Boxed Warning
Fetal risk:
Do not use lenalidomide during pregnancy. Lenalidomide, a thalidomide analogue, caused limb abnormalities in a developmental monkey study. Thalidomide is a known human teratogen that causes severe, life-threatening human birth defects. If lenalidomide is used during pregnancy, it may cause birth defects or embryo-fetal death. In females of reproductive potential, obtain 2 negative pregnancy tests before starting lenalidomide treatment. Females of reproductive potential must use 2 forms of contraception or continuously abstain from heterosexual sex during and for 4 weeks after lenalidomide treatment. To avoid embryo-fetal exposure to lenalidomide, it is only available under a restricted distribution program called Revlimid REMS program.
Information about the Revlimid REMS program is available at http://www.celgeneriskmanagement.com or by calling the manufacturer's toll-free number 1-888-423-5436.
Hematologic toxicity:
Lenalidomide can cause significant neutropenia and thrombocytopenia. Eighty percent of patients with deletion 5q myelodysplastic syndromes had to have a dose delay/reduction during the major study. Thirty-four percent of patients had to have a second dose delay/reduction. Grade 3 or 4 hematologic toxicity was seen in 80% of patients enrolled in the study. Patients on therapy for deletion 5q myelodysplastic syndromes should have their complete blood cell counts monitored weekly for the first 8 weeks of therapy and at least monthly thereafter. Patients may require dose interruption and/or reduction. Patients may require use of blood product support and/or growth factors.
Venous and arterial thromboembolism:
Lenalidomide has demonstrated a significantly increased risk of deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as risk of myocardial infarction and stroke in patients with multiple myeloma who were treated with lenalidomide and dexamethasone therapy. Monitor for and advise patients about the signs and symptoms of thromboembolism. Advise patients to seek immediate medical care if they develop symptoms such as shortness of breath, chest pain, or arm or leg swelling. Thromboprophylaxis is recommended and the choice of regimen should be based on an assessment of the patient's underlying risk factors.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Revlimid: 2.5 mg [contains fd&c blue #2 (indigotine)]
Revlimid: 5 mg
Revlimid: 10 mg, 15 mg, 20 mg [contains fd&c blue #2 (indigotine)]
Revlimid: 25 mg
Pharmacology
Mechanism of Action
Lenalidomide has immunomodulatory, antiangiogenic, and antineoplastic characteristics via multiple mechanisms. It selectively inhibits secretion of proinflammatory cytokines (potent inhibitor of tumor necrosis factor-alpha secretion); enhances cell-mediated immunity by stimulating proliferation of anti-CD3 stimulated T cells (resulting in increased IL-2 and interferon gamma secretion); inhibits trophic signals to angiogenic factors in cells. Inhibits the growth of myeloma, myelodysplastic, and lymphoma tumor cells by inducing cell cycle arrest and cell death. The addition of lenalidomide to rituximab increases antibody dependent cell-mediated cytotoxicity in follicular lymphoma and marginal zone lymphoma and increases tumor cell apoptosis in follicular lymphoma (compared to rituximab alone).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Excretion
Urine (~82%; as unchanged drug); Hemodialysis effect: ~30% of the drug in body is removed in a 4-hour hemodialysis session; Hemodialysis patients: 80% decrease in drug clearance compared with healthy subjects.
Time to Peak
MDS or myeloma patients: 0.5 to 6 hours
Half-Life Elimination
3 to 5 hours
Protein Binding
~30%
Use in Specific Populations
Special Populations: Renal Function Impairment
The half-life is increased 3-fold in moderate to severe renal impairment and increased ~4.5-fold in hemodialysis patients, compared to healthy patients. There is a 66% to 75% decrease in drug clearance in patients with moderate and severe renal impairment compared with healthy subjects. Hemodialysis patients had an 80% decrease in drug clearance compared with healthy subjects.
Use: Labeled Indications
Follicular lymphoma: Treatment of previously treated follicular lymphoma (in combination with a rituximab product) in adults.
Mantle cell lymphoma: Treatment of mantle cell lymphoma in adults that has relapsed or progressed after 2 prior therapies (one of which included bortezomib).
Marginal zone lymphoma: Treatment of previously treated marginal zone lymphoma (in combination with a rituximab product) in adults.
Multiple myeloma: Treatment of multiple myeloma (in combination with dexamethasone) in adults; maintenance therapy following autologous hematopoietic stem cell transplantation in adults.
Myelodysplastic syndromes: Treatment of adults with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes (MDS) associated with a deletion 5q (del 5q) cytogenetic abnormality with or without additional cytogenetic abnormalities.
Limitations of use: Lenalidomide is not indicated and is not recommended for the treatment of chronic lymphocytic leukemia (CLL) outside of controlled clinical trials.
Use: Off Label
Chronic lymphocytic leukemia, relapsed or refractoryb
Data from a phase 2 study in patients with relapsed or refractory chronic lymphocytic leukemia (CLL), support the use of lenalidomide (in combination with cyclic rituximab) in the treatment of patients with CLL Badoux 2013.
Diffuse large B-cell lymphoma, relapsed or refractoryb
Data from a phase 2, single-arm, multicenter study in patients with relapsed or refractory aggressive non-Hodgkin lymphoma support the use of lenalidomide in the treatment of patients with this condition Wiernik 2008.
Multiple myeloma, newly diagnoseda
Data from a phase 3 trial in patients who were ineligible for autologous stem cell transplant support the use of lenalidomide (in combination with daratumumab and dexamethasone) in the treatment of newly diagnosed multiple myeloma Facon 2019. Data from two phase 2 trials in patients with newly diagnosed multiple myeloma support the use of lenalidomide (in combination with bortezomib and dexamethasone) in the treatment of this condition Kumar 2012, Richardson 2010. In addition, data from a small phase 1/2 trial support the use of lenalidomide (in combination with carfilzomib and dexamethasone) for the treatment of newly diagnosed multiple myeloma Jakubowiak 2012.
Myelodysplastic syndrome without deletion 5qb
Data from a phase 2, multicenter study in patients with myelodysplastic syndrome (MDS) support the use of lenalidomide in the treatment of patients with MDS without deletion 5q Raza 2008.
Systemic light chain amyloidosisb
Data from two phase 2 studies in patients with systemic light chain amyloidosis support the use of lenalidomide in the treatment of patients with this condition Nair 2012, Sanchorawala 2007.
Contraindications
Severe hypersensitivity (eg, angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis) to lenalidomide or any component of the formulation; pregnancy
Canadian labeling: Additional contraindications (not in the US labeling): Platelet count <50,000/mm3 (in MDS patients); hypersensitivity to thalidomide or pomalidomide; females capable of becoming pregnant; breastfeeding; male patients unable to follow or comply with required contraceptive measures
Dosage and Administration
Dosing: Adult
Chronic lymphocytic leukemia, relapsed/refractory (off-label use): Oral: 10 mg once daily beginning on day 9 of cycle 1; administer continuously in combination with cyclic rituximab (Badoux 2013).
Diffuse large B-cell lymphoma, relapsed/refractory (off-label use): Oral: 25 mg once daily for 21 days of a 28-day treatment cycle for up to 1 year (Wiernik 2008).
Follicular lymphoma: Oral: 20 mg once daily for 21 days of a 28-day treatment cycle (in combination with rituximab) for up to 12 cycles (Leonard 2019).
Mantle cell lymphoma: Oral: 25 mg once daily for 21 days of a 28-day treatment cycle; continue until disease progression or unacceptable toxicity (Goy 2013).
Marginal zone lymphoma: Oral: 20 mg once daily for 21 days of a 28-day treatment cycle (in combination with rituximab) for up to 12 cycles (Leonard 2019).
Multiple myeloma: Oral: 25 mg once daily for 21 days of a 28-day treatment cycle (in combination with dexamethasone [consider a reduced dexamethasone dose in patients >75 years of age]). In patients not eligible for autologous stem cell transplantation, continue until disease progression or unacceptable toxicity occurs; in transplant eligible patients, hematopoietic stem cell mobilization should occur within 4 cycles of a lenalidomide-containing therapy.
Multiple myeloma, maintenance (following autologous stem cell transplant): Oral: 10 mg once daily (begin after adequate hematologic recovery [ANC ≥1,000/mm3; platelets ≥75,000/mm3]); continue until disease progression or unacceptable toxicity occurs. If tolerated, may increase dose to 15 mg once daily after 3 cycles (each cycle is 28 days).
Off-label dosing: 10 mg once daily for 21 days of a 28-day treatment cycle until relapse (Palumbo 2010).
Multiple myeloma, newly diagnosed (off-label combination): Oral: 25 mg once daily for 21 days of a 28-day cycle (in combination with daratumumab and dexamethasone) until disease progression or unacceptable toxicity occurs (Facon 2019) or 25 mg once daily for 14 days of a 21-day cycle (in combination with bortezomib and dexamethasone) for 8 cycles (Kumar 2012; Richardson 2010) or 25 mg once daily for 21 days of a 28-day cycle (in combination with carfilzomib and dexamethasone) for up to 8 cycles (Jakubowiak 2012).
Multiple myeloma, relapsed (off-label combinations): Adults: Oral: 25 mg once daily for 21 days of 28-day cycle (in combination with carfilzomib and dexamethasone) until disease progression or unacceptable toxicity occurs (Stewart 2015) or 25 mg once daily for 21 days of a 28-day cycle (in combination with daratumumab and dexamethasone) until disease progression or unacceptable toxicity occurs; refer to the IMWG recommendations for Dosing in Renal Impairment (Dimopoulos 2016a; Dimopoulos 2016b).
Myelodysplastic syndrome with deletion 5q: Oral: 10 mg once daily, continue until disease progression or unacceptable toxicity occurs.
Myelodysplastic syndrome, lower risk, without deletion 5q (off-label use): Oral: 10 mg once daily (Raza 2008).
Systemic light chain amyloidosis (off-label use): Oral: 15 mg once daily for 21 days of a 28-day cycle (in combination with dexamethasone) (Nair 2012; Sanchorawala 2007).
Dosing: Geriatric
Refer to adult dosing. Due to the potential for decreased renal function in the elderly, select dose carefully and closely monitor renal function.
Dosing: Adjustment for Toxicity
Nonhematologic toxicities:
Dermatologic toxicities:
Skin rash, grade 2 or 3: Consider interrupting or discontinuing treatment.
Angioedema, anaphylaxis, grade 4 rash, exfoliative or bullous rash, or other severe dermatologic reactions such as suspected Stevens-Johnson syndrome, toxic epidermal necrolysis, or drug reaction with eosinophilia and systemic symptoms: Permanently discontinue treatment.
Tumor flare reaction:
Grade 1 or 2: Continue therapy at physician's discretion; may consider symptom management with corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs) and/or analgesic therapy.
Grade 3 or 4: Interrupt therapy until resolved to ≤ grade 1; consider symptom management with corticosteroids, NSAIDs and/or analgesic therapy.
Other toxicities: For additional treatment-related grade 3/4 toxicities, hold treatment and restart (if appropriate) at next lower dose level when toxicity has resolved to ≤ grade 2.
Hematologic toxicities:
Follicular lymphoma and marginal zone lymphoma:
Platelets <50,000/mm3: Hold treatment, check CBC weekly.
When platelets return to ≥50,000/mm3: Resume treatment at 5 mg below previous dose. If starting dose was 20 mg/day, do not dose below 5 mg daily; if starting dose was 10 mg/day, do not dose below 2.5 mg daily.
ANC <1,000/mm3 for at least 7 days or associated with fever (≥38.5°C [101°F]): Hold treatment, check CBC weekly.
ANC <500/mm3: Hold treatment, check CBC weekly.
When ANC returns to ≥1,000/mm3: Resume treatment at 5 mg below previous dose. If starting dose was 20 mg/day, do not dose below 5 mg daily; if starting dose was 10 mg/day, do not dose below 2.5 mg daily.
Mantle cell lymphoma:
Platelets <50,000/mm3: Hold treatment, check CBC weekly.
When platelets return to ≥50,000/mm3: Resume treatment at 5 mg below previous dose; do not dose below 5 mg daily.
ANC <1,000/mm3 for at least 7 days or associated with fever (≥38.5°C [101°F]): Hold treatment, check CBC weekly.
ANC <500/mm3: Hold treatment, check CBC weekly.
When ANC returns to ≥1,000/mm3: Resume treatment at 5 mg below previous dose; do not dose below 5 mg daily.
Multiple myeloma:
Combination therapy with dexamethasone:
Platelets <30,000/mm3: Hold treatment, check CBC weekly.
When platelets return to ≥30,000/mm3: Resume at next lower dose; do not dose below 2.5 mg daily.
For each additional occurrence of platelets <30,000/mm3: Hold treatment.
When platelets return to ≥30,000/mm3: Resume treatment at next lower dose; do not dose below 2.5 mg daily.
ANC <1,000/mm3: Hold treatment, check CBC weekly.
When ANC returns to ≥1,000/mm3 (with neutropenia as only toxicity): Resume at 25 mg daily or initial starting dose.
When ANC returns to ≥1,000/mm3 (with additional toxicities): Resume at next lower dose; do not dose below 2.5 mg daily.
For each additional occurrence of ANC <1,000/mm3: Hold treatment.
When ANC returns to ≥1,000/mm3: Resume treatment at next lower dose; do not dose below 2.5 mg daily.
Maintenance following autologous stem cell transplant:
Platelets <30,000/mm3: Hold treatment, check CBC weekly.
When platelets return to ≥30,000/mm3: Resume at next lower dose; maintain continuous daily dosing.
Additional occurrence of platelets <30,000/mm3 (and current dose is 5 mg once daily): Hold treatment.
When platelets return to ≥30,000/mm3 (and current dose is 5 mg once daily): Resume treatment at 5 mg daily on days 1 to 21 of a 28-day cycle; do not dose below 5 mg daily on days 1 to 21 of a 28-day cycle.
ANC <500/mm3: Hold treatment, check CBC weekly.
When ANC returns to ≥500/mm3: Resume at next lower dose; maintain continuous daily dosing.
Subsequent occurrence of ANC <500/mm3 (and current dose is 5 mg daily): Hold treatment.
When ANC returns to ≥500/mm3: Resume treatment at 5 mg daily on days 1 to 21 of a 28-day cycle; do not dose below 5 mg daily on days 1 to 21 of a 28-day cycle.
Myelodysplastic syndromes:
Thrombocytopenia developing within 4 weeks of beginning treatment at 10 mg daily:
Baseline platelets ≥100,000/mm3:
If platelets <50,000/mm3: Hold treatment.
When platelets return to ≥50,000/mm3: Resume treatment at 5 mg daily.
Baseline platelets <100,000/mm3:
If platelets fall to 50% of baseline: Hold treatment.
If baseline ≥60,000/mm3 and platelet level returns to ≥50,000/mm3: Resume at 5 mg daily.
If baseline <60,000/mm3 and platelet level returns to ≥30,000/mm3: Resume at 5 mg daily.
Thrombocytopenia developing after 4 weeks of beginning treatment at 10 mg daily:
Platelets <30,000/mm3or <50,000/mm3 with platelet transfusions: Hold treatment.
When platelets return to ≥30,000/mm3 (without hemostatic failure): Resume at 5 mg daily.
Thrombocytopenia developing during treatment at 5 mg daily:
Platelets <30,000/mm3or <50,000/mm3 with platelet transfusions: Hold treatment.
When platelets return to ≥30,000/mm3 (without hemostatic failure): Resume at 2.5 mg once daily.
Neutropenia developing within 4 weeks of beginning treatment at 10 mg daily:
For baseline ANC ≥1,000/mm3:
ANC <750/mm3: Hold treatment.
When ANC returns to ≥1,000/mm3: Resume at 5 mg daily.
For baseline ANC <1,000/mm3:
ANC <500/mm3: Hold treatment.
When ANC returns to ≥500/mm3: Resume at 5 mg daily.
Neutropenia developing after 4 weeks of beginning treatment at 10 mg daily:
ANC <500/mm3 for ≥7 days or associated with fever (≥38.5°C [101°F]): Hold treatment.
When ANC returns to ≥500/mm3: Resume at 5 mg daily.
Neutropenia developing during treatment at 5 mg daily:
ANC <500/mm3 for ≥7 days or associated with fever (≥38.5°C [101°F]): Hold treatment.
When ANC returns to ≥500/mm3: Resume at 2.5 mg once daily.
Administration
Administer at about the same time each day with water; administer with or without food. Swallow capsule whole; do not break, open, or chew.
Missed doses: May administer a missed dose if within 12 hours of usual dosing time. If greater than 12 hours, patient should skip dose for that day and resume usual dosing the following day. Patient should not take 2 doses to make up for a missed dose.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C and 30°C (59°F and 86°F).
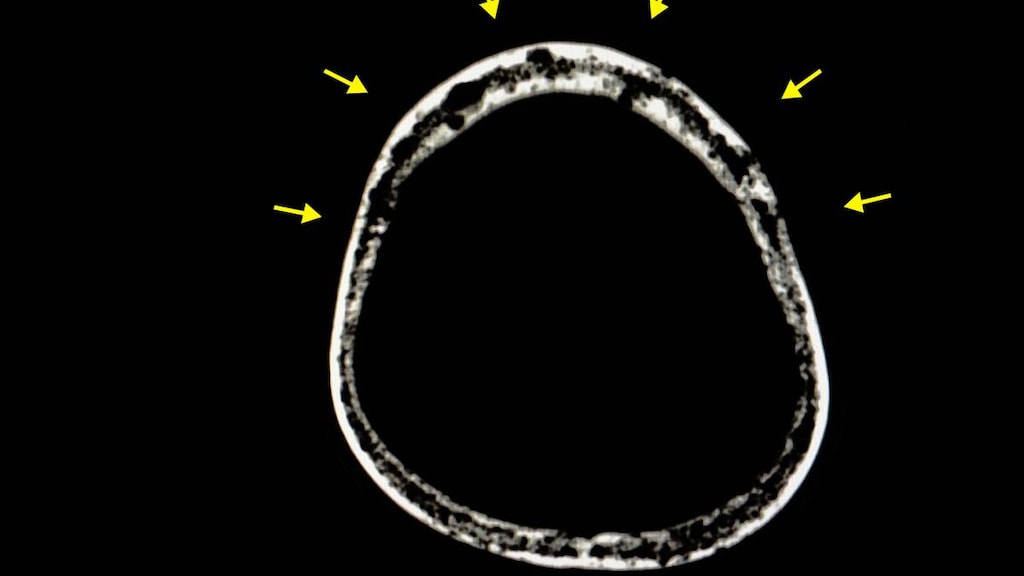
Lenalidomide Images
Drug Interactions
Abatacept: Anti-TNF Agents may enhance the adverse/toxic effect of Abatacept. An increased risk of serious infection during concomitant use has been reported. Avoid combination
Anakinra: Anti-TNF Agents may enhance the adverse/toxic effect of Anakinra. An increased risk of serious infection during concomitant use has been reported. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bisphosphonate Derivatives: Angiogenesis Inhibitors (Systemic) may enhance the adverse/toxic effect of Bisphosphonate Derivatives. Specifically, the risk for osteonecrosis of the jaw may be increased. Monitor therapy
Canakinumab: Anti-TNF Agents may enhance the adverse/toxic effect of Canakinumab. Specifically, the risk for serious infections and/or neutropenia may be increased. Avoid combination
Certolizumab Pegol: Anti-TNF Agents may enhance the immunosuppressive effect of Certolizumab Pegol. Avoid combination
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
DexAMETHasone (Systemic): May enhance the thrombogenic effect of Lenalidomide. Consider therapy modification
Digoxin: Lenalidomide may increase the serum concentration of Digoxin. Monitor therapy
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Erythropoiesis-Stimulating Agents: May enhance the thrombogenic effect of Lenalidomide. Monitor therapy
Estrogen Derivatives: May enhance the thrombogenic effect of Lenalidomide. Monitor therapy
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Pembrolizumab: May enhance the adverse/toxic effect of Thalidomide Analogues. Specifically, mortality may be increased when this combination is used for treatment of refractory multiple myeloma. Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Rilonacept: Anti-TNF Agents may enhance the adverse/toxic effect of Rilonacept. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Smallpox and Monkeypox Vaccine (Live): Immunosuppressants may diminish the therapeutic effect of Smallpox and Monkeypox Vaccine (Live). Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tocilizumab: May enhance the immunosuppressive effect of Anti-TNF Agents. Avoid combination
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Exceptions: Smallpox and Monkeypox Vaccine (Live). Avoid combination
Vedolizumab: Anti-TNF Agents may enhance the adverse/toxic effect of Vedolizumab. Avoid combination
Adverse Reactions
May vary based on indication.
>10%:
Cardiovascular: Peripheral edema (16% to 20%)
Central nervous system: Fatigue (11% to 34%), dizziness (20%), headache (9% to 20%), paresthesia (13%)
Dermatologic: Pruritus (MDS: 42%; MCL: 17%), skin rash (8% to 36%), xeroderma (≤11%)
Endocrine & metabolic: Weight loss (13%), hypokalemia (7% to 13%)
Gastrointestinal: Diarrhea (MM maintenance, MDS: 39% to 49%; MCL: 31%), nausea (11% to 30%), constipation (13% to 24%), gastroenteritis (23%), decreased appetite (14%), abdominal pain (10% to 12%), vomiting (6% to 12%)
Genitourinary: Urinary tract infection (4% to 11%)
Hematologic & oncologic: Thrombocytopenia (24% to 62%; grades 3/4: 13% to 50%), neutropenia (49% to 61%; grades 3/4: 43% to 54%), leukopenia (8% to 32%; grades 3/4: 5% to 24%), anemia (MCL: 31%, grades 3/4: 11%, MDS, MM maintenance: 9% to 12%, grades 3/4: 4% to 6%)
Infection: Influenza (13%)
Neuromuscular & skeletal: Muscle spasm (MM maintenance: 33%; MCL: 13%), asthenia (14% to 30%), arthralgia (MDS: 22%; MCL: 8%), back pain (13% to 21%), muscle cramps (18%), limb pain (11%)
Respiratory: Bronchitis (MM: 44%; MDS: 6%), nasopharyngitis (≤35%), cough (20% to 28%), pneumonia (12% to 17%), dyspnea (6% to 17%; includes exacerbation), pharyngitis (16%), epistaxis (15%), upper respiratory tract infection (11% to 15%), rhinitis (7% to 15%), sinusitis (≤14%)
Miscellaneous: Fever (21% to 23%; may be intermittent)
1% to 10%:
Cardiovascular: Edema (10%), hypotension (7%), hypertension (6%), chest pain (5%), palpitations (5%), deep vein thrombosis (2% to 4%), pulmonary embolism (1% to 2%), cardiac failure
Central nervous system: Insomnia (10%), peripheral neuropathy (5% to 10%), hypoesthesia (7%), pain (7%), myasthenia (6%), rigors (6%), chills, lethargy, vertigo
Dermatologic: Night sweats (8%), diaphoresis (7%), ecchymoses (5%), erythema of skin (5%), cellulitis (2% to 5%)
Endocrine & metabolic: Dehydration (7%), hypothyroidism (7%), hypomagnesemia (6%), hypocalcemia (3%), hyponatremia (2%)
Gastrointestinal: Anorexia (10%), upper abdominal pain (7% to 8%), xerostomia (7%), dysgeusia (6%), loose stools (6%), oral herpes simplex infection
Genitourinary: Dysuria (7%), urolithiasis (ureter)
Hematologic & oncologic: Tumor flare (10%), bruise (8%), lymphocytopenia (4% to 7%; grades 3/4: 4%), febrile neutropenia (2% to 6%; grades 3/4: 2% to 6%), pancytopenia (4%; grades 3/4: 2%), squamous cell carcinoma of skin (3%), granulocytopenia (grades 3/4: 2%), myelodysplastic syndrome (≤1%)
Hepatic: Increased serum alanine aminotransferase (8%), hyperbilirubinemia (1%)
Hypersensitivity: Hypersensitivity reaction
Infection: Herpes zoster infection (10%), infection (6%), sepsis (1% to 2%; including enterobacter, klebsiella, staphylococcus), bacteremia (1%)
Neuromuscular & skeletal: Myalgia (7% to 9%), swelling of extremities (8%), musculoskeletal pain (7%)
Renal: Renal failure syndrome (4%)
Respiratory: Oropharyngeal pain (10%), dyspnea on exertion (7%), pleural effusion (7%), rhinorrhea (5%), pulmonary infection (3%), hypoxia (2%), respiratory distress (1%), respiratory tract infection
Miscellaneous: Physical health deterioration (2%), troponin increased in blood specimen (troponin I)
Frequency not defined:
Cardiovascular: Acute myocardial infarction, angina pectoris, arterial thromboembolism, atrial fibrillation (including exacerbation), bradycardia, cardiac disorder (aortic disorder), cardiogenic shock, cardiomyopathy, cerebral infarction, cerebrovascular accident, ischemia, ischemic heart disease, septic shock, subarachnoid hemorrhage, superficial thrombophlebitis, supraventricular cardiac arrhythmia, supraventricular tachycardia, tachyarrhythmia, thrombosis, transient ischemic attacks, venous thromboembolism, ventricular dysfunction
Central nervous system: Abnormal gait, aphasia, cerebellar infarction, confusion, depression, dysarthria, falling, impaired consciousness, migraine, spinal cord compression
Dermatologic: Erythema multiforme, erythematous rash, exfoliative dermatitis, follicular rash, macular eruption, maculopapular rash, papular rash, pruritic rash, pustular rash, Sweet's syndrome
Endocrine & metabolic: Gout, gouty arthritis, Graves' disease, hypernatremia, hypoglycemia
Gastrointestinal: Biliary obstruction, cholecystitis (may be acute), Clostridioides difficile associated diarrhea, Clostridioides difficile colitis, colonic polyps, diverticulitis of the gastrointestinal tract, dysphagia, gastritis, gastrointestinal hemorrhage, gastrointestinal pain, gastrointestinal reflux disease, infection of mouth, inguinal hernia (obstructive), intestinal obstruction (small intestine), intestinal perforation, irritable bowel syndrome, ischemic colitis, lower abdominal pain, melena, pancreatitis
Genitourinary: Abscess of rectum and/or peri-rectal area, azotemia, hematuria, pelvic pain, urinary tract infection with sepsis
Hematologic & oncologic: Acquired blood coagulation disorder, acute leukemia, basal cell carcinoma of skin, bone marrow depression, bronchogenic carcinoma, decreased hemoglobin, hemolysis, hemolytic anemia, malignant lymphoma, malignant neoplasm of lung, myeloid leukemia (acute), postprocedural hemorrhage, progression of cancer, prostate carcinoma, rectal hemorrhage, splenic infarction, warm antibody immunohemolytic anemia
Hepatic: Abnormal hepatic function tests (may be transient), hepatic failure
Hypersensitivity: Transfusion reaction
Infection: Fungal infection, herpes virus infection, kidney infection, localized infection, pseudomonas infection, staphylococcal infection
Local: Catheter infection
Neuromuscular & skeletal: Arthritis (including exacerbation), bone fracture (femur, femoral neck, pelvis, hip, rib, spinal compression), calcium pyrophosphate deposition disease, neck pain
Otic: Otic infection
Renal: Acute renal failure, increased serum creatinine
Respiratory: Acute sinusitis, chronic obstructive pulmonary disease (includes exacerbation), interstitial pulmonary disease, lobar pneumonia, pulmonary edema, pulmonary infiltrates, respiratory failure, wheezing
Miscellaneous: Accidental injury (traffic accident), mass (renal), nodule
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, cholestatic hepatitis, drug reaction with eosinophilia and systemic symptoms, graft versus host disease, hematologic disease (impaired stem cell mobilization), hepatic cytolysis, hyperthyroidism, organ transplant rejection, pneumonitis, progressive multifocal leukoencephalopathy, reactivation of HPV, Stevens-Johnson syndrome, toxic epidermal necrolysis, toxic hepatitis, tumor lysis syndrome
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: [US Boxed Warning]: Hematologic toxicity (neutropenia and thrombocytopenia) occurs in a majority of patients (grade 3/4: 80% in patients with del 5q myelodysplastic syndrome) and may require dose reductions and/or delays; the use of blood product support and/or growth factors may be needed. CBC should be monitored weekly for the first 8 weeks and at least monthly thereafter in patients being treated for del 5q myelodysplastic syndromes. In patients being treated for multiple myeloma, monitor CBC weekly for the first 2 cycles, every 2 weeks during cycle 3, and monthly thereafter. In patients receiving lenalidomide for mantle cell lymphoma, monitor CBC weekly for the first cycle, every 2 weeks during cycles 2 to 4, and monthly thereafter. Monitor CBC weekly for the first 3 weeks in cycle 1 and every 2 weeks in cycles 2 to 4, and monthly thereafter in patients with follicular and marginal zone lymphoma. Monitor for signs of infection, bleeding, or bruising; may require dosage adjustment.
- CNS effects: May cause dizziness or fatigue; caution patients about performing tasks that require mental alertness (eg, operating machinery, driving).
- Dermatologic reactions: Severe cutaneous reactions, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS), have been reported; may be fatal. DRESS may manifest as a cutaneous reaction (eg, rash, exfoliative dermatitis), eosinophilia, fever, and/or lymphadenopathy with systemic complications, which may include hepatitis, nephritis, pneumonitis, myocarditis, and/or pericarditis. Consider interrupting or discontinuing treatment with grade 2 or 3 skin rash; permanently discontinue treatment with grade 4 rash, exfoliative or bullous rash, or for other severe cutaneous reactions such as suspected SJS, TEN, or DRESS. Patients with a history of grade 4 rash with thalidomide should not receive lenalidomide.
- Hepatotoxicity: Hepatic failure, including fatalities, has occurred in patients treated with combination lenalidomide and dexamethasone therapy; may have hepatocellular, cholestatic, or mixed characteristics. Risk factors may include preexisting viral liver disease, elevated liver enzymes at baseline, and concomitant medications. Monitor closely; interrupt therapy in patients with abnormal hepatic function tests. May consider resuming treatment at a lower dose upon return to baseline.
- Hypersensitivity: Hypersensitivity, including angioedema and anaphylactic reactions, have been reported. Permanently discontinue for angioedema or anaphylaxis.
- Secondary malignancy: Second primary malignancies (SPMs), including hematologic (primarily AML and MDS) and solid tumor malignancies, and non-melanoma skin cancers, have been reported with lenalidomide when used for the treatment of MDS and multiple myeloma; the incidence may be higher when lenalidomide is used in combination with an alkylating agent. Monitor for development of secondary malignancies.
- Thromboembolic events: [US Boxed Warning]: Lenalidomide has been associated with a significant increase in risk for arterial and venous thromboembolic events in multiple myeloma patients treated with lenalidomide and dexamethasone combination therapy. Deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction, and stroke have occurred; monitor for signs and symptoms of thromboembolism (shortness of breath, chest pain, or arm or leg swelling) and instruct patients to seek prompt medical attention with development of these symptoms. Thromboprophylaxis is recommended; the choice of regimen should be based on an assessment of the patient's underlying risk factors. The American Society of Clinical Oncology guidelines for VTE prophylaxis and treatment recommend thromboprophylaxis for patients receiving lenalidomide in combination with chemotherapy and/or dexamethasone; either aspirin or low molecular weight heparin (LMWH) is recommended for lower risk patients and LMWH is recommended for higher-risk patients (Lyman 2013; Lyman 2015). Erythropoietin-stimulating agents (ESAs) and estrogens may contribute to thromboembolic risk; use with caution. Patients with a prior history of arterial thromboembolic events may be at greater risk; minimize modifiable factors such as hyperlipidemia, hypertension, and smoking. Anticoagulant prophylaxis should be individualized and selected based on the thromboembolism risk of the combination treatment regimen, using the safest and easiest to administer (Palumbo 2008).
- Thyroid disorders: Both hypothyroidism and hyperthyroidism have been reported with lenalidomide use; monitor thyroid function prior to therapy initiation and periodically throughout treatment.
- Tumor flare: Observed in studies of lenalidomide for the treatment of chronic lymphocytic leukemia (CLL) and lymphomas; clinical presentation includes low grade fever, pain, rash, and tender lymph node swelling. In patients with mantle cell lymphoma, follicular lymphoma, and/or marginal zone lymphoma, tumor flare may mimic disease progression; monitor closely. In clinical trials, the majority of tumor flare events occurred in the first cycle of therapy. Treatment with corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and/or analgesics may be considered; therapy interruption may be necessary as well.
- Tumor lysis syndrome: Tumor lysis syndrome (with fatalities) has been reported with lenalidomide. Patients with a high tumor burden may be at risk for tumor lysis syndrome; monitor closely; institute appropriate management for hyperuricemia.
Disease-related concerns:
- Heart failure: In a scientific statement from the American Heart Association, lenalidomide has been determined to be an agent that may either cause direct myocardial toxicity or exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]).
- Mantle cell lymphoma: An increased incidence of early deaths (within 20 weeks) was reported in one study of patients receiving lenalidomide for the treatment of mantle cell lymphoma. Risk factors for early death include high tumor burden, mantle cell lymphoma international prognostic index (MIPI) score at diagnosis, and high WBC count (≥10,000/mm3) at baseline.
- Multiple myeloma: An increase in mortality was noted in 2 clinical studies in patients with multiple myeloma who received pembrolizumab in combination with a thalidomide analogue and dexamethasone. Causes of death in the experimental arm (containing pembrolizumab, dexamethasone, and a thalidomide analogue [pomalidomide or lenalidomide]) included myocarditis, Stevens-Johnson syndrome, MI, pericardial hemorrhage, cardiac failure, respiratory tract infection, neutropenic sepsis, sepsis, multiple organ dysfunction, respiratory failure, intestinal ischemia, cardiopulmonary arrest, suicide, pulmonary embolism, cardiac arrest, pneumonia, sudden death, and large intestine perforation. Multiple myeloma is not an approved indication for PD-1 or PD-L1 blocking antibodies; pembrolizumab should not be used to treat multiple myeloma in combination with a thalidomide analogue and dexamethasone unless as part of a clinical trial.
- Renal impairment: Use with caution in patients with renal impairment; may experience an increased rate of toxicities due to reduced clearance and increased half-life. Initial dosage adjustments are recommended for moderate to severe and dialysis-dependent renal impairment.
- Stem cell mobilization: Lenalidomide use (≥4 cycles) may decrease the number of CD34+ cells collected for autologous stem cell transplant. Transplant eligible patients receiving lenalidomide should be referred to an appropriate transplant center in order to optimize the timing of stem cell collection. Cyclophosphamide in combination with G-CSF or G-CSF in combination with a CXC chemokine receptor 4 inhibitor (eg, plerixafor) may be considered when CD34+ cell collection is impaired.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Certain adverse reactions (DVT, pulmonary embolism, atrial fibrillation, renal failure) are more likely in elderly patients; in some studies, the incidence of grade 3 or 4 adverse reactions was higher in elderly patients. Monitor renal function closely, and select dose accordingly.
- Pediatric: If used in patients between 12 to 18 years of age, the parent or legal guardian must agree to ensure compliance with the Revlimid REMS program.
- Pregnancy: [US Boxed Warning]: Do not use lenalidomide in pregnant females. Lenalidomide is an analogue of thalidomide (a human teratogen) and could potentially cause severe birth defects or embryo-fetal death; use is contraindicated during pregnancy and pregnancy must be avoided while taking lenalidomide. Obtain 2 negative pregnancy tests prior to initiation of treatment; 2 forms of contraception (or abstain from heterosexual intercourse) must be used at least 4 weeks prior to, during and for 4 weeks after lenalidomide treatment (and during treatment interruptions). In order to decrease the risk of embryo-fetal exposure, lenalidomide is available only through a restricted distribution program (Revlimid REMS). Males taking lenalidomide (even those vasectomized) must use a latex or synthetic condom during any sexual contact with females of reproductive potential and for up to 28 days following discontinuation of therapy. Males taking lenalidomide must not donate sperm.
Other warnings/precautions:
- Appropriate use: In a clinical trial comparing lenalidomide versus chlorambucil single agent therapy in patients >65 years of age with chronic lymphocytic leukemia patients (not an FDA-approved indication), increased mortality was observed in the lenalidomide treatment arm. Atrial fibrillation, cardiac failure, and MI were observed more frequently in lenalidomide-treated patients; lenalidomide (alone or in combination) is not currently recommended for first-line treatment of CLL.
- REMS program: Due to the embryo-fetal risk, lenalidomide is only available through a restricted program under the Revlimid REMS program. Prescribers and pharmacies must be certified with the program to prescribe or dispense lenalidomide. Lenalidomide should only be prescribed to patients (male and female) who can understand and comply with the conditions of the Revlimid REMS program.
- Blood donation: Patients should be advised not to donate blood during therapy and for 1 month following completion of therapy.
- Lactose intolerance: Product may contain lactose; avoid use in patients with Lapp lactase deficiency, glucose-galactose malabsorption, or glucose intolerance.
Monitoring Parameters
CBC with differential (MCL - weekly for the first cycle, every 2 weeks during cycles 2 to 4; MDS - weekly for first 8 weeks; Multiple myeloma - weekly for the first 2 cycles, every 2 weeks during the third cycle; follicular and marginal zone lymphoma – weekly for the first 3 weeks in cycle 1 and every 2 weeks in cycles 2 to 4), then monthly thereafter; serum creatinine, liver function tests, thyroid function tests (TSH at baseline then every 2 to 3 months during lenalidomide treatment [Hamnvik 2011]); ECG when clinically indicated; monitor for signs and symptoms of infection (if neutropenic), secondary malignancies, thromboembolism, dermatologic toxicity, tumor lysis syndrome, or tumor flare reaction.
Females of reproductive potential: Pregnancy test 10 to 14 days and 24 hours prior to initiating therapy, weekly during the first 4 weeks of treatment, then every 2 to 4 weeks through 4 weeks after therapy discontinued.
Monitor adherence.
Pregnancy
Pregnancy Considerations
Use is contraindicated in pregnancy. [US Boxed Warning]: Do not use lenalidomide during pregnancy. Lenalidomide, a thalidomide analogue, caused limb abnormalities in a developmental monkey study. Thalidomide is a known human teratogen that causes severe, life-threatening human birth defects. If lenalidomide is used during pregnancy, it may cause birth defects or embryo-fetal death. In females of reproductive potential, obtain two negative pregnancy tests before starting lenalidomide treatment. Females of reproductive potential must use two forms of contraception or continuously abstain from heterosexual sex during and for 4 weeks after lenalidomide treatment. To avoid embryo-fetal exposure to lenalidomide, it is only available under a restricted distribution program called Revlimid REMS program.
Females of reproductive potential should be treated only if they are able to comply with the conditions of the Revlimid REMS program. Females of reproductive potential must avoid pregnancy beginning 4 weeks prior to therapy, during therapy, during therapy interruptions, and for at least 4 weeks after therapy is discontinued. Two forms of effective/reliable contraception (eg, tubal ligation, IUD, hormonal birth control methods, male latex or synthetic condom, diaphragm, or cervical cap) or total abstinence from heterosexual intercourse must be used by females who are not infertile or who have not had a hysterectomy. A negative pregnancy test (sensitivity of at least 50 milliunits/mL) 10 to 14 days prior to therapy, within 24 hours prior to beginning therapy, weekly during the first 4 weeks, and every 4 weeks (every 2 weeks for females with irregular menstrual cycles) thereafter is required for females of reproductive potential. Lenalidomide must be immediately discontinued for a missed period, abnormal pregnancy test or abnormal menstrual bleeding; refer patient to a reproductive toxicity specialist if pregnancy occurs during treatment.
Lenalidomide is also present in the semen of males. Males (including those vasectomized) should use a latex or synthetic condom during any sexual contact with females of reproductive age during treatment, during treatment interruptions, and for 4 weeks after discontinuation. Male patients should not donate sperm during, and for 4 weeks after treatment, and during therapy interruptions.
A pregnancy exposure registry has been created to monitor outcomes in females exposed to lenalidomide during pregnancy and female partners of male patients and to understand the root cause for the pregnancy. The pregnancy exposure registry may be contacted at 1-888-423-5436. The parent or legal guardian for patients between 12 and 18 years of age must agree to ensure compliance with the required guidelines. Any suspected fetal exposure should be reported to the FDA via the MedWatch program (1-800-FDA-1088) and to Celgene Corporation (1-888-423-5436).
Patient Education
What is this drug used for?
- It is used to treat multiple myeloma and lymphoma and a health problem called myelodysplastic syndrome (MDS). It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Back pain
- Bone pain
- Diarrhea
- Sweating a lot
- Common cold symptoms
- Stuffy nose
- Sore throat
- Flu-like signs
- Change in taste
- Trouble sleeping
- Constipation
- Nausea
- Vomiting
- Abdominal pain
- Muscle pain
- Heartburn
- Tremors
- Lack of appetite
- Weight loss
- Joint pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
- Heart attack like chest pain; pain in arms, back, neck, jaw, or abdomen; shortness of breath; cold sweats; severe dizziness; passing out; or severe nausea or vomiting
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Tumor lysis syndrome like fast heartbeat or abnormal heartbeat; any passing out; trouble passing urine; muscle weakness or cramps; nausea, vomiting, diarrhea, or lack of appetite; or feel sluggish
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any bleeding that is very bad or that will not stop
- Thyroid problems like change in weight without trying, anxiety, agitation, feeling very weak, hair thinning, depression, neck swelling, difficulty focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting
- Dehydration like dry skin, dry mouth, dry eyes, increased thirst, fast heartbeat, dizziness, fast breathing, or confusion
- Burning or numbness feeling
- Edema
- Depression
- Severe headache
- Severe dizziness
- Passing out
- Severe loss of strength and energy
- Swollen glands
- Vision changes
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.