Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
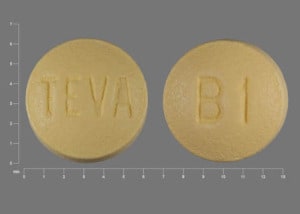
Tablet, Oral:
Femara: 2.5 mg
Generic: 2.5 mg
Pharmacology
Mechanism of Action
Letrozole is a nonsteroidal competitive inhibitor of the aromatase enzyme system which binds to the heme group of aromatase, a cytochrome P450 enzyme which catalyzes conversion of androgens to estrogens (specifically, androstenedione to estrone and testosterone to estradiol). This leads to inhibition of the enzyme and a significant reduction in plasma estrogen (estrone, estradiol and estrone sulfate) levels. Letrozole does not appear to affect synthesis of adrenal or thyroid hormones, aldosterone, or androgens.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and well absorbed; not affected by food
Distribution
Vd: ~1.9 L/kg
Metabolism
Hepatic via CYP3A4 and 2A6 to an inactive carbinol metabolite
Excretion
Urine (~90%; 6% as unchanged drug, 75% as glucuronide carbinol metabolite, 9% as unidentified metabolites)
Time to Peak
Steady state, plasma: 2 to 6 weeks; steady state serum concentrations are 1.5 to 2 times higher than single-dose values. In girls 3 to 9 years, steady state concentrations were 25% to 67% that of the mean adult values (Feuillan 2007)
Half-Life Elimination
Terminal: ~2 days
Protein Binding
Plasma: Weak
Use in Specific Populations
Special Populations: Hepatic Function Impairment
AUC was 37% higher in patients with mild to moderate hepatic impairment (Child-Pugh class A and B). AUC was increased 2-fold and systemic clearance was reduced 47% in patients with severe hepatic impairment (Child-Pugh class C).
Use: Labeled Indications
Breast cancer in postmenopausal women: Adjuvant treatment of hormone receptor-positive early breast cancer, extended adjuvant treatment of early breast cancer after 5 years of tamoxifen; treatment of advanced breast cancer with disease progression following antiestrogen therapy; first-line treatment of hormone receptor-positive or hormone receptor-unknown, locally-advanced, or metastatic breast cancer
Use: Off Label
Infertility/Ovulation stimulation in anovulatory females with polycystic ovary syndromebyes
Two meta-analyses of randomized, placebo-controlled studies suggest letrozole is superior to clomiphene for ovulation induction in subfertile females with polycystic ovary syndrome (PCOS). A greater increase in ovulation rate, clinical pregnancy rate, and live birth rate was observed with letrozole compared to clomiphene; complications were not found to differ between treatments Franik 2018, Hu 2018.
Based on the American College of Obstetricians and Gynecologists guidelines and an international guideline published by the Australian National Health and Medical Research Council in partnership with the American Society of Reproductive Medicine and the European Society of Human Reproductions and Embryology, letrozole is the preferred first-line pharmacologic treatment for ovulation induction in females with PCOS and anovulatory infertility when no other causes of infertility are present
Ovarian (epithelial) cancer, recurrentb
Data from a small phase II study support the use of letrozole in the treatment of platinum- and taxane-resistant recurrent epithelial ovarian cancer Ramierz 2008. Additional trials may be necessary to further define the role of letrozole in this condition.
Contraindications
Hypersensitivity to letrozole or any component of the formulation; pregnancy
Canadian labeling: Additional contraindications (not in the US labeling): Hypersensitivity to other aromatase inhibitors; use in patients <18 years of age; premenopausal endocrine status; breastfeeding
Dosage and Administration
Dosing: Adult
Breast cancer, advanced (first- or second-line treatment): Females: Postmenopausal: Oral: 2.5 mg once daily; continue until tumor progression
Breast cancer, early (adjuvant treatment): Females: Postmenopausal: Oral: 2.5 mg once daily for a planned duration of 5 years; discontinue at relapse.
Duration of therapy: American Society of Clinical Oncology (ASCO) guidelines for Adjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer (Focused Update) recommend a maximum duration of 5 years of aromatase inhibitor therapy for postmenopausal women; aromatase inhibitors may be combined with tamoxifen for a total duration of up to 10 years of endocrine therapy. Refer to the guidelines for specific recommendations based on menopausal status and tolerability (Burstein 2014). Treatment with an additional 5 years of therapy (for a total of 10 years of aromatase inhibitor therapy) has demonstrated a significantly improved rate of disease-free survival and a decreased risk of disease recurrence and contralateral breast cancer (when compared to placebo), although overall survival was not significantly different between groups and bone-related adverse events occurred more frequently with letrozole versus placebo (Goss 2016).
Breast cancer, early (extended adjuvant treatment): Females: Postmenopausal: Oral: 2.5 mg once daily for a planned duration of 5 years (after 5 years of tamoxifen); discontinue at relapse. In clinical trials, letrozole was initiated within 3 months of discontinuing tamoxifen (Goss 2003; Jin 2012).
Duration of therapy: ASCO guidelines for Adjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer (Focused Update) recommend a maximum duration of 5 years of aromatase inhibitor therapy for postmenopausal women; aromatase inhibitors may be combined with tamoxifen for a total duration of up to 10 years of endocrine therapy. Refer to the guidelines for specific recommendations based on menopausal status and tolerability (Burstein 2014). Treatment with an additional 5 years of therapy (for a total of 10 years of aromatase inhibitor therapy) has demonstrated a significantly improved rate of disease-free survival and a decreased risk of disease recurrence and contralateral breast cancer (when compared to placebo), although overall survival was not significantly different between groups and bone-related adverse events occurred more frequently with letrozole versus placebo (Goss 2016). The decision to extend aromatase inhibitor therapy for an additional 5 years should include initial adjuvant therapy (tamoxifen versus an aromatase inhibitor) and an assessment of the risk of recurrence.
Breast cancer off-label combinations:
Breast cancer, advanced, estrogen receptor-positive, HER2-negative: Females: Postmenopausal: Oral: 2.5 mg once daily (in combination with palbociclib) until disease progression or unacceptable toxicity (Finn 2015) or 2.5 mg once daily (in combination with ribociclib) until disease progression or unacceptable toxicity (Hortobagyi 2016) or 2.5 mg once daily (in combination with abemaciclib) until disease progression or unacceptable toxicity (Goetz 2017)
Breast cancer, metastatic, hormone receptor-positive, HER2-positive: Females: Postmenopausal: Oral: 2.5 mg once daily (in combination with lapatinib) until disease progression or unacceptable toxicity (Johnston 2009)
Infertility/Ovulation stimulation in anovulatory females with polycystic ovary syndrome (PCOS) (off-label use): Oral: Initial dose: 2.5 mg once daily for 5 days, starting on day 3, 4, or 5 following menses or progestin induced bleed; may increase to 5 mg/day for 5 days in subsequent cycles if ovulation does not occur. Maximum dose: 7.5 mg/day (ACOG 194 2018; ACOG 738 2018; Legro 2014). Dosing for up to 5 cycles was used in 1 study (Legro 2014).
Ovarian (epithelial) cancer, recurrent (off-label use): Oral: 2.5 mg once daily; continue until disease progression or unacceptable toxicity (Ramirez 2008)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Delayed puberty and growth [CDGP (constitutional delay of growth and puberty)] (males): Very limited data available: Adolescents ≥14 years: Oral: 2.5 mg once daily in combination with testosterone therapy; dosing from a double-blind placebo-controlled trial of 33 adolescent males (treatment group: n=11); during the 12 months of therapy, bone maturation was delayed, predicted adult height values were significantly increased and markers of puberty progressed (Palmert; 2012; Wickman, 2001).
McCune-Albright syndrome; precocious puberty (females): Very limited data available: Children >2-10 years at time of treatment initiation: Oral: Initial: 0.5 mg/m2/day divided every 12 hours for days 1-7, then 1 mg/m2/day divided every 12 hours on days 8-14, then 1.5 mg/m2/day divided every 12 hours beginning on day 15; if needed, may further increase to 2 mg/m2/day if markers of precocious puberty including serum estradiol levels progress. Dosing based on a pilot study of nine girls (3-8 years at time of therapy initiation) which showed long-term therapy (up to 36 months) decreased rates of growth and bone maturation; although ovarian volume decreased during the first 6 months of treatment, the mean ovarian volume increased over 1-2 years of therapy with cyst redevelopment in some patients. During the pilot study, dosing was divided twice daily to alleviate GI discomfort; however, pharmacokinetic analysis showed once daily dosing would be appropriate for young children if tolerated (Feuillan, 2007). In a case series (n=3, age range at treatment: 3-7 years), a fixed dose of 2.5 mg once daily was used for 5-19 months duration (Bercaw-Pratt, 2012).
Short-stature; idiopathic (males): Limited data available: Children and Adolescents 9-16 years: Oral: 2.5 mg once daily; dosing based experience in a double-blind, placebo-controlled trial of 30 males (treatment group: n=16; age range: 9-14 years) and a retrospective observation (n=24; age range: 9-16 years); the duration of letrozole therapy was up to 2 years (range: 4-24 months); bone maturation delay with increases in predicted adult height values were observed with treatment (Hero, 2005; Karmazin, 2005; Shulman, 2008)
Administration
Oral: Administer without regard to meals.
Dietary Considerations
Calcium and vitamin D supplementation are recommended.
Storage
Store at room temperature of 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Letrozole Images
Drug Interactions
Levomethadone: Aromatase Inhibitors may increase the serum concentration of Levomethadone. Monitor therapy
Methadone: Aromatase Inhibitors may increase the serum concentration of Methadone. Monitor therapy
Tamoxifen: May decrease the serum concentration of Letrozole. Monitor therapy
Adverse Reactions
>10%:
Cardiovascular: Flushing (50%), edema (7% to 18%)
Central nervous system: Headache (4% to 20%), dizziness (3% to 14%), fatigue (10% to 13%)
Dermatologic: Diaphoresis (24%), night sweats (15%)
Endocrine & metabolic: Hypercholesterolemia (3% to 52%), hot flash (6% to 34%), weight gain (2% to 13%)
Gastrointestinal: Nausea (9% to 17%), constipation (2% to 11%)
Neuromuscular & skeletal: Weakness (4% to 34%), arthralgia (8% to 25%), arthritis (7% to 25%), ostealgia (5% to 22%), musculoskeletal pain (21%), back pain (5% to 18%), bone fracture (10% to 15%), osteoporosis (5% to 15%)
Respiratory: Dyspnea (6% to 18%), cough (6% to 13%)
1% to 10%:
Cardiovascular: Chest pain (6% to 8%), hypertension (5% to 8%), chest wall pain (6%), peripheral edema (5%), cerebrovascular accident (2% to 3%), thromboembolism (≤3%; including portal vein thrombosis, pulmonary embolism, thrombophlebitis, venous thrombosis), transient ischemic attacks (≤3%), angina pectoris (≤2%), hemorrhagic stroke (≤2%), ischemic heart disease (≤2%), thrombotic stroke (≤2%), cardiac failure (1% to 2%), myocardial infarction (1% to 2%)
Central nervous system: Insomnia (6% to 7%), pain (5%), anxiety (<5%), depression (<5%), vertigo (<5%), drowsiness (3%), hemiparesis (≤2%)
Dermatologic: Skin rash (5%), alopecia (<5%), pruritus (1%)
Endocrine & metabolic: Weight loss (6% to 7%), hypercalcemia (<5%)
Gastrointestinal: Diarrhea (5% to 8%), vomiting (3% to 7%), abdominal pain (6%), anorexia (1% to 5%), dyspepsia (3%)
Genitourinary: Mastalgia (2% to 7%), urinary tract infection (6%), vaginal dryness (5%), vaginal hemorrhage (5%), vaginal irritation (5%)
Hematologic & oncologic: Lymphedema (7%; post-mastectomy), second primary malignant neoplasm (2% to 5%)
Infection: Infection (7%), influenza (6%), viral infection (6%)
Neuromuscular & skeletal: Limb pain (4% to 10%), myalgia (7% to 9%), osteopenia (4%)
Ophthalmic: Cataract (2%)
Renal: Renal disease (5%)
Respiratory: Pleural effusion (<5%)
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, arterial thrombosis, blurred vision, carpal tunnel syndrome, dysesthesia, dysgeusia, endometrial carcinoma, endometrium disease, endometrial hyperplasia, erythema multiforme, eye irritation, fever, hepatitis, hypersensitivity reaction, increased appetite, increased liver enzymes, increased thirst, irritability, leukopenia, memory impairment, nervousness, ovarian cyst, palpitations, paresthesia, spontaneous abortion, stomatitis, tachycardia, tenosynovitis (trigger finger), thrombocytopenia, toxic epidermal necrolysis, urinary frequency, urticaria, vaginal discharge, xeroderma, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause dizziness, fatigue, and somnolence; patients should be cautioned before performing tasks which require mental alertness (eg, operating machinery or driving).
- Decreased bone mineral density: May cause decreases in bone mineral density (BMD). In one study, a decrease in hip BMD by 3.8% from baseline in letrozole-treated patients vs 2% in placebo at 2 years was demonstrated, however, while lumbar spine BMD was decreased, the difference was not statistically significant. Results of a safety study did demonstrate a decrease in lumbar spine BMD with letrozole (compared to tamoxifen). Osteoporosis and bone fractures have occurred at higher rates when compared to tamoxifen or to placebo. Monitor BMD.
- Increased cholesterol: May increase total serum cholesterol. In patients treated with adjuvant therapy and cholesterol levels within normal limits, an increase of ≥1.5 x ULN in total cholesterol (non-fasting) has been demonstrated in 8.2% of letrozole-treated patients (25% requiring lipid-lowering medications) vs 3.2% of tamoxifen-treated patients (16% requiring medications). Monitor cholesterol panel; may require antihyperlipidemics.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment; dose adjustment recommended in patients with cirrhosis or severe hepatic dysfunction.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Cholesterol, hepatic function tests; bone density; pregnancy test (prior to treatment in females of reproductive potential). Monitor adherence.
For infertility/ovarian stimulation (off-label use), a pregnancy test is recommended prior to initiation. Midluteal progestin concentrations (in a clinical study, nonresponse to treatment was defined as a progesterone concentration <3 ng/mL during the midluteal phase; poor ovulatory response was defined as progesterone concentrations indicating ovulation but just above the cutoff point) (Legro 2014).
Pregnancy
Pregnancy Considerations
Use is contraindicated in women with an established pregnancy.
Breast cancer: Letrozole is approved for the treatment of breast cancer in postmenopausal women. Based on the mechanism of action and data from animal reproduction studies, letrozole may cause fetal harm if used during pregnancy. A pregnancy test is recommended prior to letrozole therapy in women of reproductive potential and effective contraception should be used during letrozole therapy and for at least 3 weeks following the last letrozole dose.
Infertility associated with polycystic ovarian syndrome (PCOS): Letrozole is used off-label for ovulation induction in females with PCOS and anovulatory infertility when no other causes of infertility are present (ACOG 194 2018; ACOG 738 2018; Teede 2018). Baseline testing is done prior to letrozole therapy to rule out unexpected ovulation, which prevents exposure in early pregnancy (Legro 2016). Because information related to newborn outcomes following maternal use is limited, guidelines recommend counseling females of the off-label status prior to use (ACOG 194 2018; ACOG 738 2018).
Patient Education
What is this drug used for?
- It is used to treat breast cancer in women after change of life.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Loss of strength and energy
- Hot flashes
- Nausea
- Vomiting
- Cough
- Back pain
- Muscle pain
- Joint pain
- Constipation
- Diarrhea
- Night sweats
- Sweating a lot
- Trouble sleeping
- Weight loss
- Abdominal pain
- Hair loss
- Weight gain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Swollen glands
- Edema
- Chest pain
- Severe dizziness
- Passing out
- Shortness of breath
- Severe headache
- Vision changes
- Vaginal bleeding
- Depression
- Unable to pass urine
- Change in amount of urine passed
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.