Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Iressa: 250 mg
Pharmacology
Mechanism of Action
Gefitinib is a tyrosine kinase inhibitor (TKI) which reversibly inhibits kinase activity of wild-type and select activation mutations of epidermal growth factor receptor (EGFR). EGFR is expressed on cell surfaces of normal and cancer cells and has a role in cell growth and proliferation. Gefitinib prevents autophosphorylation of tyrosine residues associated with the EGFR receptor, which blocks downstream signaling and EGFR-dependent proliferation. Gefitinib has a higher binding affinity for EGFR exon 19 deletion and exon 21 (L858R) substitution mutation than for wild-type EGFR.
Pharmacokinetics/Pharmacodynamics
Distribution
1400 L
Metabolism
Hepatic (extensive), primarily via CYP3A4, as well as CYP2D6; forms metabolites
Excretion
Feces (86%); urine (<4%)
Time to Peak
Plasma: Oral: 3 to 7 hours
Half-Life Elimination
Oral: 48 hours
Protein Binding
90%, albumin and alpha1-acid glycoprotein
Use in Specific Populations
Special Populations: Hepatic Function Impairment
When comparing patients with hepatic impairment due to cirrhosis to healthy patients, gefitinib systemic exposure was increased 40% in mild impairment, 263% in moderate impairment, and 166% in severe impairment; however, in a study of patients with liver metastases, patients with metastases and moderate impairment had similar systemic exposure as patients with metastases and normal hepatic function.
Use: Labeled Indications
Non-small cell lung cancer: First-line treatment of metastatic non-small cell lung cancer (NSCLC) in tumors with epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations as detected in tumor or plasma specimen by an approved test.
Limitation of use: Safety and efficacy have not been established in patients with metastatic NSCLC whose tumors have EGFR mutations other than exon 19 deletions or exon 21 (L858R) substitution mutations
Contraindications
There are no contraindications listed in the manufacturer’s US labeling.
Canadian labeling: Hypersensitivity to gefitinib or any component of the formulation.
Dosage and Administration
Dosing: Adult
Non-small cell lung cancer (NSCLC), metastatic, with EGFR exon 19 deletions or exon 21 (L858R) substitution mutations: Oral: 250 mg once daily until disease progression or unacceptable toxicity.
Missed doses: Do not take a missed dose if it is within 12 hours of the next scheduled dose.
Dosage adjustment for concomitant therapy: Strong CYP3A4 inducers: Increase gefitinib to 500 mg once daily (in the absence of severe adverse drug reactions); reduce gefitinib dose back to 250 mg once daily 7 days after discontinuing the strong CYP3A4 inducer.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Dermatologic toxicity:
Skin reactions (grade 3 or higher): Withhold treatment for up to 14 days; may resume treatment when fully resolved or improved to grade 1.
Severe bullous, blistering or exfoliating dermatologic conditions: Interrupt or discontinue treatment.
Gastrointestinal toxicity:
Diarrhea (grade 3 or higher): Withhold treatment for up to 14 days; may resume treatment when fully resolved or improved to grade 1.
Gastrointestinal perforation: Permanently discontinue.
Ocular toxicity:
Signs/symptoms of severe or worsening disorders, including keratitis: Withhold treatment for up to 14 days; may resume treatment when fully resolved or improved to grade 1.
Persistent ulcerative keratitis: Permanently discontinue.
Pulmonary toxicity:
Acute onset or worsening symptoms (dyspnea, cough, fever): Withhold treatment for up to 14 days; may resume treatment when fully resolved or improved to grade 1.
Interstitial lung disease (ILD), confirmed: Permanently discontinue.
Extemporaneously Prepared
For patients unable to swallow the tablet whole, place tablet in 120 to 240 ml water and stir for ~15 minutes; immediately drink the liquid or administer through a naso-gastric tube. Rinse the container with 120 to 240 mL water and immediately drink or administer through naso-gastric tube.
Iressa (gefitinib) [prescribing information]. Wilmington, DE: AstraZeneca; July 2015.
Administration
Administer with or without food.
For patients unable to swallow the tablet whole, place tablet in 120 to 240 mL water and stir for ~15 minutes; immediately drink the liquid or administer through a naso-gastric tube. Rinse the container with 120 to 240 mL water and immediately drink or administer through naso-gastric tube.
Storage
Store at 20°C to 25°C (68°F to 77°F).
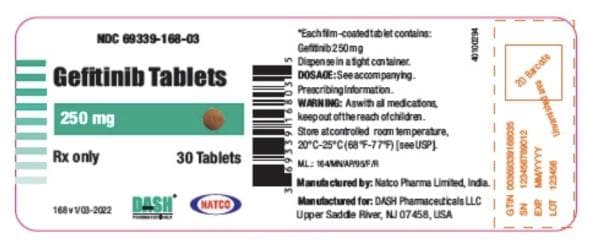
Gefitinib Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Antacids: May decrease the serum concentration of Gefitinib. Management: Administer gefitinib at least 6 hours before or after administration of an antacid, and closely monitor clinical response to gefitinib. Consider therapy modification
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Gefitinib. Management: In the absence of severe adverse reactions, increase gefitinib dose to 500 mg daily in patients receiving strong CYP3A4 inducers; resume 250 mg dose 7 days after discontinuation of the strong inducer. Carefully monitor clinical response. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Gefitinib. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Histamine H2 Receptor Antagonists: May decrease the serum concentration of Gefitinib. Management: Administer gefitinib at least 6 hours before or after administration of a histamine H2-antagonist, and closely monitor clinical response to gefitinib. Consider therapy modification
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Proton Pump Inhibitors: May decrease the serum concentration of Gefitinib. Management: Avoid use of proton pump inhibitors (PPIs) with gefitinib when possible. If required, administer gefitinib 12 hours after administration of the PPI or 12 hours before the next dose of the PPI. Consider therapy modification
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Vinorelbine: Gefitinib may enhance the neutropenic effect of Vinorelbine. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Gefitinib may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Insomnia (15%), fatigue (14%)
Dermatologic: Dermatological reaction (47% to 58%), skin rash (52%), xeroderma (24%), pruritus (18%), paronychia (14%), acne vulgaris (11%), alopecia (5% to 11%)
Gastrointestinal: Diarrhea (29% to 47%; grades 3/4: 3%), anorexia (19% to 20%), nausea (17% to 18%), decreased appetite (17%), vomiting (13% to 14%), stomatitis (7% to 13%), constipation (12%)
Genitourinary: Proteinuria (8% to 35%)
Hepatic: Increased serum AST (8% to 40%; grades 3/4: 2% to 3%), increased serum ALT (11% to 38%; grades 3/4: 2% to 5%)
Neuromuscular & skeletal: Weakness (18%)
1% to 10%:
Central nervous system: Hypoesthesia (4%), peripheral sensory neuropathy (4%), peripheral neuropathy (2%)
Dermatologic: Nail disease (5% to 8%), acneiform eruption (6%)
Endocrine & metabolic: Dehydration (2%; secondary to diarrhea, nausea, vomiting, or anorexia)
Gastrointestinal: Xerostomia (2%)
Genitourinary: Cystitis (1%)
Hematologic & oncologic: Anemia (7%), pulmonary hemorrhage (4% to 5%), hemorrhage (4%; including epistaxis, hematuria), neutropenia (3%), leukopenia (2%), thrombocytopenia (1%)
Hepatic: Increased serum bilirubin (3%; grades 3/4: <1%)
Neuromuscular & skeletal: Myalgia (8%), arthralgia (6%)
Ophthalmic: Eye disease (6% to 7%; grades 3/4: <1%; including conjunctivitis, blepharitis, and dry eye)
Renal: Increased serum creatinine (2%)
Respiratory: Cough (9%), interstitial pulmonary disease (1%; grades 3/4: 3%)
Miscellaneous: Fever (9%)
<1%, postmarketing, and/or case reports: Angioedema, bullous skin disease, corneal erosion (reversible; may be associated with aberrant eyelash growth), decreased white blood cell count, erythema multiforme, fulminant hepatitis, gastrointestinal perforation, hemorrhagic cystitis, hepatic failure, hepatitis, hypersensitivity angiitis, hypersensitivity reaction, keratitis, keratoconjunctivitis sicca, pancreatitis, renal failure, skin fissure, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Dermatologic toxicity: Skin reactions occurred in nearly one-half of patients taking gefitinib. Bullous skin disorders, including toxic epidermal necrolysis, Stevens Johnson syndrome, erythema multiforme, and dermatitis bullous have been reported. Interrupt gefitinib treatment or discontinue for development of severe bullous, blistering, or exfoliating dermatologic conditions.
- Gastrointestinal effects: Diarrhea occurs in approximately one-third of patients; grade 3 or 4 diarrhea has been observed. Diarrhea symptoms should be managed as clinically indicated; avoid dehydration. Withhold gefitinib for severe or persistent (up to 14 days) diarrhea. Gastrointestinal perforation has occurred (rarely); discontinue permanently if gastrointestinal perforation develops. Nausea, vomiting, decreased appetite, and stomatitis have also been reported.
- Hepatotoxicity: Increases in ALT, AST, and bilirubin, including grade 3 or higher toxicity have been observed. Fatal hepatotoxicity has occurred rarely. Monitor liver functions tests periodically. Withhold gefitinib in patients with worsening liver function; discontinue for severe hepatic impairment.
- Ocular toxicity: Ocular disorders, including keratitis, corneal erosion, abnormal eyelash growth, conjunctivitis, blepharitis, and dry eye have been reported; some events were grade 3. Recent corneal surgery and contact lens wearing may be risk factors for ocular toxicity. Advise patients to promptly report developing eye symptoms and promptly refer for ophthalmic evaluation if signs of keratitis (eg, acute or worsening of eye inflammation, lacrimation, blurred vision, pain, red eye, and/or light sensitivity). Interrupt gefitinib treatment or discontinue for severe or worsening ocular disorders.
- Pulmonary toxicity: Interstitial lung disease (ILD) or ILD-like reactions (eg, acute respiratory distress syndrome, lung infiltration, pneumonitis, or pulmonary fibrosis) have occurred (rarely) with gefitinib; some cases were grade 3 or higher and some were fatal. Withhold gefitinib and promptly assess any patient with worsening respiratory symptoms (dyspnea, cough, and fever); discontinue permanently if ILD is confirmed.
Disease-related concerns:
- Hepatic impairment: Gefitinib exposure is increased in patients with mild, moderate, and severe hepatic impairment due to cirrhosis. However, in a study of patients with liver metastases, patients with metastases and moderate impairment had similar systemic exposure as patients with metastases and normal hepatic function. Monitor for adverse reactions if administering to patients with moderate or severe hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Drugs that affect gastric pH: Elevated gastric pH may reduce gefitinib plasma concentrations; if possible, avoid concomitant use with proton pump inhibitors. If proton pump inhibitor therapy is necessary, administer gefitinib 12 hours before or 12 hours after the proton pump inhibitor dose. May administer gefitinib 6 hours before or 6 hours after H2-receptor antagonists or antacids.
Special populations:
- CYP2D6 poor metabolizers: Systemic exposure of gefitinib may be increased in CYP2D6 poor metabolizers. No dosage adjustment is recommended, although patients should be monitored closely for adverse reactions.
Other warnings/precautions:
- Appropriate use: Establish EGFR mutation status (in tumor or plasma specimen; if mutation is not detected in plasma, test tumor tissue if feasible) prior to treatment. Information on tests to detect EGFR mutations may be found at http://www.fda.gov/companiondiagnostics. Do not use in patients with EGFR mutation-negative tumors. Studies have demonstrated a subset of patients who are more likely to respond to gefitinib treatment. This subset includes patients of Asian origin, never-smokers, women, patients with bronchoalveolar adenocarcinoma, and patients with EGFR-mutated tumors. Deletion in exon 19 and mutation in exon 21 are the two most commonly found EGFR mutations; both mutations correlate with clinical response, resulting in increased response rates in patients with the mutation (Riely 2006). Studies have compared gefitinib in treatment naïve patients to combination chemotherapy in the subsets of patients described above, resulting in a longer progression free survival in the gefitinib arm (Mok 2009). ASCO guidelines state that the first-line use of gefitinib may be recommended in stage IV disease with activating EGFR mutations (Masters 2015). In patients with a KRAS mutation, however, EGFR-TKI therapy is not recommended.
Monitoring Parameters
EGFR mutation status (prior to treatment initiation) in tumor or plasma specimen; liver function tests (ALT, AST, bilirubin at baseline and periodically thereafter); INR or prothrombin time (with concurrent warfarin treatment). Monitor for signs/symptoms of dermatologic toxicity, gastrointestinal perforation, ocular toxicity, and pulmonary toxicity; monitor closely for adverse reactions in CYP2D6 poor metabolizers and patients with hepatic impairment. Monitor adherence.
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Gefitinib may cause fetal harm when administered to a pregnant female. Females of reproductive potential should use effective contraception during and for at least 2 weeks following gefitinib treatment.
Patient Education
What is this drug used for?
- It is used to treat lung cancer.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Skin irritation
- Acne
- Dry skin
- Nail changes
- Lack of appetite
- Dry eyes
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse
- Vision changes
- Eye pain
- Severe eye irritation
- Sensitivity to light
- Severe abdominal pain
- Chest pain
- Coughing up blood
- Mouth irritation
- Mouth sores
- Severe or persistent diarrhea
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.