Boxed Warning
Severe acute exacerbations of hepatitis B:
Severe acute exacerbations of hepatitis B have been reported in patients who have discontinued antihepatitis B therapy, including entecavir. Closely monitor hepatic function with clinical and laboratory follow-up for at least several months in patients who discontinue antihepatitis B therapy. If appropriate, initiation of antihepatitis B therapy may be warranted.
HIV and chronic hepatitis B virus coinfection:
Limited clinical experience suggests there is a potential for the development of resistance to HIV nucleoside reverse transcriptase inhibitors if entecavir is used to treat chronic hepatitis B virus (HBV) infection in patients with HIV infection not being treated. Therapy with entecavir is not recommended for HIV/HBV coinfected patients who are not also receiving antiretroviral therapy.
Lactic acidosis and hepatomegaly:
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogue inhibitors alone or in combination with antiretrovirals.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral:
Baraclude: 0.05 mg/mL (210 mL) [contains methylparaben, propylparaben; orange flavor]
Tablet, Oral:
Baraclude: 0.5 mg, 1 mg
Generic: 0.5 mg, 1 mg
Pharmacology
Mechanism of Action
Entecavir is intracellularly phosphorylated to guanosine triphosphate which competes with natural substrates to effectively inhibit hepatitis B viral polymerase; enzyme inhibition blocks reverse transcriptase activity thereby reducing viral DNA synthesis.
Pharmacokinetics/Pharmacodynamics
Absorption
Delayed with food; Cmax decreased 44% to 46%, AUC decreased 18% to 20%
Distribution
Extensive (Vd in excess of body water)
Metabolism
Minor hepatic glucuronide/sulfate conjugation
Excretion
Urine (60% to 73% as unchanged drug)
Time to Peak
0.5 to 1.5 hours
Half-Life Elimination
Terminal: ~5 to 6 days; accumulation: ~24 hours
Protein Binding
~13%
Use in Specific Populations
Special Populations: Renal Function Impairment
Apparent oral clearance of entecavir decreased as CrCl decreased. Cmax and AUC increased. Hemodialysis removed about 13% of the entecavir dose over 4 hours; continuous ambulatory peritoneal dialysis (CAPD) removed about 0.3% of the dose during 7 days.
Special Populations: Elderly
AUC was 29.3% greater in elderly subjects, most likely because of differences in renal function. Base dose adjustment of entecavir on renal function of patient, not on age.
Use: Labeled Indications
Chronic hepatitis B: Treatment of chronic hepatitis B virus (HBV) infection in adults and pediatric patients ≥2 years of age with evidence of active viral replication and either evidence of persistent transaminase elevations or histologically-active disease.
Note: In adults, indication is based on data in patients with compensated and decompensated liver disease; in children, indication is based on data in patients with compensated, HBeAg-positive liver disease.
Use: Off Label
Hepatitis B virus (HBV) reactivation prophylaxis, immunocompromised patientsbyes
Data from a randomized, controlled trial and observational studies support the use of an effective nucleos(t)ide analog with a high resistance barrier, such as entecavir, for prophylaxis against hepatitis B reactivation in the setting of cytotoxic (eg, anticancer) therapies or immunosuppressive therapies Chen 2013, Huang 2014, Li 2011, Perrillo 2015, Yu 2016, Zhang 2016.
Based on the American Association for the Study of Liver Diseases (AASLD) 2018 guidelines for the prevention, diagnosis, and treatment of chronic hepatitis B, entecavir is an effective and recommended prophylactic agent for prevention of hepatitis B reactivation in anti-HBc-positive and HBsAg-positive individuals receiving anticancer therapy and in anti-HBc-positive, HBsAg-negative individuals undergoing stem cell transplantation or receiving anti-CD20 therapy, such as rituximab.
Hepatitis B virus (HBV) reinfection prophylaxis, post liver transplantbyes
Data from an open-label, prospective study with a median follow-up of 5 years support the long-term use of entecavir for the prophylaxis of HBV reinfection after liver transplantation in recipients with chronic hepatitis B Fung 2017. Another phase IIIb, single-arm, open-label study in patients undergoing orthotopic liver transplantation for chronic hepatitis B infection supports the use of entecavir in this setting Perrillo 2013.
Based on the AASLD guidelines for the prevention, diagnosis, and treatment of chronic hepatitis B, entecavir, with or without hepatitis B immune globulin (HBIG), is effective and recommended for prevention of HBV reinfection in liver transplant recipients posttransplant.
HIV/HBV coinfectionyes
Based on the Department of Health and Human Services (HHS) guidelines for the use of antiretroviral agents in adults and adolescents living with HIV, entecavir (in combination with a fully suppressive antiretroviral regimen) is effective and recommended in the management of HIV/HBV coinfected patients who cannot use a tenofovir-based antiretroviral regimen.
Contraindications
There are no contraindications listed in the manufacturer's US labeling.
Canadian labeling: Hypersensitivity to entecavir or any component of the formulation
Dosage and Administration
Dosing: Adult
Hepatitis B virus (HBV) infection, treatment: Oral:
Nucleoside-treatment naive, compensated liver disease: 0.5 mg once daily.
Decompensated liver disease: 1 mg once daily.
Treatment duration (AASLD practice guidelines): Treatment duration for nucleos(t)ide analog-based therapy (eg, entecavir) is variable and influenced by HBeAg status, duration of HBV suppression, and presence of cirrhosis/decompensation (AASLD [Terrault 2018]).
Patients without cirrhosis:
Hepatitis B e antigen (HBeAg) positive immune-active chronic hepatitis: Treat until HBeAg seroconversion; after seroconversion, prolonged consolidation therapy is often required in patients treated with nucleos(t)ide analogues to prevent hepatitis flares. Optimal duration is unknown; however, consolidation therapy is generally a minimum of 12 months of persistently normal ALT and undetectable serum HBV DNA levels after HBeAg seroconversion.
HBeAg-negative immune-active chronic hepatitis: Indefinite antiviral therapy is suggested unless there is competing rationale for discontinuation (risk/benefit decision); treatment discontinuation may be considered in patients with loss of HBsAg; however, there is insufficient evidence to guide decisions in these patients.
Patients with compensated cirrhosis:
HBeAg-positive immune-active chronic hepatitis: In patients who seroconvert on therapy, continue antiviral therapy indefinitely due to concerns with decompensation and death, unless there is a strong competing rationale for discontinuation.
HBeAg-negative immune-active chronic hepatitis: Treatment discontinuation is not recommended due to potential for decompensation and death (limited data).
Patients with decompensated cirrhosis: Individuals with decompensated cirrhosis should receive indefinite therapy regardless of HBV DNA level, HBeAg status, or ALT level.
Viral breakthrough (AASLD practice guidelines): Patients with confirmed viral breakthrough (HBV DNA ≥100 IU/mL with previously undetectable levels [<10 IU/mL] or >1 log increase in HBV DNA) should either be switched to an alternative antiviral monotherapy agent with a high genetic barrier to resistance or receive a second antiviral agent with a complementary resistance profile; consult current clinical practice guidelines for recommended agents (AASLD [Terrault 2018]).
HBV reactivation prophylaxis, immunocompromised patients (off-label use): Oral: 0.5 mg once daily (AASLD [Terrault 2018]; Chen 2013; Huang 2014; Li 2011; Yu 2016).
HBV reinfection prophylaxis, post liver transplant (with or without HBIG) (off-label use): Oral: 0.5 mg once daily (Fung 2017) or 1 mg once daily (Perrillo 2013).
HIV/HBV coinfection, nucleoside-treatment naive (alternative agent) (off-label use): Oral: 0.5 mg once daily. Note: Only recommended in patients who cannot take tenofovir; must be used in addition to a fully suppressive antiretroviral therapy regimen (HHS [adult 2018]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Oral tablets and solution may be used interchangeably on a mg:mg basis.
Hepatitis B infection (HBV), chronic: Oral: Note: Optimal duration of treatment not established for nucleoside analogs, a minimum of 12 months and typically longer required; consolidation therapy of at least 6 months after seroconversion and complete viral suppression has been suggested (Jonas 2010).
Children and Adolescents 2 to <16 years with compensated liver diseases:
Treatment naive:
10 to 11 kg: 0.15 mg oral solution once daily
>11 to 14 kg: 0.2 mg oral solution once daily
>14 to 17 kg: 0.25 mg oral solution once daily
>17 to 20 kg: 0.3 mg oral solution once daily
>20 to 23 kg: 0.35 mg oral solution once daily
>23 to 26 kg: 0.4 mg oral solution once daily
>26 to 30 kg: 0.45 mg oral solution once daily
>30 kg: 0.5 mg oral solution or tablet once daily
Lamivudine-experienced:
10 to 11 kg: 0.3 mg oral solution once daily
>11 to 14 kg: 0.4 mg oral solution once daily
>14 to 17 kg: 0.5 mg oral solution once daily
>17 to 20 kg: 0.6 mg oral solution once daily
>20 to 23 kg: 0.7 mg oral solution once daily
>23 to 26 kg: 0.8 mg oral solution once daily
>26 to 30 kg: 0.9 mg oral solution once daily
>30 kg: 1 mg oral solution or tablet once daily
Adolescents ≥16 years:
Nucleoside treatment naïve with compensated liver disease: 0.5 mg once daily
Lamivudine-refractory or known lamivudine or telbivudine-resistant mutations: 1 mg once daily
HIV/Hepatitis B virus coinfection: Limited data available: Note: Only recommended in patients who cannot take tenofovir; must be used in addition to a fully suppressive antiretroviral therapy regimen (DHHS [adult/pediatric] 2013): Oral:
Nucleoside treatment naive: Adolescents: 0.5 mg once daily (DHHS [adult] 2013)
Lamivudine-refractory or -resistant with decompensated liver disease:
Children 12 years of age: 0.5 mg once daily (DHHS [pediatric] 2013)
Adolescents: 1 mg once daily (DHHS [adult] 2013)
HBV reinfection prophylaxis, postliver transplant (with or without HBIG): Limited data available: Adolescents ≥16 years: Oral: 1 mg once daily has been reported in an open-label trial of 65 patients (age range: 16 years and older); however, a lower dose of 0.5 mg once daily has also been used in adult patients (age range: 23 to 65 years) (Fung 2011; Perrillo 2012).
Administration
Administer on an empty stomach (2 hours before or after a meal). Do not dilute or mix oral solution with water or other beverages; use calibrated oral dosing syringe. Oral solution and tablet are bioequivalent on a mg-to-mg basis.
Dietary Considerations
Take on an empty stomach (2 hours before or after a meal).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light. After opening, oral solution can be used up to expiration date on the bottle.
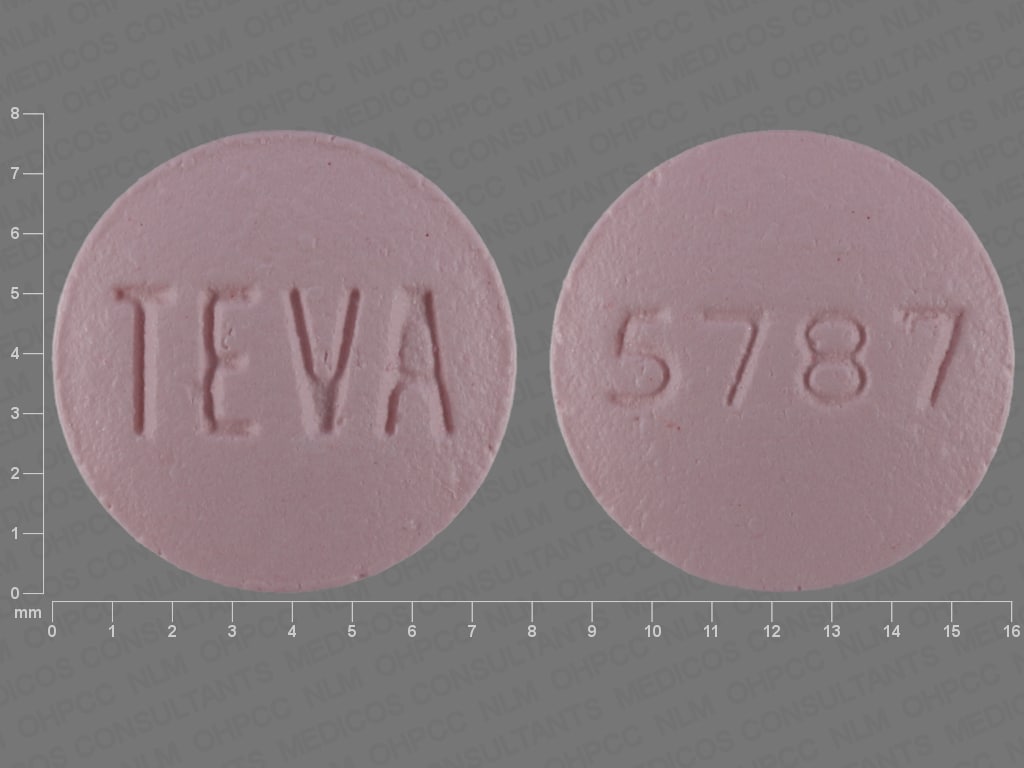
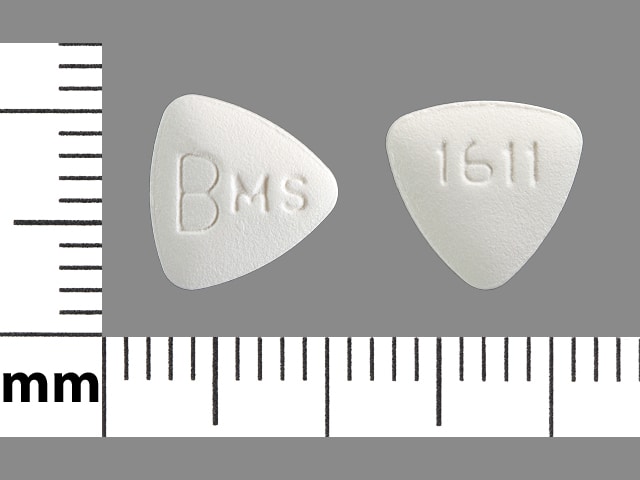
Entecavir Images
Drug Interactions
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
Orlistat: May decrease the serum concentration of Antiretroviral Agents. Monitor therapy
Adverse Reactions
As reported with adult patients, unless otherwise noted.
>10%: Hepatic: Increased serum alanine aminotransferase (>5 x ULN: 11% to 12%; >10 x ULN and >2 x baseline: 2%)
1% to 10%:
Central nervous system: Headache (2% to 4%), fatigue (1% to 3%)
Dermatologic: Skin rash (>1%)
Endocrine & metabolic: Glycosuria (4%), hyperglycemia (2% to 3%)
Gastrointestinal: Increased serum lipase (7%), abdominal pain (children and adolescents: >1%), diarrhea (children and adolescents: >1%; adults: ≤1%), nausea (children and adolescents: >1%; adults: <1%), unpleasant taste (children and adolescents: >1%), vomiting (children and adolescents: >1%; adults: <1%), dyspepsia (≤1%)
Genitourinary: Hematuria (9%)
Hepatic: Increased serum bilirubin (2% to 3%)
Renal: Increased serum creatinine (1% to 2%)
<1%, postmarketing, and/or case reports: Alopecia, anaphylactoid shock, dizziness, drowsiness, hepatomegaly, hepatomegaly with steatosis, hypoalbuminemia, increased serum transaminases, insomnia, lactic acidosis, macular edema (Muqit 2011), thrombocytopenia
Warnings/Precautions
Concerns related to adverse effects:
- Lactic acidosis/hepatomegaly: [US Boxed Warning]: Lactic acidosis and severe hepatomegaly with steatosis (including fatal cases) have been reported with nucleoside analogue inhibitors; use with caution in patients with risk factors for liver disease (risk may be increased with female gender, decompensated liver disease, obesity, or prolonged nucleoside inhibitor exposure) and suspend treatment in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or hepatotoxicity (transaminase elevation may/may not accompany hepatomegaly and steatosis).
Disease-related concerns:
- Chronic hepatitis B: [US Boxed Warning]: Severe, acute exacerbation of hepatitis B may occur upon discontinuation of antihepatitis B therapy, including entecavir. Monitor liver function for at least several months after stopping treatment; reinitiation of antihepatitis B therapy may be required.
- HIV: [US Boxed Warning]: May cause the development of HIV resistance in chronic hepatitis B patients with unrecognized or untreated HIV infection. Determine HIV status prior to initiating treatment with entecavir. Not recommended for HIV/HBV coinfected patients unless also receiving antiretroviral therapy. The manufacturer's labeling states that entecavir does not exhibit any clinically-relevant activity against human immunodeficiency virus (HIV type 1). However, a small number of case reports have indicated declines in virus levels during entecavir therapy. HIV resistance to a common HIV drug has been reported in an HIV/HBV-infected patient receiving entecavir as monotherapy for HBV.
- Hepatic impairment: Dose adjustment not required. Limited data supporting treatment of chronic hepatitis B in patients with decompensated liver disease; observe for increased adverse reactions, including hepatorenal dysfunction.
- Renal impairment: Use with caution in patients with renal impairment or patients receiving concomitant therapy which may reduce renal function; dose adjustment recommended for CrCl <50 mL/minute.
Special populations:
- Children: There are limited data available on the use of entecavir in lamivudine-experienced pediatric patients; use in these patients only if the potential benefit justifies the potential risk to the child.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson, 2002; Lucente 2000; Shelley, 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade, 1986; CDC, 1984). See manufacturer’s labeling.
Other warnings/precautions:
- Resistance: Cross-resistance may develop in patients failing previous therapy with lamivudine.
Monitoring Parameters
Manufacturer’s labeling: HIV status (prior to initiation of therapy); periodic monitoring of hepatic function is recommended during treatment and for at least several months after treatment in patients who discontinue anti-hepatitis B therapy. Monitor patients for signs and symptoms of lactic acidosis and hepatotoxicity.
Alternate recommendations: Chronic Hepatitis B: HBV DNA and ALT (HBV DNA usually done every 3 months until undetectable and then every 3 to 6 months thereafter); HBeAg; anti-HBe (in patients who are HBeAg-positive to monitor for seroconversion); HBsAg; consider monitoring lactic acid levels (if clinical concern); following discontinuation, monitor for recurrent viremia, ALT flares, seroreversion, and clinical decompensation every 3 months for at least 1 year. As antivirals do not eliminate the risk of hepatocellular carcinoma, continued monitoring for this complication is recommended in at-risk patients (AASLD [Terrault 2018]). Renal function at baseline and at least annually; monitor renal function more frequently in patients at high risk of renal dysfunction (WHO 2015).
Pregnancy
Pregnancy Considerations
Teratogenic effects have been observed in animal studies. Information related to use in pregnancy is limited. Other agents may be preferred for the treatment of chronic hepatitis B in pregnancy (AASLD [Terrault 2016]).
Pregnant women taking entecavir should enroll in the pregnancy registry by calling 1-800-258-4263.
Patient Education
What is this drug used for?
- It is used to treat hepatitis B infection.
Frequently reported side effects of this drug
- Headache
- Dizziness
- Nausea
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lactic acidosis like fast breathing, fast heartbeat, abnormal heartbeat, vomiting, fatigue, shortness of breath, severe loss of strength and energy, severe dizziness, feeling cold, or muscle pain or cramps.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.