Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection:
Glyrx-PF: 0.2 mg/mL (1 mL); 0.4 mg/2 mL (2 mL)
Robinul: 0.2 mg/mL (1 mL [DSC]); 0.4 mg/2 mL (2 mL [DSC]); 1 mg/5 mL (5 mL [DSC]); 4 mg/20 mL (20 mL [DSC]) [contains benzyl alcohol]
Generic: 0.2 mg/mL (1 mL); 0.4 mg/2 mL (2 mL); 1 mg/5 mL (5 mL); 4 mg/20 mL (20 mL)
Solution, Oral:
Cuvposa: 1 mg/5 mL (473 mL) [contains methylparaben, propylene glycol, propylparaben, saccharin sodium; cherry flavor]
Solution Prefilled Syringe, Injection [preservative free]:
Generic: 0.2 mg/mL (1 mL); 0.4 mg/2 mL (2 mL)
Tablet, Oral:
Glycate: 1.5 mg
Robinul: 1 mg [DSC] [scored]
Robinul-Forte: 2 mg [DSC] [scored]
Generic: 1 mg, 1.5 mg, 2 mg
Pharmacology
Mechanism of Action
Blocks the action of acetylcholine at parasympathetic sites in smooth muscle, secretory glands, and the CNS; indirectly reduces the rate of salivation by preventing the stimulation of acetylcholine receptors
Pharmacokinetics/Pharmacodynamics
Absorption
Oral tablet: Poor (~3%); variable and erratic; Oral solution: 23% lower compared to tablet; high-fat meal markedly reduces the oral bioavailability
Distribution
Vd: IV: Children and Adolescents ≤14 years: 1.3 to 1.8 L/kg (range: 0.7 to 3.9 L/kg); Adults: 0.42 ± 0.22 L/kg
Excretion
Urine (as unchanged drug, IM: >80%, IV: 85%); bile (as unchanged drug, <5%)
Clearance: Children and Adolescents ≤14 years: Mean range: 1.01 to 1.41 L/kg/hour (range: 0.32 to 2.22 L/kg/hour); Adults: 0.54 ± 0.14 L/kg/hour
Onset of Action
IM: 15 to 30 minutes; IV: Within 1 minute; Peak effect: IM: Within ~30 to 45 minutes
Time to Peak
3.1 hours
Duration of Action
Vagal effect: 2 to 3 hours; Inhibition of salivation: Up to 7 hours; Parenteral: 7 hours
Half-Life Elimination
IV: Infants: 21.6 to 130 minutes; Children: 19.2 to 99.2 minutes; IM: Adults: 0.55 to 1.25 hours; IV: 0.83 ± 0.27 hour; Oral solution: Adults: 3 hours
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination is severely impaired in patients with renal failure.
Use: Labeled Indications
Chronic drooling (Cuvposa only): To reduce chronic, severe drooling in pediatric patients 3 to 16 years with neurologic conditions (eg, cerebral palsy) associated with problem drooling
Reduction of secretions (injection only): To reduce salivary, tracheobronchial, and pharyngeal secretions and to reduce the volume and acidity of gastric secretions during induction of anesthesia and intubation
Reversal of bradycardia, vagal reflexes (injection only): To block cardiac vagal inhibitory reflexes during induction of anesthesia and intubation; intraoperatively to counteract surgically or drug-induced or vagal reflexes associated arrhythmias
Reversal of muscarinic effects of cholinergic agents (injection only): Protects against the peripheral muscarinic effects (eg, bradycardia, excessive secretions) of cholinergic agents (eg, neostigmine, pyridostigmine) given to reverse the neuromuscular blockade due to non-depolarizing muscle relaxants
Use: Off Label
Primary focal hyperhidrosiscyes
Retrospective data from a limited number of patients suggests that systemic therapy with oral glycopyrrolate may be beneficial for treatment of primary focal hyperhidrosis Bajaj 2007, Lee 2012, Walling 2012. The Canadian Hyperhidrosis Advisory Committee guideline on treatment of primary focal hyperhidrosis recommends oral glycopyrrolate as an option for first-line therapy of craniofacial hyperhidrosis and as alternative therapy in severe cases of axillary, palmar, or plantar hyperhidrosis unresponsive to first- or second-line therapies Solish 2007. Additional data may be necessary to further define the role of glycopyrrolate in this condition.
Contraindications
Hypersensitivity to glycopyrrolate or any component of the formulation; medical conditions that preclude use of anticholinergic medication (eg, severe ulcerative colitis, toxic megacolon complicating ulcerative colitis, paralytic ileus, obstructive disease of GI tract [eg, achalasia, pyloroduodenal stenosis], intestinal atony in elderly or debilitated patients, unstable cardiovascular status in acute hemorrhage, glaucoma, obstructive uropathy [eg, bladder neck obstruction due to prostatic hypertrophy], myasthenia gravis)
Oral solution: Additional contraindication: Concomitant use of potassium chloride in a solid oral dosage form
Dosage and Administration
Dosing: Adult
Primary focal hyperhidrosis (off-label): Limited data available: Oral: 1 to 2 mg once or twice daily may be a typical effective dosage range (Walling 2012); titrate per response and tolerability; doses up to 6 to 8 mg per day in 2 or 3 divided doses have been used in some patients (Bajaj 2007; Solish 2007; Walling 2012).
Reduction of secretions (preoperative): IM: 4 mcg/kg 30 to 60 minutes before anesthesia or when the preanesthetic opioid and/or sedative are administered
Reversal of bradycardia, vagal reflexes (intraoperative): IV: 0.1 mg as a single dose; repeat as needed at 2- to 3-minute intervals
Reversal of muscarinic effects of cholinergic agents: IV: 0.2 mg for each 1 mg of neostigmine or 5 mg of pyridostigmine administered
Dosing: Geriatric
Refer to adult dosing. Use with caution; consider dose reduction.
Dosing: Pediatric
Chronic drooling: Children ≥3 years and Adolescents ≤16 years: Oral solution (Cuvposa): 20 mcg/kg/dose 3 times daily, titrate in increments of 20 mcg/kg/dose every 5 to 7 days as tolerated to response up to a maximum dose of 100 mcg/kg/dose 3 times daily; not to exceed 1,500 to 3,000 mcg/dose
Control of respiratory secretions, palliative care: Limited data available: Children: Oral: 40 to 100 mcg/kg/dose every 4 to 8 hours (Kliegman 2016)
Reduction of secretions (preoperative):
Infants and Children ≤2 years: IM: 4 to 9 mcg/kg/dose 30 to 60 minutes before procedure
Children >2 years and Adolescents: IM: 4 mcg/kg/dose 30 to 60 minutes before procedure
Reversal of bradycardia, vagal reflexes (intraoperative): Infants, Children, and Adolescents: IV: 4 mcg/kg/dose (maximum dose: 100 mcg/dose) at 2 to 3 minute intervals
Reversal of muscarinic effects of cholinergic agents: Infants, Children, and Adolescents: IV: 0.2 mg for each 1 mg of neostigmine or 5 mg of pyridostigmine administered
Reconstitution
IV: May further dilute in a compatible solution.
Extemporaneously Prepared
Note: A glycopyrrolate oral solution (0.2 mg/mL) is commercially available.
0.5 mg/mL Oral Suspension
A 0.5 mg/mL oral suspension may be made with 1 mg tablets and a 1:1 mixture of Ora-Plus and either Ora-Sweet or Ora-Sweet SF. Crush thirty 1 mg tablets in a mortar and reduce to a fine powder. Prepare diluent by mixing 30 mL of Ora-Plus with 30 mL of either Ora-Sweet or Ora-Sweet SF and stir vigorously. Add 30 mL of diluent (via geometric dilution) to powder until smooth suspension is obtained. Transfer suspension to 60 mL amber bottle. Rinse contents of mortar into bottle with sufficient quantity of remaining diluent to obtain 60 mL (final volume). Label “shake well”. Stable at room temperature for 90 days. Due to bitter aftertaste, chocolate syrup may be administered prior to or mixed (1:1 v/v) with suspension immediately before administration (Cober 2011).
Cober MP, Johnson CE, Sudekum D, et al. Stability of extemporaneously prepared glycopyrrolate oral suspensions. Am J Health Syst Phar. 2011;68(9):843-845.21515869
A 0.5 mg/mL oral solution can be made from tablets. Crush fifty 1 mg tablets in a mortar and reduce to a fine powder. Add enough distilled water to make about 90 mL, mix well. Transfer to a bottle, rinse mortar with water, and add a quantity of water sufficient to make 100 mL. Label “shake well” and “protect from light”. Stable at room temperature for 25 days (Gupta 2001).
Gupta VD. Stability of an oral liquid dosage form of glycopyrrolate prepared from tablets. Int J Pharm Compd. 2001;5(6):480-481.23982044
0.1 mg/mL Oral Solution
A 0.1 mg/mL oral solution may be made using glycopyrrolate 0.2 mg/mL injection without preservatives. Withdraw 50 mL from vials with a needle and syringe, add to 50 mL of a 1:1 mixture of Ora-Sweet and Ora-Plus in a bottle. Label “shake well”, “protect from light,” and “refrigerate”. Stable refrigerated for 35 days (Landry 2005).
Landry C, Forest JM, Hildgen P. Stability and subjective taste acceptability of four glycopyrrolate solutions for oral administration. Int J Pharm Compd. 2005;9(5):396-398.23925137
Administration
IM: May administer undiluted.
IV: May be administered IV without dilution or may dilute in a compatible solution. In perioperative setting, usually administered over 1 to 2 minutes (eg, in adults: 0.2 mg over 1 to 2 minutes). May also be administered via the tubing of a running IV infusion of a NS. May be administered IV in the same syringe with neostigmine or pyridostigmine for reversal of neuromuscular blockade.
Oral: Administer oral solution 1 hour before or 2 hours after meals. Measure oral solution with an accurate measuring device (eg, dosing cup or oral syringe).
Storage
Injection: Store at 20°C to 25°C (68°F to 77°F).
Oral: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
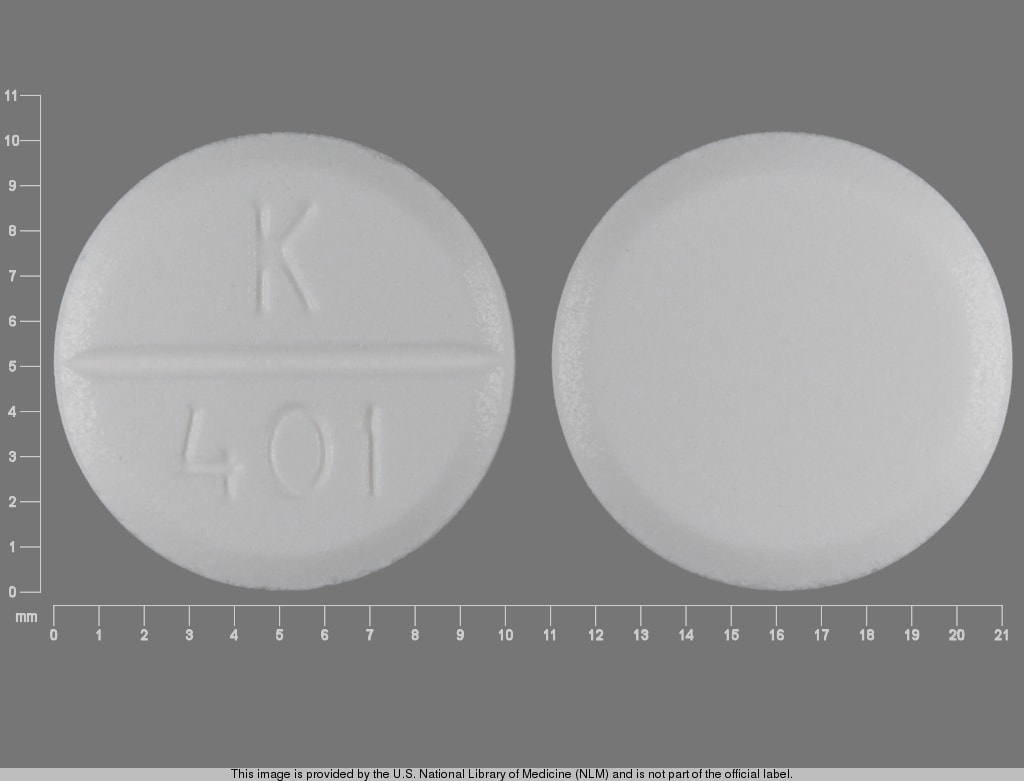
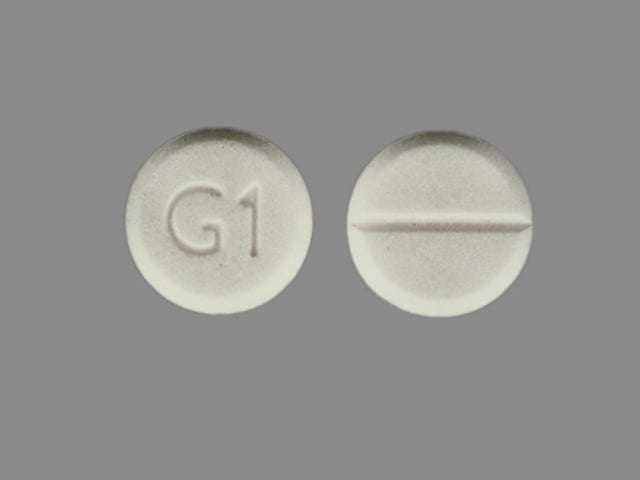
Glycopyrrolate (Systemic) Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Glycopyrrolate (Systemic). Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Atenolol: Glycopyrrolate (Systemic) may increase the serum concentration of Atenolol. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Digoxin: Glycopyrrolate (Systemic) may increase the serum concentration of Digoxin. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Haloperidol: Glycopyrrolate (Systemic) may decrease the serum concentration of Haloperidol. Management: Monitor patients closely for signs/symptoms of reduced clinical response to haloperidol if concurrent use with glycopyrrolate is required. When possible, consider avoiding concurrent use. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levodopa-Containing Products: Glycopyrrolate (Systemic) may decrease the serum concentration of Levodopa-Containing Products. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
MetFORMIN: Glycopyrrolate (Systemic) may increase the serum concentration of MetFORMIN. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Glycopyrrolate (Systemic) may enhance the adverse/toxic effect of Potassium Chloride. This is specific to solid oral dosage forms of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
Frequency not always defined.
Cardiovascular: Flushing (30%), pallor (≤2%), cardiac arrhythmias, heart block, hypertension, hypotension, palpitation, tachycardia
Central nervous system: Headache (15%), aggressiveness (≤2%), agitation (≤2%), crying (abnormal; ≤2%), irritability (≤2%), mood changes (≤2%), pain (≤2%), restlessness (≤2%), confusion, dizziness, drowsiness, excitement (higher incidence in older adults), insomnia, nervousness
Dermatologic: Dry skin (≤2%), pruritus (≤2%), rash (≤2%), hypohidrosis, urticaria
Endocrine & metabolic: Dehydration (≤2%)
Gastrointestinal: Vomiting (40%), xerostomia (40%), constipation (35%), abdominal distention (≤2%), abdominal pain (≤2%), flatulence (≤2%), retching (≤2%), intestinal obstruction, loss of taste, nausea, pseudo-obstruction
Genitourinary: Urinary retention (15%), urinary tract infection (≤2%), decreased lactation, impotence, urinary hesitancy
Neuromuscular & skeletal: Weakness
Ophthalmic: Nystagmus (≤2%), blurred vision, cycloplegia, increased intraocular pressure, mydriasis
Respiratory: Nasal congestion (30%), sinusitis (15%), upper respiratory tract infection (15%), bronchial secretion (thickening; ≤2%), nasal dryness (≤2%), pneumonia (≤2%)
<1%, postmarketing, and/or case reports: Arrhythmias, hypertension, hypotension, malignant hyperthermia, seizure
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May cause drowsiness and/or blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- GI transit: Slowing of GI muscular action can occur resulting in constipation or intestinal pseudo-obstruction. Constipation is a common dose-limiting adverse event. Intestinal pseudo-obstruction can result in abdominal distention, pain, nausea, or vomiting; discontinue if these symptoms develop or worsen during treatment.
- Heat prostration: May occur in the presence of fever, increased environmental temperature, and/or during physical exercise, particularly in children and the elderly; use caution in hot weather and/or exercise. Avoid exertion and high environmental temperature after administration.
- Mechanical obstruction (incomplete): Diarrhea may be an early sign of incomplete intestinal obstruction, especially in patients with an ileostomy or colostomy; avoid use in these patients. Discontinue treatment if incomplete mechanical intestinal obstruction is suspected or if diarrhea occurs.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with coronary artery disease, arrhythmias, heart failure, hypertension, or tachycardia; evaluate tachycardia prior to administration.
- Hepatic impairment: Use with caution in patients with hepatic impairment; consider dosage reduction.
- Hiatal hernia: Use with caution in patients with hiatal hernia with reflux esophagitis; consider dosage reduction.
- Hyperthyroidism: Use with caution in patients with hyperthyroidism.
- Neuropathy: Use with caution in patients with autonomic neuropathy; consider dosage reduction.
- Prostatic hyperplasia/bladder neck obstruction: May worsen the symptoms (eg, urinary retention) of prostatic hyperplasia and/or bladder neck obstruction; use with caution; consider dosage reduction in patients with prostatic hypertrophy.
- Renal impairment: Use with caution in patients with renal impairment; elimination is severely impaired in renal failure; dosage adjustment may be necessary.
- Ulcerative colitis: Use with caution in patients with ulcerative colitis; large doses may suppress intestinal motility; consider dosage reduction; may precipitate/exacerbate an ileus or toxic megacolon. Use is contraindicated in patients with severe ulcerative colitis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly; increased risk for anticholinergic effects, confusion, and hallucinations; consider dosage reduction.
- Pediatric: Infants, patients with Down syndrome, and pediatric patients with spastic paralysis or brain damage may experience an increased response to anticholinergics, increasing the potential for adverse events. A paradoxical reaction characterized by hyperexcitability may occur in pediatric patients taking large doses. Infants and young children are especially susceptible to the toxic effects of anticholinergics.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Glyrx-PR: Sensitivity of the eyes to light may occur. Protect eyes from light after administration.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Monitoring Parameters
Heart rate; anticholinergic effects; bowel sounds; bowel movements; effects on drooling
Pregnancy
Pregnancy Risk Factor
B (injection)
Pregnancy Considerations
Glycopyrrolate does not appear to penetrate through the placental barrier in significant amounts. Glycopyrrolate in doses of 0.004 mg/kg has not been found to affect fetal heart rate or fetal heart rate variability to a significant degree.
Patient Education
What is this drug used for?
- It is used to treat GI (gastrointestinal) ulcers.
- It is used to reduce drooling.
- In surgery, it is used to lower secretions such as saliva.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Blurred vision
- Flushing
- Dry mouth
- Dizziness
- Change in taste
- Headache
- Stuffy nose
- Anxiety
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lack of sweating
- Confusion
- Difficult urination
- Fast heartbeat
- Abnormal heartbeat
- Fast breathing
- Enlarged pupils
- Vision changes
- Eye pain
- Severe eye irritation
- Diarrhea
- Bloating
- Constipation
- Abdominal edema
- Abdominal pain
- Severe nausea
- Vomiting
- Muscle weakness
- Sexual dysfunction
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.