Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Drisdol: 1.25 MG (50000 UT) [contains brilliant blue fcf (fd&c blue #1), soybean oil, tartrazine (fd&c yellow #5)]
Ergocal: 62.5 MCG (2500 UT) [gluten free; contains fd&c blue #1 aluminum lake, fd&c yellow #10 (quinoline yellow), gelatin (bovine), soybean lecithin]
Generic: 1.25 MG (50000 UT)
Solution, Oral:
Calcidol: 200 mcg/mL (60 mL) [contains propylene glycol]
Calciferol: 200 mcg/mL (60 mL) [contains propylene glycol]
Drisdol: 200 mcg/mL (60 mL [DSC]) [contains propylene glycol]
Generic: 200 mcg/mL (60 mL)
Tablet, Oral:
Generic: 10 MCG (400 UNIT), 50 MCG (2000 UT)
Pharmacology
Mechanism of Action
Ergocalciferol (vitamin D2) is a provitamin. The active metabolite, 1,25-dihydroxyvitamin D (calcitriol), stimulates calcium and phosphate absorption from the small intestine, promotes secretion of calcium from bone to blood; promotes renal tubule phosphate resorption.
Pharmacokinetics/Pharmacodynamics
Absorption
Absorbed in the small intestine; fat soluble; requires bile (IOM 2011)
Metabolism
Inactive until hydroxylated hepatically to 25-hydroxyvitamin D [25(OH)D; calcifediol] then renally to the active metabolite 1,25-dihydroxyvitamin D (calcitriol)
Excretion
Feces (IOM 2011)
Onset of Action
10 to 24 hours; Maximum effect: ~1 month following daily doses
Half-Life Elimination
Circulating: 25(OH)D: 2 to 3 weeks; 1,25-dihydroxyvitamin D ~4 hours
Use: Labeled Indications
Dietary supplement: For use as a vitamin D supplement.
Hypoparathyroidism: Treatment of hypoparathyroidism. Note: Since parathyroid hormone (PTH) is required for the conversion of vitamin D (ergocalciferol or cholecalciferol) to the active metabolite of vitamin D (1,25-dihydroxyvitamin D), alternative vitamin D preparations not dependent on this conversion (eg, alfacalcidol, calcitriol) are recommended for routine use (Endocrine Society [Brandi 2016]).
Use: Off Label
Osteoporosis, preventionyes
Based on the Clinician's Guide to Prevention and Treatment of Osteoporosis from the National Osteoporosis Foundation (NOF), adequate intake of vitamin D (through dietary sources and/or supplementation with ergocalciferol [or cholecalciferol] if needed) is effective and recommended for the prevention of osteoporosis.
Vitamin D insufficiency/deficiencyyes
Based on the National Osteoporosis Foundation (NOF) Clinician's Guide to Prevention and Treatment of Osteoporosis, supplemental cholecalciferol (or ergocalciferol) may be used for the prevention or treatment of vitamin D deficiency to achieve desired serum 25(OH)D levels.
Vitamin D insufficiency/deficiency in patients with chronic kidney disease, treatmentyes
Based on the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD), vitamin D insufficiency/deficiency in patients without severe and progressive hyperparathyroidism, including chronic kidney disease stages G3 to G5 and dialysis or transplant patients, should be corrected using treatment strategies recommended for the general population, which includes repletion with ergocalciferol (or cholecalciferol) KDIGO 2009, KDIGO 2017. In patients in whom serum parathyroid hormone levels are progressively rising and remain persistently elevated despite correction of modifiable factors, calcitriol or vitamin D analogs are suggested instead of ergocalciferol (or cholecalciferol) KDOQI commentary [Uhlig 2010].
Contraindications
Hypercalcemia; malabsorption syndrome; abnormal sensitivity to the toxic effects of vitamin D; hypervitaminosis D
Note: Although the manufacturer's labeling lists use in malabsorption syndrome as contraindicated, when dosed appropriately, ergocalciferol may be used in these patients (AACE/ACE [Camacho 2016]; Dawson-Hughes 2018).
Documentation of allergenic cross-reactivity for vitamin D analogues is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: 1 mcg = 40 units
Osteoporosis, prevention (off-label use): Oral: Adults ≥50 years of age: 800 to 1,000 units/day is recommended, through dietary sources and/or supplementation if needed (NOF [Cosman 2014]).
Vitamin D insufficiency/deficiency treatment (off-label use): Note: Repletion strategies may vary depending on desired target serum 25(OH)D levels as well as the clinical status of the patient. The optimal serum 25(OH)D level is controversial; the Institute of Medicine recommends a 25(OH)D level >20 ng/mL as sufficient in nearly all persons (IOM 2011), whereas others have suggested targeting a level of ~30 ng/mL to minimize the risk of fractures, particularly in patients with osteoporosis (AACE/ACE [Camacho 2016]; NOF [Cosman 2014]). However, some data suggest levels >40 ng/mL (median level in one trial: ~48 ng/mL) are associated with increased risk of falls in postmenopausal women (Sanders 2010; Smith 2017).
Therefore, some experts recommend a range of 20 to 40 ng/mL as a reasonable target in most patients (Dawson-Hughes 2018). Ergocalciferol (vitamin D2) is considered an alternative agent to the use of cholecalciferol (vitamin D3) by some experts due to limited data showing slightly higher levels of serum 25(OH)D achieved with D3, especially when higher doses or longer intervals are used (Dawson-Hughes 2018; Tripkovic 2012). In patients with normal absorption, for every 100 units/day of vitamin D ingested the serum 25(OH)D level is expected to increase by ~0.7 to 1 ng/mL (ASPEN [McKeever 2017]; Dawson-Hughes 2018). The dose-response declines as the 25(OH)D concentration increases above 40 ng/mL (100 nmol/L) (Dawson-Hughes 2018). The following recommendations are based primarily on expert opinion and clinical experience:
Initial dosing (according to baseline serum 25(OH)D level):
Serum 25(OH)D 20 to 30 ng/mL: Initial: Supplementation dosing: Oral: 600 to 800 units once daily; a repeat serum 25(OH)D level is not required (Dawson-Hughes 2018) or 1,000 to 2,000 units once daily; may consider a repeat serum 25(OH)D level in ~3 months to determine if the target level has been achieved (Khan 2010).
Serum 25(OH)D 10 to <20 ng/mL: Initial:
Supplementation dosing: Oral: 800 to 1,000 units once daily (Dawson-Hughes 2018) or 2,000 units once daily (Khan 2010); a repeat serum 25(OH)D level should be drawn after ~3 months. If target serum 25(OH)D level has not been achieved, may increase to 2,000 units once daily or administer therapeutic dosing of 50,000 units once weekly for 6 to 8 weeks (Dawson-Hughes 2018).
OR
Therapeutic dosing (ie, high-dose ergocalciferol): Oral: 50,000 units once weekly (or 5,000 to 7,000 units once daily) for ~8 weeks followed by decreased maintenance dosing as needed to maintain target serum 25(OH)D level (AACE/ACE [Camacho 2016]; NOF [Cosman 2014]).
Serum 25(OH)D <10 ng/mL or in patients with deficiency symptoms: Initial: Therapeutic dosing (ie, high-dose ergocalciferol): Oral: 50,000 units once weekly (or 5,000 to 7,000 units once daily) for 6 to 8 weeks to achieve target serum 25(OH)D level; a repeat serum 25(OH)D level should be drawn after ~3 months to assure target serum 25(OH)D level has been met (AACE/ACE [Camacho 2016]; Dawson-Hughes 2018; NOF [Cosman 2014]).
Maintenance dosing: Maintenance dosing is highly patient specific and dependent on target 25(OH)D level and may range from 600 to 800 units/day (Dawson-Hughes 2018) to 1,000 to 2,000 units/day (AACE/ACE [Camacho 2016]); NOF [Cosman 2014]).
Special populations (eg, obese patients, patients on medications known to affect vitamin D metabolism, patients with malabsorption syndromes or gastrectomy): Higher doses or longer durations may be necessary for adequate repletion (AACE/ACE [Camacho 2016]; Dawson-Hughes 2018).
Vitamin D deficiency/insufficiency in patients with chronic kidney disease (off-label use): Oral:
Note: In patients without severe and progressive hyperparathyroidism, including chronic kidney disease (CKD) stages G3 to G5 and dialysis or transplant patients, KDIGO guidelines recommend correcting vitamin D deficiency and insufficiency with treatment strategies recommended for the general population using ergocalciferol (or cholecalciferol) while avoiding hypercalcemia and ensuring phosphate levels are in the normal range. An individualized monitoring approach to direct treatment is also recommended (KDIGO 2009; KDIGO 2017). In patients in whom serum parathyroid hormone levels are progressively rising and remain persistently elevated despite correction of modifiable factors (eg, hyperphosphatemia, vitamin D deficiency), calcitriol or vitamin D analogs are suggested instead of ergocalciferol (or cholecalciferol) (KDOQI commentary [Uhlig 2010]).
Hypoparathyroidism: Note: Active vitamin D preparations (ie, alfacalcidol, calcitriol) in conjunction with calcium supplementation are recommended therapy. Addition of ergocalciferol (or cholecalciferol) may be considered for supplemental therapy (Endocrine Society [Brandi 2016]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: 1 mcg = 40 USP units
Hypoparathyroidism: Oral: Infants, Children, and Adolescents: 50,000 to 200,000 units daily with calcium supplements
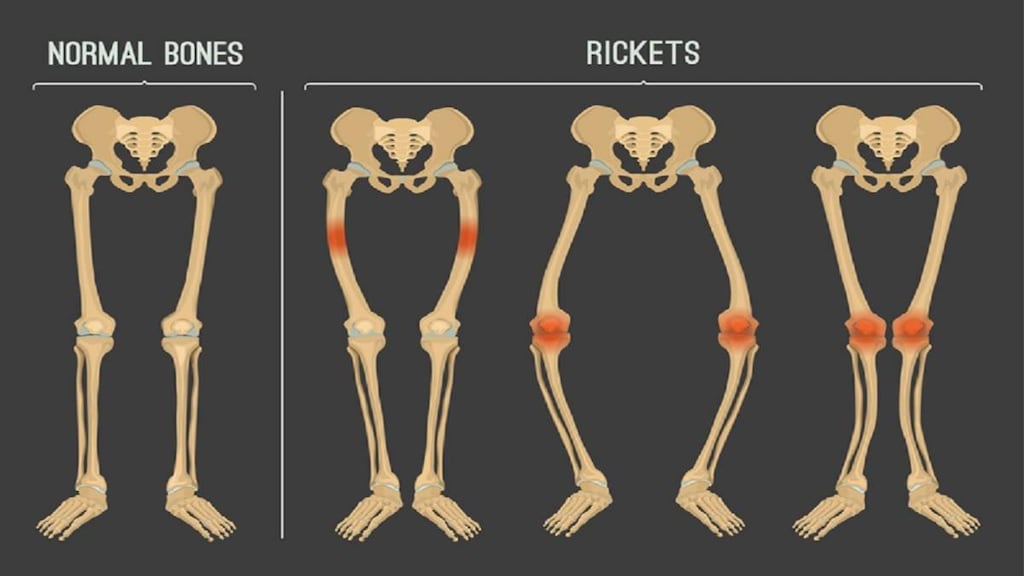
Vitamin D deficiency, prevention (eg, Rickets prevention) (AAP [Folsom 2017]; AAP [Wagner 2008]; Munns 2016): Oral:
Breast-fed infants (fully or partially): Oral: 400 units/day beginning in the first few days of life. Continue supplementation until infant is weaned to ≥1,000 mL/day or 1 qt/day of vitamin D-fortified formula or whole milk (after 12 months of age)
Formula-fed infants ingesting <1,000 mL of vitamin D-fortified formula or milk: Oral: 400 units/day
Children and Adolescents without adequate intake: Oral: 400 to 600 units/day. Note: Children with increased risk of vitamin D deficiency (chronic fat malabsorption, maintained on chronic antiseizure medications) may require higher doses. Use laboratory testing [25(OH)D, PTH, bone mineral status] to evaluate.
Vitamin D deficiency, treatment: Note: Treatment should also include calcium and phosphorus supplementation; some patients with chronic fat malabsorption, obesity, or who are maintained on chronic antiseizure medications, glucocorticoids, HIV medications, or antifungals may require higher doses of ergocalciferol (AAP [Golden 2014]); monitor vitamin D status closely:
Infants: Oral: 2,000 units daily for 6 weeks to achieve a serum 25(OH)D level >20 ng/mL; followed by a maintenance dose of 400 to 1,000 units daily. Note: For patients at high risk of fractures a serum 25(OH)D level >30 ng/mL has been suggested (AAP [Golden 2014])
Children and Adolescents: Oral: 2,000 units daily for 6 to 8 weeks to achieve a serum 25(OH)D level >20 ng/mL; followed by a maintenance dose of 600 to 1,000 units daily. Note: For patients at high risk of fractures a serum 25(OH)D level >30 ng/mL has been suggested (AAP [Golden 2014])
Vitamin D insufficiency or deficiency associated with CKD (stages 2 to 5, 5D); serum 25 hydroxyvitamin D (25[OH]D) level <30 ng/mL: (K/DOQI Guidelines 2009): Oral:
Serum 25(OH)D level 16 to 30 ng/mL: Infants, Children, and Adolescents: 2,000 units/day for 3 months or 50,000 units every month for 3 months
Serum 25(OH)D level 5 to 15 ng/mL: Infants, Children, and Adolescents: 4,000 units/day for 12 weeks or 50,000 units every other week for 12 weeks
Serum 25(OH)D level <5 ng/mL: Infants, Children, and Adolescents: 8,000 units/day for 4 weeks then 4,000 units/day for 2 months for total therapy of 3 months or 50,000 units/week for 4 weeks followed by 50,000 units 2 times monthly for a total therapy of 3 months
Maintenance dose [once repletion accomplished; serum 25(OH)D level >30 ng/mL]: Infants, Children, and Adolescents: 200 to 1,000 units/day
Rickets:
Nutritional rickets, treatment: Limited data available (Munns 2016): Administer in combination with calcium supplementation:
Daily therapy (preferred):
Infants: Oral: 2,000 units daily for ≥3 months, followed by maintenance dose of 400 units daily
Children: Oral: 3,000 to 6,000 units daily for ≥3 months, followed by maintenance dose of 600 units daily
Adolescents: Oral: 6,000 units daily for ≥3 months, followed by maintenance dose of 600 units daily
Single-dose therapy: Note: While ergocalciferol can be used, cholecalciferol is the preferred supplement for single-dose therapy due to longer half-life
Infants ≥3 months: Oral: 50,000 units once, or in divided doses over several days; after 3 months, initiate maintenance dose of 400 units daily
Children: Oral: 150,000 units once, or in divided doses over several days; after 3 months, initiate maintenance dose of 600 units daily
Adolescents: Oral: 300,000 units once, or in divided doses over several days; after 3 months, initiate maintenance dose of 600 units daily
Dietary Considerations
Vitamin D is found in egg yolks, fatty fish, fortified milk, fortified cereal, and infant formulas; it is also produced by exposure to sunlight (IOM 2011).
Dietary Reference Intake for Vitamin D (IOM 2011):
Infants 0 to 12 months: Adequate intake: 10 mcg/day (400 units/day)
1 to 70 years: RDA: 15 mcg/day (600 units/day)
>70 years: RDA: 20 mcg/day (800 units/day)
Pregnancy/Lactating: RDA: 15 mcg/day (600 units/day)
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from light.
Ergocalciferol Images
Drug Interactions
Aluminum Hydroxide: Vitamin D Analogs may increase the serum concentration of Aluminum Hydroxide. Specifically, the absorption of aluminum may be increased, leading to increased serum aluminum concentrations. Avoid combination
Bile Acid Sequestrants: May decrease the serum concentration of Vitamin D Analogs. More specifically, bile acid sequestrants may impair absorption of Vitamin D Analogs. Management: Avoid concomitant administration of vitamin D analogs and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the potential risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Calcium Salts: May enhance the adverse/toxic effect of Vitamin D Analogs. Monitor therapy
Cardiac Glycosides: Vitamin D Analogs may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Danazol: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Erdafitinib: Serum Phosphate Level-Altering Agents may diminish the therapeutic effect of Erdafitinib. Management: Avoid coadministration of serum phosphate level-altering agents with erdafitinib before initial dose increase period based on serum phosphate levels (Days 14 to 21). Consider therapy modification
Mineral Oil: May decrease the serum concentration of Vitamin D Analogs. More specifically, mineral oil may interfere with the absorption of Vitamin D Analogs. Management: Avoid concomitant, oral administration of mineral oil and vitamin D analogs. Consider separating the administration of these agents by several hours to minimize the risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Orlistat: May decrease the serum concentration of Vitamin D Analogs. More specifically, orlistat may impair absorption of Vitamin D Analogs. Management: Monitor clinical response (including serum calcium) to oral vitamin D analogs closely if used with orlistat. If this combination must be used, consider giving the vitamin D analog at least 2 hrs before or after orlistat. Consider therapy modification
Sucralfate: Vitamin D Analogs may increase the serum concentration of Sucralfate. Specifically, the absorption of aluminum from sucralfate may be increased, leading to an increase in the serum aluminum concentration. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Vitamin D Analogs: May enhance the adverse/toxic effect of other Vitamin D Analogs. Avoid combination
Adverse Reactions
Frequency not defined: Endocrine & metabolic: Hypervitaminosis D
Warnings/Precautions
Concerns related to adverse effects:
- Vitamin D toxicity: May occur with excessive doses; symptoms may include nausea, vomiting, loss of appetite, constipation, dehydration, fatigue, irritability, confusion, weakness, and/or weight loss. Effects of vitamin D can last ≥2 months after therapy is discontinued.
Disease-related concerns:
- Hyperphosphatemia: Normal serum phosphorous concentrations must be maintained in patients treated for hyperphosphatemia to prevent metastatic calcification.
- Obesity: Adults with a BMI >30 kg/m2 are at high risk for vitamin D deficiency due to storage of vitamin D in adipose tissue. Doses higher than the RDA may be required, but must be carefully monitored to avoid toxicity.
- Renal impairment: Metabolism of vitamin D may be altered in patients with chronic kidney disease. Supplementation with ergocalciferol may be needed; close monitoring is required (KDIGO 2009).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Propylene glycol: Oral solutions may contain propylene glycol; toxicities may occur if large doses of vitamin D are required. Alternate dosage forms/products should be used (Misra 2008).
- Tartrazine: Products may contain tartrazine, which may cause allergic reactions in certain individuals.
Monitoring Parameters
Signs/symptoms of vitamin D toxicity (eg, hypercalcemia, hypercalciuria, confusion, psychosis, tremor, calcification of soft tissue, nausea, weakness) (ASPEN [McKeever 2017])
Adults:
Serum 25(OH)D: For patients being treated for vitamin D deficiency, measure ~3 months after initiation or dosage adjustment. In healthy patients initiating supplementation dosing, routine monitoring is not required (Dawson-Hughes 2018).
Additional monitoring of calcium, phosphorous, parathyroid hormone (PTH), and alkaline phosphatase may be required depending on severity of 25(OH)D deficiency and/or concomitant clinical condition (eg, chronic kidney disorder [CKD], hypoparathyroidism) (Dawson-Hughes 2018; Endocrine Society [Brandi 2016]; KDIGO 2017).
Infants, Children, and Adolescents:
Vitamin D deficiency: Serum calcium, phosphorus, and alkaline phosphatase (ALP) one month after starting therapy; serum calcium, phosphorous, magnesium, ALP, 25(OH)D, and PTH as well as x-ray (may also consider urine calcium/creatinine ratio) after 3 months; 25(OH)D yearly (Misra 2008).
Increased risk of vitamin D deficiency (eg, chronic fat malabsorption, chronic antiseizure medication use): Serum 25(OH)D, PTH, and bone mineral status (baseline); if vitamin D supplement is required, repeat 25(OH)D levels at 3-month intervals until normal. PTH and bone mineral status should be monitored every 6 months until normal (Wagner 2008).
CKD: Measure serum 25(OH)D levels after 3 months of treatment. Measure corrected total calcium and phosphorous after 1 month and then at least every 3 months (KDOQI 2009).
Pregnancy
Pregnancy Considerations
The ergocalciferol (vitamin D2) metabolite, 25(OH)D, crosses the placenta; maternal serum concentrations correlate with fetal concentrations at birth (Misra 2008; Wagner 2008).
Vitamin D deficiency in a pregnant woman may lead to a vitamin D deficiency in the neonate (Misra 2008; Wagner 2008). Serum 25(OH)D concentrations should be measured in pregnant women considered to be at increased risk of deficiency (ACOG 2011). The amount of vitamin D contained in prenatal vitamins may not be adequate to treat a deficiency during pregnancy; although larger doses may be needed, current guidelines recommend a total of 1000 to 2000 units/day until more safety data is available (ACOG 2011). In women not at risk for deficiency, doses larger than the RDA should be avoided during pregnancy (ACOG 2011).
Maternal vitamin D requirements are the same for breastfeeding and nonbreastfeeding females (IOM 2011). The maternal dose of vitamin D needed to provide the infant with an adequate amount of vitamin D is still under study (Wagner 2008)
Patient Education
What is this drug used for?
- It is used to treat poor parathyroid function.
- It is used to treat or prevent low phosphate levels.
- It is used to treat rickets.
- It may be given to you for other reasons. Talk with the doctor.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.