Boxed Warning
Arrhythmias:
To minimize the risk of induced arrhythmia, patients initiated or re-initiated on dofetilide should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous electrocardiographic monitoring, and cardiac resuscitation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
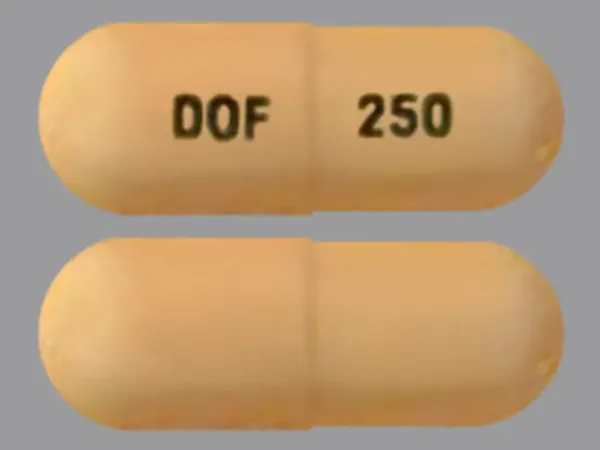
Capsule, Oral:
Tikosyn: 125 mcg, 250 mcg, 500 mcg [contains corn starch]
Generic: 125 mcg, 250 mcg, 500 mcg
Pharmacology
Mechanism of Action
Vaughan Williams Class III antiarrhythmic activity. Blockade of the cardiac ion channel carrying the rapid component of the delayed rectifier potassium current. Dofetilide has no effect on sodium channels, adrenergic alpha-receptors, or adrenergic beta-receptors. It increases the monophasic action potential duration due to delayed repolarization. The increase in the QT interval is a function of prolongation of both effective and functional refractory periods in the His-Purkinje system and the ventricles. Changes in cardiac conduction velocity and sinus node function have not been observed in patients with or without structural heart disease. PR and QRS width remain the same in patients with preexisting heart block and or sick sinus syndrome.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Vd: 3 L/kg
Metabolism
Hepatic via CYP3A4 (low affinity); metabolites formed by N-dealkylation and N-oxidation
Excretion
Urine (80%; ~80% as unchanged drug, 20% as inactive or minimally active metabolites); renal elimination consists of glomerular filtration and active tubular secretion via cationic transport system
Time to Peak
Serum: Fasting: 2 to 3 hours
Half-Life Elimination
~10 hours; prolonged with renal impairment
Protein Binding
60% to 70%
Use in Specific Populations
Special Populations: Renal Function Impairment
Clearance is decreased and half-life is prolonged with decreasing CrCl.
Special Populations: Gender
Women have approximately 12% to 18% lower clearance.
Use: Labeled Indications
Atrial fibrillation/atrial flutter: Maintenance of normal sinus rhythm in patients with chronic atrial fibrillation/atrial flutter of longer than 1-week duration who have been converted to normal sinus rhythm; conversion of atrial fibrillation and atrial flutter to normal sinus rhythm.
Use: Off Label
Atrial fibrillation in patients with hypertrophic cardiomyopathyyes
Based on the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy, dofetilide is an effective and recommended alternative antiarrhythmic for the treatment of atrial fibrillation in patients with hypertrophic cardiomyopathy especially in patients with an implantable cardioverter defibrillator (ICD).
Supraventricular tachycardiayes
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines for the management of patients with supraventricular arrhythmias, dofetilide may be a therapeutic option for the ongoing management of symptomatic supraventricular arrhythmias (atrioventricular nodal reentrant tachycardia or atrioventricular reentrant tachycardia) in patients who are not candidates for, or prefer not to undergo, catheter ablation and in whom other therapies have failed or are contraindicated. Dofetilide may also be reasonable for the acute treatment or ongoing management of hemodynamically stable patients with adult congenital heart disease and recurrent atrial flutter or focal atrial tachycardia.
Contraindications
Hypersensitivity to dofetilide or any component of the formulation; congenital or acquired long QT syndromes; patients with baseline QT interval or QTc >440 msec (500 msec in patients with ventricular conduction abnormalities); severe renal impairment (CrCl <20 mL/minute); concurrent use with cimetidine, dolutegravir, hydrochlorothiazide (alone or in combinations), itraconazole (according to itraconazole prescribing information), ketoconazole, megestrol, prochlorperazine, trimethoprim (alone or in combination), or verapamil
Dosage and Administration
Dosing: Adult
Note: CrCl and QTc interval (or QT interval if heart rate is <60 beats/minute) must be determined prior to first dose. If QTc >440 msec (>500 msec in patients with ventricular conduction abnormalities), dofetilide is contraindicated. Adjust initial dosage in patients with estimated CrCl <60 mL/minute (see dosage adjustment in renal impairment). Dofetilide may be initiated at lower doses than recommended based on physician discretion; however, if the lower dose is increased, the patient will require rehospitalization for 3 days.
Atrial fibrillation/atrial flutter: Oral: Initial: 500 mcg twice daily (maximum dose: 500 mcg twice daily)
Supraventricular tachycardia (ongoing management) (off-label use): Oral: Initial: 500 mcg every 12 hours (ACC/AHA/HRS [Page 2015])
Modification of dosage in response to initial dose: QTc interval should be measured 2 to 3 hours after the initial dose. If the QTc interval increases to more than 15% above baseline QTc or if the QTc is >500 msec (>550 msec in patients with ventricular conduction abnormalities), dofetilide dose should be reduced by 50%. If the starting dose was 500 mcg twice daily, then reduce to 250 mcg twice daily. If the starting dose was 250 mcg twice daily, then reduce to 125 mcg twice daily. If the starting dose was 125 mcg twice daily, then reduce to 125 mcg once daily. QTc interval should be measured 2 to 3 hours after each subsequent dose (in-hospital doses 2 through 5). If at any time after the second dose the QTc is >500 msec (>550 msec in patients with ventricular conduction abnormalities), dofetilide should be discontinued.
Maintenance therapy: No further down titration of dose based on QTc is recommended following modification of initial dose. Renal function and QTc should be re-evaluated every 3 months or as medically warranted. If QTc >500 msec (>550 msec in patients with ventricular conduction abnormalities), discontinue therapy. If renal function deteriorates, adjust dose as described in dosage adjustment in renal impairment.
Dosing: Geriatric
Refer to adult dosing. No specific dosage adjustments are recommended based on age; however, careful assessment of renal function is particularly important in this population.
Administration
Oral: Administer with or without food.
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from moisture and humidity.
Dofetilide Images
Drug Interactions
AMILoride: May increase the serum concentration of Dofetilide. Monitor therapy
Amiodarone: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amisulpride: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Amisulpride. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Azithromycin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Bictegravir: May increase the serum concentration of Dofetilide. Avoid combination
Ceritinib: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ceritinib. Ceritinib may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Chloroquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Cimetidine: May increase the serum concentration of Dofetilide. This is likely via inhibition of dofetilide renal tubular secretion (primarily) and inhibition of dofetilide metabolism. Avoid combination
Citalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Citalopram. Avoid combination
Clarithromycin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clarithromycin. Avoid combination
Clofazimine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
CloZAPine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Cobicistat: May increase the serum concentration of Dofetilide. Monitor therapy
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Dofetilide. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Dofetilide. Monitor therapy
CYP3A4 Inhibitors (Weak): May increase the serum concentration of Dofetilide. Monitor therapy
Dasatinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Dasatinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Dolutegravir: May increase the serum concentration of Dofetilide. Avoid combination
Domperidone: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Domperidone. Avoid combination
Doxepin-Containing Products: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Doxepin-Containing Products. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Droperidol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Erythromycin (Systemic): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Erythromycin (Systemic). Erythromycin (Systemic) may enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Avoid concomitant use of erythromycin and class III antiarrhythmic agents. Use of erythromycin with dronedarone is specifically contraindicated. Avoid combination
Escitalopram: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Escitalopram. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Avoid combination
Fingolimod: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Flecainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flecainide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Flupentixol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Flupentixol. Avoid combination
Gadobenate Dimeglumine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Gemifloxacin: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Gilteritinib: May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Consider alternatives to this combination. If use is necessary, monitor for QTc interval prolongation and arrhythmias. Consider therapy modification
Halofantrine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Haloperidol: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
HydroCHLOROthiazide: May enhance the QTc-prolonging effect of Dofetilide. HydroCHLOROthiazide may increase the serum concentration of Dofetilide. Avoid combination
Inotuzumab Ozogamicin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Itraconazole: May increase the serum concentration of Dofetilide. Avoid combination
Ketoconazole (Systemic): May increase the serum concentration of Dofetilide. Avoid combination
Lacosamide: Antiarrhythmic Agents (Class III) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
LamoTRIgine: May increase the serum concentration of Dofetilide. Avoid combination
Lefamulin: May enhance the QTc-prolonging effect of QT-prolonging CYP3A4 Substrates. Management: Do not use lefamulin tablets with QT-prolonging CYP3A4 substrates. Lefamulin prescribing information lists this combination as contraindicated. Avoid combination
Levofloxacin-Containing Products (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
Lidocaine (Topical): May enhance the arrhythmogenic effect of Antiarrhythmic Agents (Class III). Antiarrhythmic Agents (Class III) may increase the serum concentration of Lidocaine (Topical). This mechanism specifically applies to amiodarone and dronedarone. Monitor therapy
Lofexidine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Lofexidine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Loop Diuretics: May enhance the QTc-prolonging effect of Dofetilide. Management: Monitor serum potassium and magnesium more closely when dofetilide is combined with loop diuretics. Some therapy modification may be required. Consider therapy modification
Megestrol: May increase the serum concentration of Dofetilide. Avoid combination
MetFORMIN: May increase the serum concentration of Dofetilide. Monitor therapy
Methadone: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Midostaurin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Moxifloxacin (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Moxifloxacin (Systemic). Avoid combination
Nilotinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Nilotinib. Avoid combination
OLANZapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Ondansetron: QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Osimertinib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Osimertinib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Pentamidine (Systemic): QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pilsicainide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pilsicainide. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Pimozide: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Pimozide. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Avoid combination
Piperaquine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Piperaquine. Avoid combination
Posaconazole: May increase the serum concentration of Dofetilide. Avoid combination
Probucol: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Probucol. Avoid combination
Prochlorperazine: May increase the serum concentration of Dofetilide. Avoid combination
Propafenone: May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Agents (Indeterminate Risk - Avoid): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Agents (Indeterminate Risk - Caution): May enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of other QT-prolonging Class III Antiarrhythmics (Highest Risk). Avoid combination
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Miscellaneous Agents (Highest Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Erythromycin (Systemic); Nilotinib; Ribociclib. Consider therapy modification
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): QT-prolonging Class III Antiarrhythmics (Highest Risk) may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Ceritinib; Clarithromycin. Consider therapy modification
QUEtiapine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of QUEtiapine. Avoid combination
Ribociclib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Ribociclib. Avoid combination
RisperiDONE: QT-prolonging Agents (Highest Risk) may enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sodium Stibogluconate: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Sparfloxacin: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Sparfloxacin. Avoid combination
Tafenoquine: May increase the serum concentration of MATE1 Substrates. Management: Avoid use of MATE substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the MATE substrate and consider a reduced dose of the MATE substrate according to that substrate's labeling. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May enhance the QTc-prolonging effect of Dofetilide. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Dofetilide. Management: Although hydrochlorothiazide is specifically cited as a contraindication, the risk likely extends to all thiazide and thiazide-like diuretics and may be even greater with chlorthalidone or bendroflumethiazide. Consider alternatives when possible. Exceptions: HydroCHLOROthiazide. Consider therapy modification
Thioridazine: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Thioridazine. Avoid combination
Triamterene: May increase the serum concentration of Dofetilide. Monitor therapy
Trimethoprim: May increase the serum concentration of Dofetilide. Avoid combination
Vemurafenib: QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of Vemurafenib. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
Verapamil: May increase the serum concentration of Dofetilide. Avoid combination
Adverse Reactions
>10%:
Cardiovascular: Torsades de pointes (patients receiving doses in excess of those recommended: ≤11%; cardiac failure patients: 3%; patients with recent myocardial infarction: <1%; occurs most frequently within the first 3 days of therapy)
Central nervous system: Headache (11%)
1% to 10%:
Cardiovascular: Chest pain (10%), ventricular fibrillation (≤5%), ventricular tachycardia (3% to 4%), bradycardia (≤2%), cardiac arrest (≤2%), cerebral ischemia (≤2%), cerebrovascular accident (≤2%), edema (≤2%), myocardial infarction (≤2%), syncope (≤2%), atrioventricular block (<2%), heart block (1%)
Central nervous system: Dizziness (8%), insomnia (4%), facial paralysis (≤2%), flaccid paralysis (≤2%), migraine (≤2%), paralysis (≤2%), paresthesia (≤2%)
Dermatologic: Skin rash (3%)
Gastrointestinal: Nausea (5%), abdominal pain (3%), diarrhea (3%)
Hepatic: Hepatotoxicity (≤2%), hepatic injury (<2%)
Hypersensitivity: Angioedema (≤2%)
Neuromuscular & skeletal: Back pain (3%)
Respiratory: Respiratory tract infection (7%), dyspnea (6%), flu-like symptoms (4%), increased cough (≤2%), cough (<2%)
Miscellaneous: Accidental injury (3%), surgery (3%)
<1%, postmarketing, and/or case reports: Bundle branch block
Warnings/Precautions
Concerns related to adverse effects:
- Proarrhythmic effects: May cause serious ventricular arrhythmias, primarily torsades de pointes (TdP). Watch for proarrhythmic effects; monitor and adjust dose to prevent QTc prolongation; reduced CrCl or certain dofetilide drug interactions will increase dofetilide plasma concentration. Risk of TdP significantly increases with doses greater than the maximum dose of 500 mcg twice daily. The risk of TdP may be higher in certain patient subgroups (eg, patients with heart failure). Most episodes of TdP occur within the first 3 days of therapy.
Disease-related concerns:
- Arrhythmias: Appropriate use: Reserve for patients who are highly symptomatic with atrial fibrillation/atrial flutter. [US Boxed Warning]: Must be initiated (or reinitiated) in a setting that can provide continuous monitoring of CrCl and ECG monitoring and cardiac resuscitation with staff familiar with the recognition and treatment of life-threatening arrhythmias for a minimum of 3 days, or for a minimum of 12 hours after electrical or pharmacological cardioversion to normal sinus rhythm, whichever is greater. Patients should be readmitted for continuous monitoring if dosage is later increased.
- Conduction disturbances: Use with caution in patients with second or third-degree heart block and/or sick sinus syndrome unless a functional pacemaker is in place; these patients were not included in phase 3 clinical trials. However, no effect on AV nodal conduction seen in patients with normal conduction and those with first-degree heart block. Defibrillation threshold is reduced in patients with ventricular tachycardia or ventricular fibrillation undergoing implantation of a cardioverter-defibrillator device.
- Electrolyte imbalance: Correct electrolyte disturbances, especially hypokalemia or hypomagnesemia, prior to use and throughout therapy.
- Hepatic impairment: Use with caution in patients with severe hepatic impairment (has not been studied).
- Renal impairment: Use with caution in patients with renal impairment; systemic clearance of dofetilide is decreased and plasma concentration increased with decreasing CrCl. Dose adjustment is required for patients with CrCl ≤60 mL/minute.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
ECG monitoring with attention to QTc interval (or QT interval if heart rate <60 beats per minute) and occurrence of ventricular arrhythmias, baseline serum creatinine and changes in serum creatinine. Upon initiation (or reinitiation) continuous ECG monitoring recommended for a minimum of 3 days, or for at least 12 hours after electrical or pharmacological conversion to normal sinus rhythm, whichever is greater. Monitor serum potassium and magnesium levels at baseline and throughout therapy. QTc must be monitored at baseline prior to the first dose and 2 to 3 hours afterwards. If at baseline, QTc >440 msec (>500 msec in patients with ventricular conduction abnormalities), use is contraindicated. If dofetilide initiated, QTc interval must be determined 2 to 3 hours after each subsequent dose of dofetilide for in-hospital doses 2 to 5. Thereafter, QTc and CrCl should be evaluated every 3 months. If at any time during therapy after the second dose the measured QTc is >500 msec (>550 msec in patients with ventricular conduction abnormalities), dofetilide should be discontinued.
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Patient Education
What is this drug used for?
- It is used to treat certain types of abnormal heartbeats.
Frequently reported side effects of this drug
- Headache
- Common cold symptoms
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Dizziness
- Passing out
- Fast heartbeat
- Abnormal heartbeat
- Shortness of breath
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.