- Renal impairment: Use with caution in renal impairment; reduced dosage recommended. The controlled release form is not recommended for CrCl ≤40 mL/minute.
- Wolff-Parkinson-White syndrome: Use with caution in patients with Wolff-Parkinson-White syndrome.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- CAST trial: [US Boxed Warning]: In the Cardiac Arrhythmia Suppression Trial (CAST), recent (>6 days but <2 years ago) myocardial infarction patients with asymptomatic, non-life-threatening ventricular arrhythmias did not benefit and may have been harmed by attempts to suppress the arrhythmia with flecainide or encainide. An increased mortality or nonfatal cardiac arrest rate (7.7%) was seen in the active treatment group compared with patients in the placebo group (3%). The applicability of the CAST results to other populations is unknown. Antiarrhythmic agents should be reserved for patients with life-threatening ventricular arrhythmias.
Monitoring Parameters
ECG, blood pressure, urinary retention, CNS anticholinergic effects (confusion, agitation, hallucinations, etc); disopyramide drug level (if available); signs and symptoms of heart failure
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Disopyramide levels have been reported in human fetal blood. Disopyramide may stimulate contractions in pregnant women. In a case report, disopyramide use in the third trimester resulted in painful uterine contractions after the first dose and hemorrhage after the second dose (Abbi 1999).
Patient Education
What is this drug used for?
- It is used to treat certain types of abnormal heartbeats.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Constipation
- Dry mouth or throat
- Nasal dryness
- Dry eyes
- Loss of strength and energy
- Fatigue
- Bloating
- Passing gas
- Nausea
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Chest pain
- Muscle weakness
- Fast heartbeat
- Abnormal heartbeat
- Severe dizziness
- Passing out
- Vision changes
- Trouble urinating
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.