Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Kit, Subcutaneous:
Supprelin LA: 50 mg
Vantas: 50 mg
Pharmacology
Mechanism of Action
Potent inhibitor of gonadotropin secretion; continuous administration results in, after an initiation phase, the suppression of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and a subsequent decrease in testosterone and dihydrotestosterone (males) and estrone and estradiol (premenopausal females). Testosterone levels are reduced to castrate levels in males (treated for prostate cancer) within 2 to 4 weeks. Additionally, in patients with CPP, linear growth velocity is slowed (improves chance of attaining predicted adult height).
Pharmacokinetics/Pharmacodynamics
Distribution
Adults: Vd: ~58.4 L ± 7.86 L
Metabolism
Hepatic via C-terminal dealkylation and hydrolysis
Onset of Action
Prostate cancer: Chemical castration: Within 2 to 4 weeks; CPP: Progression of sexual development stops and growth is decreased within 1 month
Time to Peak
Adults: 12 hours
Duration of Action
12 months (plus a few additional weeks of histrelin release)
Half-Life Elimination
Adults: Terminal: ~4 hours
Protein Binding
Adults: ~70% ± 9%
Use in Specific Populations
Special Populations: Renal Function Impairment
Average serum histrelin concentrations are approximately 50% higher in patients with renal function impairment.
Use: Labeled Indications
Central precocious puberty (Supprelin LA): Treatment of children with central precocious puberty
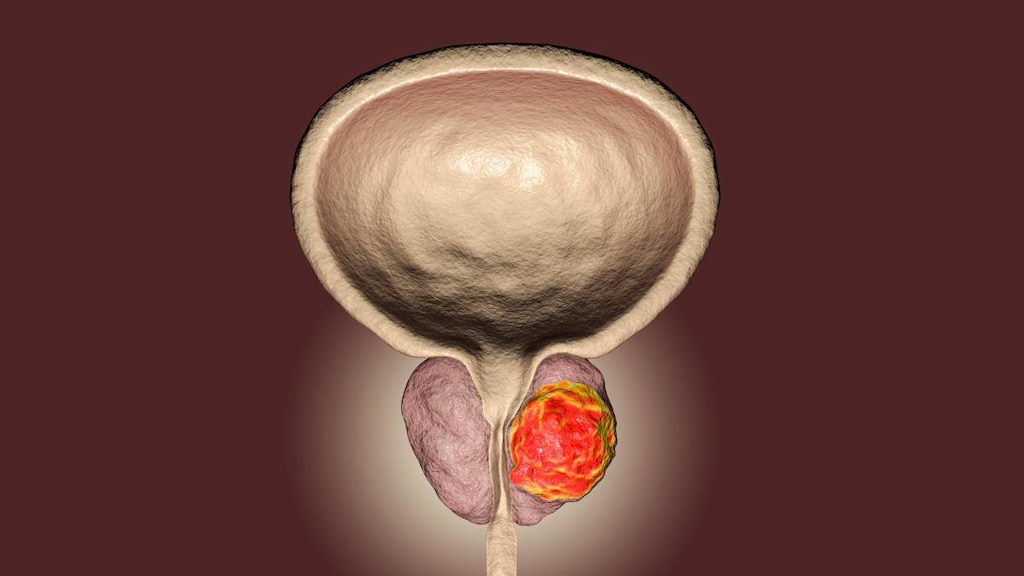
Prostate cancer, advanced (Vantas): Palliative treatment of advanced prostate cancer
Contraindications
Hypersensitivity to histrelin acetate, gonadotropin-releasing hormone (GnRH), GnRH-agonist analogs, or any component of the formulation; females who are or may become pregnant
Dosage and Administration
Dosing: Adult
Prostate cancer, advanced (Vantas): SubQ: 50 mg implant surgically inserted every 12 months
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Central precocious puberty: Children ≥2 years: Supprelin LA: SubQ: 50 mg implant surgically inserted every 12 months; discontinue at the appropriate time for the onset of puberty
Reconstitution
The implant may be slightly curved and/or partially flattened when removed from refrigerator; may roll implant (in sterile-gloved hands) a few times between fingers and thumb. If resistance is felt when inserting implant into insertion tool cannula, remove and manually manipulate or roll as needed and reinsert into cannula.
Administration
SubQ: Surgical implantation (using a sterile field) into the inner portion of the upper arm requires the use of the implantation device provided. Do not bend or pinch the implant. Use the patient's nondominant arm for placement; implant should be placed halfway between the shoulder and the elbow at the crease between the tricep and the bicep. Implant removal should occur after ~12 months; a replacement implant may be inserted if therapy is to be continued. Palpate area of incision to locate implant for removal. If not readily palpated, ultrasound, CT, or MRI may be used to locate implant; plain films are not recommended because the implant is not radiopaque. Refer to manufacturer's labeling for full insertion and removal details.
Storage
Upon delivery, separate contents of implant carton. Store implant (small carton containing amber plastic pouch and glass vial) under refrigeration at 2°C to 8°C (36°F to 46°F) until the day of insertion; excursions permitted to 25°C (77°F) for 7 days (if unused within 7 days, may return to proper refrigeration until product expiration date). Keep implant wrapped in the amber pouch for protection from light; do not freeze. Do not open implant vial until just before the time of insertion. The implantation insertion kit should be stored at room temperature (do not refrigerate insertion kit).
Drug Interactions
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Choline C 11: Luteinizing Hormone-Releasing Hormone Analogs may diminish the therapeutic effect of Choline C 11. Monitor therapy
Corifollitropin Alfa: Luteinizing Hormone-Releasing Hormone Analogs may enhance the therapeutic effect of Corifollitropin Alfa. Avoid combination
Indium 111 Capromab Pendetide: Luteinizing Hormone-Releasing Hormone Analogs may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Test Interactions
Results of diagnostic test of pituitary gonadotropic and gonadal functions may be affected during and after therapy
Adverse Reactions
CPP:
>10%: Dermatologic: Dermatological reaction (51%; insertion site reaction includes bruise, discomfort, erythema, pain, protrusion of implant area, pruritus, soreness, swelling, tingling)
1% to 10%:
Central nervous system: Emotional lability (≤2%), headache (≤2%), migraine (≤2%), sensation of cold (≤2%)
Dermatologic: Cicatrix of skin (6%), pruritus (≤2%)
Endocrine & metabolic: Gynecomastia (≤2%), heavy menstrual bleeding (≤2%), weight gain (≤2%)
Genitourinary: Uterine hemorrhage (4%), breast tenderness (≤2%), dysmenorrhea (≤2%), precocious puberty (≤2%; progression of central precocious puberty)
Hematologic & oncologic: Pituitary neoplasm (≤2%)
Infection: Localized infection (≤2%; implant site)
Local: Application site pain (4%)
Neuromuscular & skeletal: Keloid-like scar (6%)
Respiratory: Epistaxis (≤2%), flu-like symptoms (≤2%)
Miscellaneous: Procedural complications (6%; suture-related), postoperative pain (4%)
Frequency not defined: Endocrine & metabolic: Altered hormone levels
1%, postmarketing, and/or case reports: Aggressive behavior, amblyopia, crying, hostility, irritability, seizure, suicidal ideation
Prostate cancer:
>10%:
Dermatologic: Dermatological reaction (3% to 14%)
Endocrine & metabolic: Hot flash (66%)
1% to 10%:
Cardiovascular: Flushing (<2%), palpitations (<2%), peripheral edema (<2%), ventricular premature contractions (<2%)
Central nervous system: Fatigue (10%), headache (3%), insomnia (3%), depression (<2%), dizziness (<2%), irritability (<2%), lethargy (<2%), malaise (<2%), pain (<2%), sensation of cold (<2%)
Dermatologic: Diaphoresis (<2%), genital pruritus (<2%), hypotrichosis (<2%), night sweats (<2%), pruritus (<2%)
Endocrine & metabolic: Gynecomastia (4%), decreased libido (2%), weight gain (2%), fluid retention (<2%), hypercalcemia (<2%), hypercholesterolemia (<2%), increased lactate dehydrogenase (<2%), increased prostatic acid phosphatase (<2%), increased serum glucose (<2%), weight loss (<2%)
Gastrointestinal: Constipation (4%), abdominal distress (<2%), food cravings (<2%), increased appetite (<2%), nausea (<2%)
Genitourinary: Testicular atrophy (5%; expected pharmacological consequence of testosterone suppression), erectile dysfunction (4%), breast tenderness (<2%), dysuria (<2%), exacerbation of gynecomastia (<2%), exacerbation of hematuria (<2%), exacerbation of urinary frequency (<2%), hematuria (<2%), mastalgia (<2%), urinary frequency (<2%), urinary retention (<2%)
Hematologic & oncologic: Anemia (<2%), bruise (<2%), hematoma (<2%)
Hepatic: Hepatic disease (<2%), increased serum AST (<2%)
Local: Bruising at injection site (7%), pain at injection site (≤4%), tenderness at injection site (≤4%), erythema at injection site (3%), inflammation at injection site (1%), injection site infection (1%)
Neuromuscular & skeletal: Arthralgia (<2%), asthenia (<2%), back pain (<2%), exacerbation of back pain (<2%), limb pain (<2%), muscle twitching (<2%), myalgia (<2%), neck pain (<2%), ostealgia (<2%), tremor (<2%)
Renal: Renal insufficiency (5%), decreased creatinine clearance (<2%), exacerbation of renal failure (<2%), nephrolithiasis (<2%)
Respiratory: Dyspnea on exertion (<2%)
Miscellaneous: Stent occlusion (<2%)
<1%, postmarketing, and/or case reports: Decreased bone mineral density, hepatic injury (severe), increased testosterone level, swelling at injection site
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Androgen-deprivation therapy (ADT) may increase the risk for cardiovascular disease (Levine 2010). An increased risk of MI, sudden cardiac death, and stroke has been reported with GnRH agonist use in men; monitor for symptoms associated with cardiovascular disease. ADT may prolong the QT/QTc interval; consider the benefits of ADT versus the risk for QT prolongation in patients with a history of QTc prolongation, congenital long QT syndrome, heart failure, frequent electrolyte abnormalities, and in patients with medications known to prolong the QT interval, or with pre-existing cardiac disease. Consider periodic monitoring of electrocardiograms and electrolytes in at-risk patients.
- Hyperglycemia: Hyperglycemia has been reported with androgen deprivation therapy (in prostate cancer) and may manifest as diabetes or worsening of preexisting diabetes. Monitor blood glucose and/or HbA1c.
- Pituitary apoplexy: Rare cases of pituitary apoplexy (frequently secondary to pituitary adenoma) have been observed with GnRH agonist administration (onset from 1 hour to usually <2 weeks); may present as sudden headache, vomiting, visual or mental status changes, and infrequently, cardiovascular collapse; immediate medical attention required.
- Psychiatric events: Psychiatric events have been described with GnRH agonists, including histrelin; symptoms of emotional lability, irritability, impatience, anger, and aggression have been reported in postmarketing accounts. Monitor for development or worsening of psychiatric symptoms.
- Seizures: Seizures have been reported in patients receiving GnRH agonists, including histrelin. Reports have occurred in patients with a history of seizures, epilepsy, cerebrovascular disorders, CNS anomalies, or tumors, and patients on concomitant medications associated with seizures (eg, bupropion, SSRIs). Seizures have also been reported in patients without underlying conditions.
- Spinal cord compression: Has been reported, may contribute to paralysis when used for prostate cancer; closely observe patients with metastatic vertebral lesions for weakness and paresthesias in first few weeks of therapy.
- Tumor flare: Transient increases in serum testosterone (in men with prostate cancer) occur during the first week of use and may result in a worsening of disease signs and symptoms (bone pain, neuropathy, hematuria, ureteral/bladder outlet obstruction, spinal cord compression) during the first week of treatment.
- Urinary tract obstruction: Ureteral obstruction may occur when used for prostate cancer; closely observe patients for urinary tract obstruction or poor urine output in first few weeks of therapy.
- Worsening of symptoms: Transient increases in estradiol serum levels (female) or testosterone levels (female and male) may occur during the first week of use for central precocious puberty (CPP); however, manifestations of puberty should decrease within 4 weeks.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Implant complications: Proper surgical insertion technique is essential to avoid complications. Patients should keep arm dry for 24 hours and avoid heavy lifting/strenuous exertion of insertion arm for 7 days after implantation. In prostate cancer studies, the implant was not recovered in a small number of patients. Serum testosterone rose above castrate level and the implant was not palpable or visualized (via ultrasound); it was believed to have been extruded. Some patients had continued testosterone levels below castration level even though the implant was not palpable. If the implant breaks during removal in children with CPP, the remaining pieces should be removed; confirm the removal of the entire implant (refer to manufacturer's instructions for removal procedure).
Monitoring Parameters
Central precocious puberty (CPP): Luteinizing hormone, follicle-stimulating hormone, estradiol, or testosterone (after 1 month then every 6 months); height, bone age (every 6 to 12 months); Tanner staging; monitor for clinical evidence of suppression of CPP manifestations; monitor for development or worsening of psychiatric symptoms, including depression.
Prostate cancer: Serum testosterone levels, prostate specific antigen (PSA); bone mineral density; weakness, paresthesias, and urinary tract obstruction (especially during first few weeks of therapy); screen for diabetes; monitor for symptoms associated with cardiovascular disease. Consider periodic monitoring of electrocardiograms and electrolytes.
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Histrelin is contraindicated for use during pregnancy or in women who may become pregnant. May cause fetal harm or spontaneous abortion if administered during pregnancy.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience application site irritation, loss of strength and energy, or constipation. Have patient report immediately to prescriber signs of high blood sugar (confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), seizures, burning or numbness feeling, unable to pass urine, change in amount of urine passed, painful urination, blood in the urine, bone pain, weakness, difficulty moving, severe dizziness, passing out, fast heartbeat, abnormal heartbeat, signs of pituitary apoplexy (sudden headache, vomiting, passing out, mood changes, eye weakness, unable to move eyes, or vision changes), behavioral changes, or mood changes (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.