Boxed Warning
Alcohol intoxication:
Disulfiram should never be administered to a patient when he is in a state of alcohol intoxication, or without his full knowledge. The physician should instruct relatives accordingly.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Antabuse: 250 mg
Antabuse: 500 mg [scored]
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Disulfiram is a thiuram derivative which blocks the oxidation of alcohol at the acetaldehyde stage. When taken concomitantly with alcohol, there is an increase in serum acetaldehyde levels. High acetaldehyde causes uncomfortable symptoms including flushing, throbbing in head and neck, nausea, vomiting, diaphoresis, thirst, palpitations, chest pain, dyspnea, hyperventilation, tachycardia, syncope, weakness, blurred vision, confusion, vertigo, and hypotension. This reaction is the basis for disulfiram use in post-withdrawal long-term care of alcohol use disorder.
Pharmacokinetics/Pharmacodynamics
Absorption
Slow
Metabolism
Reduction of disulfide linkage to diethyldithiocarbamic acid, then further metabolized via glucuronidation, non-enzymatic degradation, methylation and oxidation (Eneanya 1981)
Excretion
Feces (20% unchanged) and exhaled gases (as metabolites), urine (50% metabolites) (Eneanya 1981)
Onset of Action
Full effect: 12 hours
Duration of Action
~1 to 2 weeks after last dose
Use: Labeled Indications
Alcohol use disorder: Management of chronic alcohol use disorder.
Note: Suggested for use in patients with alcohol use disorder (moderate to severe) who want to abstain from alcohol and either prefer disulfiram or are unable to tolerate or are unresponsive to naltrexone and acamprosate (APA [Reus 2018]).
Contraindications
Hypersensitivity to disulfiram or any component of the formulation or to other thiuram derivatives used in pesticides and rubber vulcanization; patients receiving or using alcohol, metronidazole, paraldehyde, or alcohol-containing preparations (eg, cough syrup, tonics); psychosis; severe myocardial disease or coronary occlusion.
Dosage and Administration
Dosing: Adult
Alcohol use disorder: Oral: Note: Do not administer until the patient has abstained from alcohol for at least 12 hours.
Initial: Up to 500 mg once daily for 1 to 2 weeks (maximum: 500 mg/day)
Average maintenance dose: 250 mg once daily (range: 125 to 500 mg/day; maximum: 500 mg/day).
Dosing: Geriatric
Refer to adult dosing; use with caution, starting at low end of dosing range.
Administration
Administration of any medications containing alcohol, including topicals, is contraindicated. Do not administer disulfiram if alcohol has been consumed within the prior 12 hours. Morning administration is preferred, but may be given at bedtime if sedation is experienced. Tablets may be crushed and mixed with liquids.
Dietary Considerations
Do not administer disulfiram if alcohol has been consumed within the prior 12 hours.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light.
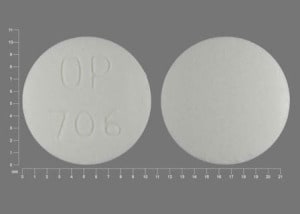
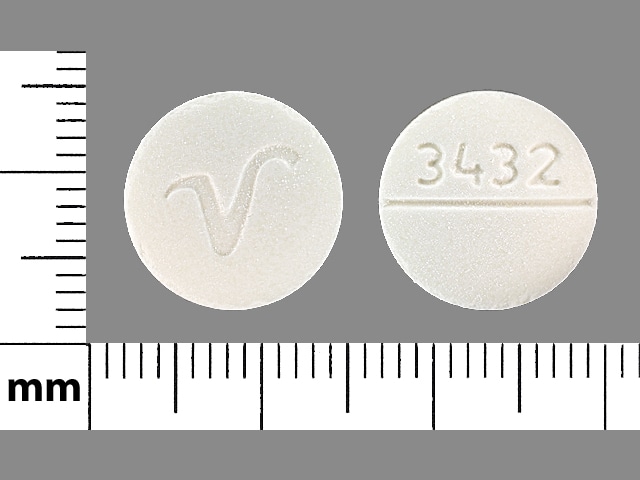
Disulfiram Images
Drug Interactions
Alcohol (Ethyl): Disulfiram may enhance the adverse/toxic effect of Alcohol (Ethyl). A disulfiram-like reaction may occur. Avoid combination
Atazanavir: May diminish the therapeutic effect of Disulfiram. Monitor therapy
Bacampicillin: May enhance the adverse/toxic effect of Disulfiram. Avoid combination
Benznidazole: May enhance the adverse/toxic effect of Disulfiram. In particular, the risk for CNS toxicities such as psychosis may be increased. Avoid combination
Carbocisteine: Disulfiram may enhance the adverse/toxic effect of Carbocisteine. Specifically, disulfiram may enhance adverse effects of alcohol that is present in liquid formulations of carbocisteine-containing products. Avoid combination
ChlordiazePOXIDE: Disulfiram may increase the serum concentration of ChlordiazePOXIDE. Monitor therapy
Chlorzoxazone: Disulfiram may increase the serum concentration of Chlorzoxazone. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cocaine (Topical): Disulfiram may increase the serum concentration of Cocaine (Topical). Avoid combination
CYP2E1 Substrates (High risk with Inhibitors): CYP2E1 Inhibitors (Strong) may decrease the metabolism of CYP2E1 Substrates (High risk with Inhibitors). Consider therapy modification
DiazePAM: Disulfiram may increase the serum concentration of DiazePAM. Monitor therapy
Dronabinol: Disulfiram may enhance the adverse/toxic effect of Dronabinol. Specifically, disulfiram may produce severe intolerance to the alcohol contained in the dronabinol oral solution. Consider therapy modification
Fexinidazole [INT]: May enhance the adverse/toxic effect of Disulfiram. Avoid combination
Flunitrazepam: Disulfiram may increase the serum concentration of Flunitrazepam. Monitor therapy
Fosphenytoin: Disulfiram may increase the serum concentration of Fosphenytoin. Management: Avoid concomitant use of disulfiram and phenytoin when possible. Phenytoin dose adjustment will likely be necessary when starting and/or stopping concurrent disulfiram. Monitor phenytoin response and concentrations closely. Consider therapy modification
Isoniazid: Disulfiram may enhance the adverse/toxic effect of Isoniazid. Disulfiram may increase the serum concentration of Isoniazid. Monitor therapy
Lopinavir: May enhance the adverse/toxic effect of Disulfiram. Specifically, the combination of lopinavir/ritonavir solution, which contains 42% alcohol, may result in a disulfiram-alcohol reaction if combined. Avoid combination
MetroNIDAZOLE (Systemic): Disulfiram may enhance the adverse/toxic effect of MetroNIDAZOLE (Systemic). In particular, the risk for CNS toxicities such as psychosis may be increased. Avoid combination
MetroNIDAZOLE (Topical): May enhance the adverse/toxic effect of Disulfiram. In particular, the risk for CNS toxicities such as psychosis may be increased. Management: Warn patients and monitor for the development of serious CNS toxicity if topical metronidazole is used in a patient taking disulfiram. Some manufacturers of vaginal metronidazole products list disulfiram use within 2 weeks as a contraindication. Consider therapy modification
Paraldehyde: Disulfiram may increase the serum concentration of Paraldehyde. Avoid combination
Phenytoin: Disulfiram may increase the serum concentration of Phenytoin. Management: Avoid concomitant use of disulfiram and phenytoin when possible. Phenytoin dose adjustment will likely be necessary when starting and/or stopping concurrent disulfiram. Monitor phenytoin response and concentrations closely. Consider therapy modification
Ritonavir: May enhance the adverse/toxic effect of Disulfiram. Specifically, the combination of ritonavir oral solution, which contains 43% alcohol, may result in a disulfiram-alcohol reaction if combined. Avoid combination
Sertraline: Disulfiram may enhance the adverse/toxic effect of Sertraline. This is specifically related to sertraline oral concentrate due to its alcohol content (12%). Management: Sertraline Oral Concentrate contains 12% alcohol, and its use should be avoided with disulfiram. Avoid combination
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Tinidazole: May enhance the adverse/toxic effect of Disulfiram. Avoid combination
Tipranavir: Disulfiram may enhance the adverse/toxic effect of Tipranavir. Consider therapy modification
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Disulfiram may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
Frequency not defined.
Central nervous system: Bitter taste (garlic), drowsiness, fatigue, headache, metallic taste, peripheral neuritis, peripheral neuropathy, polyneuropathy, psychosis
Dermatologic: Acneiform eruption, allergic dermatitis, skin rash
Genitourinary: Impotence
Hepatic: Cholestatic hepatitis, fulminant hepatitis, hepatic failure (multiple case reports)
Ophthalmic: Optic neuritis
Warnings/Precautions
Concerns related to adverse effects:
- Disulfiram reaction: Ingesting alcohol, even in small amounts, during treatment with disulfiram may result in flushing, throbbing in head and neck, nausea, copious vomiting, respiratory difficulty, diaphoresis, thirst, chest pain, palpitation, dyspnea, hyperventilation, tachycardia, hypotension, syncope, marked uneasiness, weakness, vertigo, blurred vision and confusion. Severe reactions may involve respiratory depression, cardiovascular collapse, arrhythmias, myocardial infarction, acute congestive heart failure, unconsciousness, seizure and death. The intensity of the reaction is generally proportional to the amounts of disulfiram and alcohol ingested. The reaction can last from 30 minutes to several hours in more severe cases, or as long as it takes the alcohol to be metabolized. Patients should avoid alcohol consumption for >12 hours prior to administration; disulfiram reactions can occur up to 14 days after taking disulfiram if alcohol is consumed (APA [Reus 2018]).
- Hepatotoxicity: Severe (sometimes fatal) hepatitis and/or hepatic failure resulting in transplantation have been associated with use; may occur in patients with or without prior history of abnormal hepatic function. Monitor for hepatotoxicity and educate patients about signs and symptoms.
Disease-related concerns:
- Cerebral damage: Use with extreme caution in patients with cerebral damage.
- Contact dermatitis: Evaluate patients with a history of rubber contact dermatitis for hypersensitivity to thiuram derivatives before administering disulfiram.
- Diabetes: Use with extreme caution in patients with diabetes mellitus.
- Hepatic impairment: Use with extreme caution in patients with hepatic cirrhosis or impairment.
- Hypothyroidism: Use with extreme caution in patients with hypothyroidism.
- Nephritis: Use with extreme caution in patients with acute or chronic nephritis.
- Seizures: Use with extreme caution in patients with a history of seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Alcohol intoxication: [US Boxed Warning]: Should never be administered to a patient when he/she is in a state of alcohol intoxication, or without his/her knowledge. The physician should instruct relatives accordingly.
- Patient information: Patients must receive appropriate counseling, including information on the disulfiram reaction, “disguised” forms of alcohol (eg, tonics, mouthwashes, cough mixtures, sauces, vinegars, aftershave lotions, back rubs) and the duration of drug activity (up to 14 days).
Monitoring Parameters
Liver function tests (baseline and after 10 to 14 days of treatment), CBC, serum chemistries; cardiac function at baseline if clinically appropriate (APA [Reus 2018])
Pregnancy
Pregnancy Considerations
Safety in pregnancy has not been established; there is limited data on maternal use during pregnancy (Reitnauer 1997).
Pharmacological agents should not be used for the treatment of alcohol use disorder in pregnant women unless needed for the treatment of acute alcohol withdrawal or a coexisting disorder; agents other than disulfiram are recommended for acute alcohol withdrawal.
Patient Education
What is this drug used for?
- It is used to help you stop drinking alcohol.
- It is used to help keep you alcohol-free.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Sexual dysfunction
- Acne
- Headache
- Change in taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Vision changes
- Burning or numbness feeling
- Mood changes
- Behavioral changes
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.