Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet:
Stalevo 50: Levodopa 50 mg, carbidopa 12.5 mg, and entacapone 200 mg
Stalevo 75: Levodopa 75 mg, carbidopa 18.75 mg, and entacapone 200 mg
Stalevo 100: Levodopa 100 mg, carbidopa 25 mg, and entacapone 200 mg
Stalevo 125: Levodopa 125 mg, carbidopa 31.25 mg, and entacapone 200 mg
Stalevo 150: Levodopa 150 mg, carbidopa 37.5 mg, and entacapone 200 mg
Stalevo 200: Levodopa 200 mg, carbidopa 50 mg, and entacapone 200 mg
Generic: Levodopa 50 mg, carbidopa 12.5 mg, and entacapone 200 mg; Levodopa 75 mg, carbidopa 18.75 mg, and entacapone 200 mg; Levodopa 100 mg, carbidopa 25 mg, and entacapone 200 mg; Levodopa 125 mg, carbidopa 31.25 mg, and entacapone 200 mg; Levodopa 150 mg, carbidopa 37.5 mg, and entacapone 200 mg; Levodopa 200 mg, carbidopa 50 mg, and entacapone 200 mg
Pharmacology
Mechanism of Action
Levodopa: The metabolic precursor of dopamine, a chemical depleted in Parkinson's disease. Levodopa is able to circulate in the plasma and cross the blood-brain-barrier (BBB), where it is converted by striatal enzymes to dopamine.
Carbidopa: Inhibits the peripheral plasma breakdown of levodopa by inhibiting its decarboxylation; increases available levodopa at the BBB
Entacapone: A reversible and selective inhibitor of catechol-O-methyltransferase (COMT). Alters the pharmacokinetics of levodopa, resulting in more sustained levodopa serum levels and increased concentrations available for absorption across the BBB.
Pharmacokinetics/Pharmacodynamics
Metabolism
Levodopa: Two major pathways (decarboxylation and O-methylation) of metabolism; Carbidopa inhibits the decarboxylation of levodopa to dopamine in the peripheral tissue to allow greater levodopa distribution into the CNS; Entacapone: Isomerization to the cis-isomer, followed by direct glucuronidation of the parent and cis-isomer
Excretion
Levodopa: Urine (as metabolites); Carbidopa: Urine (30% as unchanged drug; also as metabolites); Entacapone: Feces (90%); urine (10%; <1% as unchanged drug)
Time to Peak
Levodopa: ~1 to 2 hours; Carbidopa: 2.5 to 3.4 hours; Entacapone: ~1 hour
Half-Life Elimination
Levodopa: 1.7 hours (range: 1.1 to 3.2 hours); Carbidopa: 1.6 to 2 hours (range ~1 to 4 hours); Entacapone: ~1 hour (range: 0.3 to 4.5 hours)
Protein Binding
Levodopa: ~10% to 30%; Carbidopa: ~36%; Entacapone: 98% (primarily to albumin
Use: Labeled Indications
Parkinson disease: Treatment of Parkinson disease.
Contraindications
Use of nonselective MAO inhibitor therapy with or within 14 prior days; narrow-angle glaucoma
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to levodopa, carbidopa, entacapone, or any component of the formulation; clinical or laboratory evidence of uncompensated cardiovascular, endocrine, hematologic, pulmonary (including bronchial asthma), or renal disease; history of neuroleptic malignant syndrome (NMS) and/or nontraumatic rhabdomyolysis; hepatic impairment; pheochromocytoma; when administration of a sympathomimetic amine is contraindicated; suspicious, undiagnosed skin lesions or a history of melanoma
Dosage and Administration
Dosing: Adult
Note: All strengths of Stalevo contain a carbidopa/levodopa ratio of 1:4 plus entacapone 200 mg.
Parkinson disease: Oral: Dose should be individualized based on therapeutic response; doses may be adjusted by changing strength or adjusting interval. Fractionated doses are not recommended and only 1 tablet should be given at each dosing interval; maximum daily dose: 8 tablets of Stalevo 50, 75, 100, 125, or 150, or 6 tablets of Stalevo 200. Patients receiving <70 to 100 mg of the carbidopa component may experience nausea and vomiting.
Patients previously treated with carbidopa/levodopa immediate release tablets (ratio of 1:4):
With current entacapone therapy: May switch directly to corresponding strength of combination tablet. No data available on transferring patients from controlled release preparations or products with a 1:10 ratio of carbidopa/levodopa.
Without entacapone therapy:
If current levodopa dose is >600 mg daily or history of moderate or severe dyskinesias: Levodopa dose reduction may be required when adding entacapone to therapy; therefore, titrate dose using individual products first (carbidopa/levodopa immediate release with a ratio of 1:4 plus entacapone 200 mg); then transfer to combination product once stabilized.
If current levodopa dose is <600 mg and without a history of dyskinesias: May transfer to corresponding dose of combination product; monitor, dose reduction of levodopa may be required.
Patients previously treated with benserazide/levodopa immediate release tablets [Canadian product]: With current entacapone therapy: Prior to switching to combination product (carbidopa/levodopa/entacapone), withhold treatment for 1 night, then initiate (carbidopa/levodopa/entacapone) therapy the following morning at a dose that provides either an equivalent amount or ~5% to 10% more levodopa.
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Swallow tablet whole; do not crush, break, or chew. Only 1 tablet should be administered at each dosing interval. May be administered without regard to meals; absorption may be delayed 2 hours if given with a high-fat, high-calorie meal.
Dietary Considerations
Distribute protein intake throughout the day to avoid fluctuations in levodopa absorption. Separate dosing of iron supplements and multivitamins with minerals.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
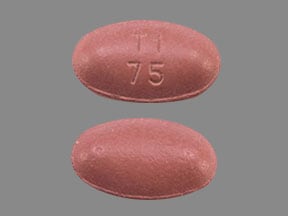
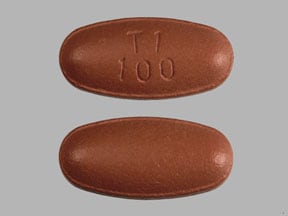
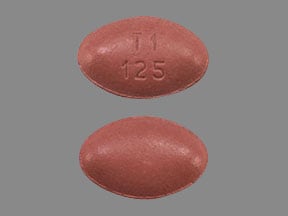
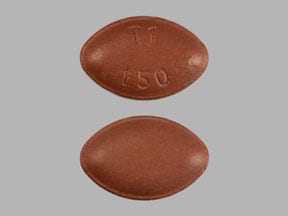
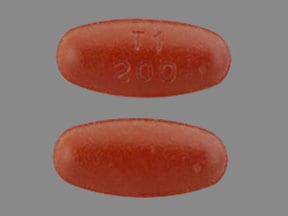
Levodopa, Carbidopa, and Entacapone Images
-
carbidopa/entacapone/levodopa 12.5 mg / 200 mg / 50 mg -
carbidopa/entacapone/levodopa 18.75 mg / 200 mg / 75 mg -
carbidopa/entacapone/levodopa 25 mg / 200 mg / 100 mg -
carbidopa/entacapone/levodopa 31.25 mg / 200 mg / 125 mg -
carbidopa/entacapone/levodopa 37.5 mg / 200 mg / 150 mg -
carbidopa/entacapone/levodopa 50 mg / 200 mg / 200 mg
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amisulpride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Amisulpride. Avoid combination
Antipsychotic Agents (First Generation [Typical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Antipsychotic Agents (First Generation [Typical]). Management: Avoid concomitant therapy if possible and monitor for decreased effects of both agents when these combinations cannot be avoided. Atypical antipsychotics such as clozapine and quetiapine may be less likely to reduce the effects of anti-Parkinson agents. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider using an alternative antipsychotic agent when possible in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine or quetiapine, which may convey the lowest interaction risk. Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Biperiden: May enhance the adverse/toxic effect of Levodopa-Containing Products. Specifically, the risk of choreic movements or dyskinesias may be increased. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BuPROPion: Anti-Parkinson Agents (Dopamine Agonist) may enhance the adverse/toxic effect of BuPROPion. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
COMT Substrates: COMT Inhibitors may decrease the metabolism of COMT Substrates. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Droxidopa: Carbidopa may diminish the therapeutic effect of Droxidopa. Carbidopa may decrease serum concentrations of the active metabolite(s) of Droxidopa. Carbidopa may increase the serum concentration of Droxidopa. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin-Phenytoin: May diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Glycopyrrolate (Systemic): May decrease the serum concentration of Levodopa-Containing Products. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Iron Preparations: May decrease the serum concentration of Levodopa. Only applies to oral iron preparations. Management: Consider separating doses of the agents by 2 or more hours to minimize the effects of this interaction. Monitor for decreased therapeutic effects of levodopa during concomitant therapy, particularly if doses cannot be separated. Exceptions: Ferric Carboxymaltose; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Iron Preparations: May decrease the serum concentration of Entacapone. Management: Consider separating doses of the agents by 2 or more hours to minimize the effects of this interaction. Monitor for decreased therapeutic effects of levodopa during concomitant therapy, particularly if doses cannot be separated. Exceptions: Ferric Carboxymaltose; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Isoniazid: May diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofepramine: Entacapone may enhance the adverse/toxic effect of Lofepramine. Avoid combination
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Macimorelin: Levodopa-Containing Products may diminish the diagnostic effect of Macimorelin. Avoid combination
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methionine: May diminish the therapeutic effect of Levodopa-Containing Products. Management: Avoid large daily doses of methionine in patients receiving levodopa (clinical studies showing interaction used 4.5 g methionine daily). More typical doses of methionine (eg, 500 mg) may not cause a problem. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: May enhance the adverse/toxic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Metoclopramide: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: Levodopa-Containing Products may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Of particular concern is the development of hypertensive reactions when levodopa is used with nonselective MAOI. Exceptions: Rasagiline; Safinamide; Selegiline. Avoid combination
Monoamine Oxidase Inhibitors: COMT Inhibitors may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Consider therapy modification
Multivitamins/Fluoride (with ADE): May diminish the therapeutic effect of Levodopa-Containing Products. Management: Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): May diminish the therapeutic effect of Levodopa. Multivitamins/Minerals (with ADEK, Folate, Iron) may decrease the serum concentration of Levodopa. Only applies to oral iron-containing preparations. Management: Separate doses of these agents by 2 or more hours. Monitor for decreased levodopa effects, particularly if doses cannot be separated. Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May diminish the therapeutic effect of Levodopa-Containing Products. Management: Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Papaverine: May enhance the hypotensive effect of Levodopa-Containing Products. Papaverine may diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pyridoxine: May diminish the therapeutic effect of Levodopa-Containing Products. Management: The concomitant use of pyridoxine and levodopa (in the absence of a dopa decarboxylase inhibitor (DDI)) should be avoided. Use of a DDI (eg, carbidopa) with levodopa will essentially eliminate the risk of this interaction. Consider therapy modification
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sapropterin: May enhance the adverse/toxic effect of Levodopa-Containing Products. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Solriamfetol: Anti-Parkinson Agents (Dopamine Agonist) may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Spiramycin: May decrease the serum concentration of Carbidopa. And thus may decrease the effectiveness of levodopa. Monitor therapy
Sulpiride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
False-negative reaction using glucose-oxidase tests for glucosuria; false-positive urine ketones; false diagnosis for pheochromocytoma (rare) based on plasma and urine levels of catecholamines
Adverse Reactions
See individual agents.
Warnings/Precautions
Concerns related to adverse effects:
- Diarrhea: Has been associated with delayed development of diarrhea (onset after 4 to 12 weeks, but may appear as early as the first week); use with caution in patients with lower gastrointestinal disease or an increased risk of dehydration. Diarrhea may be a sign of drug-induced colitis. Monitor for weight loss. Discontinue use with prolonged diarrhea.
- Dyskinesias: May cause or exacerbate dyskinesias; may require dose adjustment.
- Hallucinations: May cause hallucinations.
- Impulse control disorders: Dopamine agonists used for Parkinson disease or restless legs syndrome have been associated with compulsive behaviors and/or loss of impulse control, which has manifested as pathological gambling, increased sexual urges, intense urges to spend money uncontrollably, and other intense urges. Dose reduction or discontinuation of therapy has been reported to reverse these behaviors in some, but not all cases.
- Melanoma: Risk for melanoma development is increased in Parkinson disease patients; drug causation or factors contributing to risk have not been established. Patients should be monitored closely and periodic skin examinations should be performed.
- Neuroleptic malignant syndrome: Entacapone, in conjunction with other drug therapy that alters brain biogenic amine concentrations (eg, MAO inhibitors, SSRIs), has been associated with a syndrome resembling neuroleptic malignant syndrome (hyperpyrexia and confusion) (some fatal) on abrupt withdrawal or dosage reduction. Concomitant use of entacapone and nonselective MAO inhibitors should be avoided.
- Orthostatic hypotension: Entacapone may cause orthostatic hypotension and syncope; Parkinson disease patients appear to have an impaired capacity to respond to a postural challenge; use with caution in patients at risk of hypotension (such as those receiving antihypertensive drugs) or in whom transient hypotensive episodes would be poorly tolerated (cardiovascular disease or cerebrovascular disease). Parkinson patients being treated with dopaminergic agonists ordinarily require careful monitoring for signs and symptoms of postural hypotension, especially during dose escalation, and should be informed of this risk.
- Pleural/retroperitoneal fibrosis: Ergot-derived dopamine agonists have also been associated with fibrotic complications (eg, retroperitoneal fibrosis, pleural effusions, pleural thickening, and pulmonary infiltrates); monitor closely for signs and symptoms of fibrosis.
- Rhabdomyolysis: Severe cases have been reported (rare); may be related to severe, prolonged motor activity/dyskinesia.
- Somnolence: Somnolence and falling asleep while engaged in activities of daily living (including operation of motor vehicles) have been reported; some cases reported that there were no warning signs for the onset of symptoms. Some events have occurred more than 1 year after start of therapy. Prior to treatment initiation, evaluate for factors that may increase these risks such as concomitant sedating medications, and the presence of sleep disorders. Monitor for drowsiness or sleepiness. If significant daytime sleepiness or episodes of falling asleep during activities that require active participation occurs (eg, driving, conversations, eating), discontinue the medication. There is insufficient information to suggest that dose reductions will eliminate these symptoms. If therapy is continued, advise patient to avoid driving and other potentially dangerous activities.
Disease-related concerns:
- Endocrine disease: Use with caution when interpreting plasma/urine catecholamine levels; falsely diagnosed pheochromocytoma has been rarely reported.
- Glaucoma: Use with caution in patients with wide-angle glaucoma; monitor IOP carefully; use is contraindicated in patients with narrow-angle glaucoma.
- Hepatic impairment: Use with caution in patients with hepatic impairment and biliary obstruction.
- Peptic ulcer disease: Use with caution in patients with a history of peptic ulcer disease; risk of gastrointestinal hemorrhage may be increased.
- Psychotic disorders: Use with extreme caution in patients with psychotic disorders; observe patients closely for development of depression with concomitant suicidal tendencies.
- Renal impairment: Use with caution in patients with severe renal impairment.
Concurrent drug therapy concerns:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in elderly patients; may be more sensitive to CNS effects (eg, hallucinations) of levodopa.
Dosage form specific issues:
- Sucrose: Contains sucrose; avoid use in patients with fructose intolerance, glucose-galactose malabsorption, or sucrase-isomaltase insufficiency.
Other warnings/precautions:
- Body fluid discoloration: Urine, saliva, or sweat may appear dark in color (red, brown, black) during therapy.
- Discontinuation of therapy: Dopaminergic agents have been associated with a syndrome resembling neuroleptic malignant syndrome on abrupt withdrawal or significant dosage reduction after long-term use.
Monitoring Parameters
Signs and symptoms of Parkinson's disease; CBC, liver function tests, renal function; blood pressure, mental status; signs and symptoms of neuroleptic malignant syndrome if abrupt discontinuation required (as with surgery); serum iron (if signs of anemia); IOP (in patients with wide-angle glaucoma); dermatologic examination (regularly while on therapy); weight loss (patients with diarrhea); cardiac function with initial dose adjustments and periodically during prolonged therapy (patients with history of MI, arrhythmia); fibrotic complications (eg, retroperitoneal fibrosis, pulmonary infiltrates or effusions, pleural thickening); signs of excessive drowsiness or sleepiness during treatment; signs of depression (including suicidal thoughts); signs and symptoms of impulse control/compulsive behaviors.
Pregnancy
Pregnancy Considerations
The incidence of Parkinson disease in pregnancy is relatively rare and information related to the use of carbidopa/levodopa/entacapone in pregnant women is limited (Seier 2017; Tüfekçioglu 2018).
Refer to the entacapone and the carbidopa/levodopa monographs for additional information.
Patient Education
What is this drug used for?
- It is used to treat Parkinson disease.
Frequently reported side effects of this drug
- Body fluid discoloration
- Constipation
- Fatigue
- Dry mouth
- Headache
- Trouble sleeping
- Back pain
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Behavioral changes
- Sensing things that seem real but are not
- Severe dizziness
- Passing out
- Confusion
- Narcolepsy
- Severe nausea
- Severe vomiting
- Severe or persistent diarrhea
- Vomiting blood
- Black, tarry, or bloody stools
- Severe abdominal pain
- Muscle pain
- Muscle weakness
- Skin growths
- Mole changes
- Uncontrollable urges
- Abnormal movements
- Extra muscle movement
- Change in balance
- Trouble swallowing
- Trouble speaking
- Chest pain
- Shortness of breath
- Chills
- Sore throat
- Bruising
- Bleeding
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.