Boxed Warning
Monitoring:
Use with extreme caution in patients with renal impairment. Close monitoring of hematologic, renal, and hepatic status of all patients is essential.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Ancobon: 250 mg, 500 mg
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Penetrates fungal cells and is converted to fluorouracil which competes with uracil interfering with fungal RNA and protein synthesis
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid; serum concentrations are highly variable in neonates; monitor closely (Pasqualotto, 2007); serum concentrations tended to be higher in children <12 years of age; monitor closely (Soltani, 2006)
Distribution
Into CSF, aqueous humor, joints, peritoneal fluid; Vd: 0.6 L/kg
Metabolism
Minimally hepatic; deaminated both in yeasts and possibly via gut bacteria to 5-fluorouracil
Excretion
Urine (>90% as unchanged drug)
Time to Peak
Serum: Neonates: 2.5 ± 1.3 hours; Adults: ~1 to 2 hours
Half-Life Elimination
Neonates: 4 to 34 hours (Baley, 1990); Infants: 7.4 hours; Adults: 2 to 5 hours; Anuria: 85 hours (range: 30 to 250); End-stage renal disease (ESRD): 75 to 200 hours
Protein Binding
3% to 4%
Use in Specific Populations
Special Populations: Renal Function Impairment
Prolonged half-life (29.9 to 250 hours in anuric or nephrectomized patients).
Use: Labeled Indications
Candida/Cryptococcus infections: Adjunctive treatment of systemic fungal infections (eg, septicemia, endocarditis, UTI, meningitis, or pulmonary) caused by susceptible strains of Candida or Cryptococcus
Contraindications
Hypersensitivity to flucytosine or any component of the formulation
Dosage and Administration
Dosing: Adult
Usual dosage ranges: Oral: 50 to 150 mg/kg/day in divided doses every 6 hours
Candidiasis (off-label dose) (IDSA [Pappas 2016]): Oral:
Central nervous system (eg, meningitis): 25 mg/kg/dose 4 times daily (with amphotericin B [liposomal]) until step-down therapy is clinically appropriate.
Cystitis, symptomatic: Fluconazole-resistant C. glabrata: 25 mg/kg/dose 4 times daily for 7 to 10 days as monotherapy.
Endocarditis (native or prosthetic valve) or infected implantable cardiac devices (eg, pacemaker, ICD, VAD): 25 mg/kg/dose 4 times daily (with an amphotericin B lipid formulation); for native or prosthetic valve endocarditis, therapy should continue for at least 6 weeks after valve replacement surgery (longer durations in patients with abscesses or other complications); for patients with implantable cardiac devices, therapy should continue for 4 to 6 weeks after surgery (4 weeks for infections limited to generator pockets and at least 6 weeks for infections involving the wires). Note: May transition to fluconazole if patient clinically stable with fluconazole-susceptible isolates in whom Candida has cleared from the bloodstream.
Endophthalmitis (with or without vitritis): Fluconazole- or voriconazole-resistant isolates: 25 mg/kg/dose 4 times daily (with amphotericin B [liposomal]) for at least 4 to 6 weeks until examination indicates resolution; for patients with vitritis or with macular involvement (with or without vitritis), an intravitreal injection with voriconazole or amphotericin B deoxycholate is also recommended.
Pyelonephritis, symptomatic: Fluconazole-resistant C. glabrata: 25 mg/kg/dose 4 times daily in combination with amphotericin B deoxycholate for 1 to 7 days or as monotherapy for 14 days.
Cryptococcal meningitis, treatment: Oral:
Non-HIV-infected, non-transplant: Induction: 25 mg/kg/dose (with amphotericin B) every 6 hours for at least 4 weeks; if clinical and microbiological improvement, may discontinue both amphotericin and flucytosine and follow with an extended course of fluconazole (IDSA [Perfect 2010]).
HIV-infected or solid organ transplant recipients: Induction: 25 mg/kg/dose (with amphotericin B) every 6 hours for at least 2 weeks; if clinical and microbiological improvement, may discontinue both amphotericin and flucytosine and follow with an extended course of fluconazole (HHS [OI adult 2019]; IDSA [Perfect 2010]).
Cerebral cryptococcomas: Induction: 25 mg/kg/dose (with amphotericin B and corticosteroids) every 6 hours for at least 6 weeks, followed with an extended course of fluconazole (IDSA [Perfect 2010])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: In general, administer in combination with amphotericin B or another susceptible antifungal due to development of resistance.
General dosing, susceptible infections: Infants, Children, and Adolescents: Oral: 50 to 150 mg/kg/day in divided doses every 6 hours (Red Book [AAP 2015])
Aspergillosis, endocarditis: Limited data available: Children and Adolescents: Oral: 37.5 mg/kg/dose every 6 hours in combination with amphotericin B (AHA [Baltimore 2015])
Candidiasis:
Chorioretinitis: Infants, Children, and Adolescents: Oral: 25 mg/kg/dose every 6 hours in combination with amphotericin B (IDSA [Pappas 2016])
CNS disease, treatment: Infants, Children, and Adolescents: Oral: 25 mg/kg/dose every 6 hours in combination with amphotericin B (IDSA [Pappas 2016])
Endocarditis or implanted cardiovascular device:
Infants: Oral: 25 mg/kg/dose every 6 hours in combination with amphotericin B; valve replacement or removal of hardware is strongly recommended (IDSA [Pappas 2016])
Children and Adolescents: Oral: 25 to 37.5 mg/kg/dose every 6 hours in combination with amphotericin B; valve replacement or removal of hardware is strongly recommended (AHA [Baltimore 2015]; IDSA [Pappas 2016])
Urinary tract infection: Infants, Children, and Adolescents: Oral:
Cystitis, symptomatic: 25 mg/kg/dose every 6 hours for 7 to 10 days (IDSA [Pappas 2016])
Pyelonephritis: 25 mg/kg/dose every 6 hours for 2 weeks with or without amphotericin B (IDSA [Pappas 2016]); if fungal balls present, use in combination with amphotericin B and treatment duration should be until symptom resolution and clear urine culture
Cryptococcal disease; disseminated (including CNS disease); treatment (independent of HIV status): Infants, Children, and Adolescents: Oral: 25 mg/kg/dose every 6 hours in combination with amphotericin B or fluconazole; minimum treatment duration: ≥2 weeks; full treatment duration dependent upon: HIV status, source of infection and concomitant antifungal therapy (HHS [OI pediatric 2013]; HHS [OI Adult 2015]; Perfect 2010; Tunkel 2008)
Extemporaneously Prepared
50 mg/mL Oral Suspension (ASHP standard concentration) (ASHP 2017)
A 50 mg/mL oral suspension may be made with capsules and OraPlus and OraSweet SF. Mix 30 mL of OraPlus and 30 mL of OraSweet SF together in a separate container. Empty the contents of six 500 mg capsules in a mortar; add 15 mL portion of the vehicle mixture and triturate. Transfer mixture to a 60 mL (2 ounce) amber prescription bottle. Rinse the mortar with an additional 15 mL of vehicle mixture and pour into the amber bottle. Repeat rinsing procedure until a final bottle volume of 60 mL is achieved. Label the bottle "shake well." Stable for 90 days at 3°C to 5°C (37°F to 41°F) or 23°C to 25°C (73°F to 77°F).
VandenBussche HL, Johnson CE, Yun J, et al. Stability of flucytosine 50 mg/mL in extemporaneous oral liquid formulations. Am J Health Syst Pharm. 2002;93(19):1853-1855.12374070
10 mg/mL Oral Suspension
A 10 mg/mL oral suspension may be made with capsules and distilled water. Empty the contents of ten 500 mg capsules in a mortar; add small portions of distilled water and mix to a uniform paste. Mix while adding distilled water in incremental proportions to almost 500 mL; transfer to a 500 mL volumetric flask, rinse mortar several times with distilled water, and add sufficient quantity of distilled water to make 500 mL. Store in glass or plastic prescription bottles and label "shake well". Stable for 70 days refrigerated and 14 days at room temperature.
Wintermeyer SM and Nahata MC. Stability of Flucytosine in an Extemporaneously Compounded Oral Liquid. Am J Health Syst Pharm. 1996;53(4):407-409.8673661
Administration
Administer around-the-clock to promote less variation in peak and trough serum levels. To reduce or avoid nausea and vomiting, administer a few capsules at a time over 15 minutes until full dose is taken.
Storage
Store at room temperature of 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
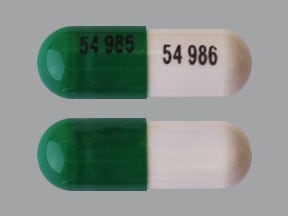
Flucytosine Images
Drug Interactions
Amphotericin B: May enhance the adverse/toxic effect of Flucytosine. This may be related to the adverse effects of amphotericin B on renal function. Monitor therapy
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Cytarabine (Conventional): May diminish the therapeutic effect of Flucytosine. Consider therapy modification
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Gimeracil: May increase serum concentrations of the active metabolite(s) of Flucytosine. Specifically, gimeracil may increase concentrations of fluorouracil. Avoid combination
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Saccharomyces boulardii: Antifungal Agents (Systemic, Oral) may diminish the therapeutic effect of Saccharomyces boulardii. Avoid combination
Test Interactions
Flucytosine causes markedly false elevations in serum creatinine values when the Ektachem® analyzer is used. The Jaffé reaction is recommended for determining serum creatinine.
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiotoxicity, chest pain, ventricular dysfunction
Central nervous system: Ataxia, confusion, fatigue, hallucination, headache, paresthesia, parkinsonian-like syndrome, peripheral neuropathy, psychosis, sedation, seizure, vertigo
Dermatologic: Pruritus, skin photosensitivity, skin rash, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Hypoglycemia, hypokalemia
Gastrointestinal: Abdominal pain, anorexia, diarrhea, duodenal ulcer, enterocolitis, gastrointestinal hemorrhage, nausea, ulcerative colitis, vomiting, xerostomia
Genitourinary: Azotemia, crystalluria
Hematologic & oncologic: Agranulocytosis, anemia, aplastic anemia, bone marrow aplasia, eosinophilia, leukopenia, pancytopenia, thrombocytopenia
Hepatic: Hepatic injury (acute), hepatic insufficiency, hepatic necrosis, increased liver enzymes, increased serum bilirubin, jaundice
Hypersensitivity: Hypersensitivity reaction
Neuromuscular & skeletal: Weakness
Otic: Hearing loss
Renal: Increased blood urea nitrogen, increased serum creatinine, renal failure
Respiratory: Dyspnea
Miscellaneous: Fever
Warnings/Precautions
Disease-related concerns:
- Hematologic disease: Use with caution in patients with bone marrow depression, hematologic disease or who have been treated with radiation or drugs that suppress the bone marrow; bone marrow toxicity may be irreversible.
- Hepatic impairment: Use with caution in patients with hepatic impairment; hepatotoxicity may occur.
- Renal impairment: [US Boxed Warning]: Use with extreme caution in patients with renal dysfunction; dosage adjustment required.
Other warnings/precautions:
- Monitoring: [US Boxed Warning]: Closely monitor hematologic, renal, and hepatic status. Hepatotoxicity and bone marrow toxicity appear to be dose related; monitor levels closely and adjust dose accordingly.
- Monotherapy: Avoid use as monotherapy; resistance rapidly develops.
Monitoring Parameters
Pretreatment: Electrolytes (especially potassium), CBC with differential, BUN, renal function, blood culture
During treatment: CBC with differential and LFTs (eg, alkaline phosphatase, AST/ALT) frequently; renal function; serum flucytosine concentrations (2 hours after administration of a dose) after ~3 days of treatment and as clinically indicated (eg, following dosage adjustment, change in renal function, bone marrow toxicity) (BSMM [Ashbee 2014]).
Pregnancy
Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies. Flucytosine is metabolized to fluorouracil which may cause adverse events if administered during pregnancy; refer to the Fluorouracil (Systemic) monograph for additional information.
Patient Education
What is this drug used for?
- It is used to treat fungal infections.
Frequently reported side effects of this drug
- Fatigue
- Dry mouth
- Abdominal pain
- Nausea
- Headache
- Vomiting
- Diarrhea
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Kidney problems like unable to pass urine, blood in urine, change in amount of urine passed, or weight gain.
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any bleeding that is very bad or that will not stop.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, a fast heartbeat, confusion, hunger, or sweating.
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, severe abdominal pain, light-colored stools, vomiting, or yellow skin or eyes.
- Confusion
- Severe loss of strength and energy
- Swelling of arms or legs
- Tremors
- Trouble moving
- Stiff muscles
- Chest pain
- Seizures
- Mood changes
- Hearing loss
- Change in balance
- Burning or numbness feeling
- Excessive weight gain
- Shortness of breath
- Sensing things that seem real but are not
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.