Boxed Warning
Weight reduction:
Thyroid hormones, including levothyroxine, either alone or with other therapeutic agents, should not be used for the treatment of obesity or for weight loss. In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction. Larger doses may produce serious or even life-threatening manifestations of toxicity, particularly when given in association with sympathomimetic amines, such as those used for their anorectic effects.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Tirosint: 175 mcg, 200 mcg
Capsule, Oral, as sodium:
Tirosint: 13 mcg, 25 mcg, 50 mcg, 75 mcg, 88 mcg, 100 mcg, 112 mcg, 125 mcg, 137 mcg, 150 mcg
Solution, Intravenous [preservative free]:
Generic: 100 mcg/5 mL (5 mL); 200 mcg/5 mL (5 mL); 500 mcg/5 mL (5 mL)
Solution, Oral, as sodium:
Tirosint-SOL: 13 mcg/mL (1 mL); 25 mcg/mL (1 mL); 50 mcg/mL (1 mL); 75 mcg/mL (1 mL); 88 mcg/mL (1 mL); 100 mcg/mL (1 mL); 112 mcg/mL (1 mL); 125 mcg/mL (1 mL); 137 mcg/mL (1 mL); 150 mcg/mL (1 mL); 175 mcg/mL (1 mL); 200 mcg/mL (1 mL)
Solution Reconstituted, Intravenous, as sodium [preservative free]:
Generic: 100 mcg (1 ea); 200 mcg (1 ea); 500 mcg (1 ea)
Tablet, Oral, as sodium:
Euthyrox: 25 mcg, 50 mcg, 75 mcg, 88 mcg, 100 mcg, 112 mcg, 125 mcg, 137 mcg, 150 mcg, 175 mcg, 200 mcg [contains corn starch]
Levoxyl: 25 mcg [scored; contains fd&c yellow #6 aluminum lake]
Levoxyl: 50 mcg [scored]
Levoxyl: 75 mcg [scored; contains fd&c blue #1 aluminum lake]
Levoxyl: 88 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Levoxyl: 100 mcg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Levoxyl: 112 mcg [scored; contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Levoxyl: 125 mcg [scored; contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Levoxyl: 137 mcg, 150 mcg [scored; contains fd&c blue #1 aluminum lake]
Levoxyl: 175 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Levoxyl: 200 mcg [scored; contains fd&c yellow #10 aluminum lake]
Synthroid: 25 mcg [scored; contains fd&c yellow #6 aluminum lake]
Synthroid: 50 mcg [scored; contains corn starch]
Synthroid: 75 mcg [scored; contains corn starch, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake]
Synthroid: 88 mcg [scored; contains corn starch, fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Synthroid: 100 mcg [scored; contains corn starch, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Synthroid: 112 mcg [scored; contains corn starch]
Synthroid: 125 mcg [scored; contains corn starch, fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Synthroid: 137 mcg [scored; contains fd&c blue #1 aluminum lake]
Synthroid: 150 mcg [scored; contains fd&c blue #2 aluminum lake]
Synthroid: 175 mcg [scored; contains fd&c blue #1 aluminum lake]
Synthroid: 200 mcg [scored; contains fd&c red #40 aluminum lake]
Synthroid: 300 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid: 25 mcg [contains fd&c yellow #6 aluminum lake]
Unithroid: 50 mcg
Unithroid: 75 mcg [contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake]
Unithroid: 88 mcg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid: 100 mcg [contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid: 112 mcg
Unithroid: 125 mcg [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid: 137 mcg [contains fd&c blue #1 aluminum lake]
Unithroid: 150 mcg [contains fd&c blue #2 aluminum lake]
Unithroid: 175 mcg [contains fd&c blue #1 aluminum lake]
Unithroid: 200 mcg [contains fd&c red #40 aluminum lake]
Unithroid: 300 mcg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 (quinoline yellow), fd&c yellow #6 aluminum lake]
Unithroid Direct: 25 mcg [scored; contains fd&c yellow #6 aluminum lake]
Unithroid Direct: 50 mcg [scored]
Unithroid Direct: 75 mcg, 88 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid Direct: 100 mcg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid Direct: 112 mcg [scored]
Unithroid Direct: 125 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Unithroid Direct: 150 mcg [scored; contains fd&c blue #2 aluminum lake]
Unithroid Direct: 175 mcg [scored; contains fd&c blue #1 aluminum lake]
Unithroid Direct: 200 mcg [scored; contains fd&c red #40 aluminum lake]
Unithroid Direct: 300 mcg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Generic: 25 mcg, 50 mcg, 75 mcg, 88 mcg, 100 mcg, 112 mcg, 125 mcg, 137 mcg, 150 mcg, 175 mcg, 200 mcg, 300 mcg
Pharmacology
Mechanism of Action
Levothyroxine (T4) is a synthetic form of thyroxine, an endogenous hormone secreted by the thyroid gland. T4 is converted to its active metabolite, L-triiodothyronine (T3). Thyroid hormones (T4 and T3) then bind to thyroid receptor proteins in the cell nucleus and exert metabolic effects through control of DNA transcription and protein synthesis; involved in normal metabolism, growth, and development; promotes gluconeogenesis, increases utilization and mobilization of glycogen stores, and stimulates protein synthesis, increases basal metabolic rate
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Erratic (40% to 80% [per manufacturer]); reported bioavailability in fasting state is 79% to 81% (Dickerson 2010; Fish 1987). Absorption may be decreased by age and specific foods and drugs.
Metabolism
Hepatic to triiodothyronine (T3; active); ~80% thyroxine ( T4) deiodinated in kidney and periphery; glucuronidation/conjugation also occurs; undergoes enterohepatic recirculation
Excretion
Urine (major route of elimination; decreases with age); feces (~20%)
Onset of Action
Oral: 3 to 5 days; peak therapeutic effect may require 4 to 6 weeks; IV: Within 6 to 8 hours
Time to Peak
Serum: 2 to 4 hours
Half-Life Elimination
Euthyroid: 6 to 7 days; Hypothyroid: 9 to 10 days; Hyperthyroid: 3 to 4 days
Protein Binding
>99% bound to plasma proteins including thyroxine-binding globulin, thyroxine-binding prealbumin, and albumin
Use: Labeled Indications
Oral:
Hypothyroidism: Replacement or supplemental therapy in congenital or acquired hypothyroidism of any etiology. Specific indications include primary (thyroidal), secondary (pituitary), and tertiary (hypothalamic) hypothyroidism. Note: Levothyroxine monotherapy is recommended as the preferred thyroid preparation for the treatment of hypothyroidism (ATA [Jonklaas 2014]; ES [Fleseriu 2016]).
Pituitary thyrotropin-stimulating hormone suppression: An adjunct to surgery and radioiodine therapy in the management of thyrotropin-dependent well-differentiated thyroid cancer.
Injectable: Treatment of myxedema coma
Use: Off Label
Deceased organ donor management (hormonal resuscitation for the deceased organ donor)cyes
Data from retrospective cohort studies of brain-dead donors who successfully donated organs suggest that the use of levothyroxine given concomitantly with vasopressin, methylprednisolone, and a continuous infusion of insulin (goal blood glucose: 120 to 180 mg/dL) may be beneficial for hemodynamically unstable brain-dead donors to increase the quantity and quality of organs available for transplantation Novitzky 2014, Novitzky 2015, Rosendale 2003a, Rosendale 2003b; however, data supporting benefit are conflicting MacDonald 2012.
Based on a Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations consensus statement, the use of levothyroxine (or liothyronine) (in combination with vasopressin, methylprednisolone, and insulin) should be considered for hemodynamically unstable donors or potential cardiac donors with reduced left ventricular ejection fraction (<45%) Kotloff 2015.
Subclinical hypothyroidismcyes
Nonpregnant patients:
Data from a meta-analysis do not support the routine use of levothyroxine in nonpregnant adults with subclinical hypothyroidism Feller 2018. Clinical experience suggests treatment be considered in select patients depending on degree of TSH abnormality, age, and symptoms Ross 2019d.
Based on the American Association of Clinical Endocrinologists/American Thyroid Association (AACE/ATA) clinical practice guidelines for hypothyroidism in adults and the European Thyroid Association (ETA) guideline for management of subclinical hypothyroidism, thyroid replacement with levothyroxine is recommended in select patients with subclinical hypothyroidism (persistently elevated TSH with free T4 within normal range) AACE/ATA [Garber 2012], ETA [Pearce 2013].
Pregnant patients:
Clinical experience suggests treatment with levothyroxine for pregnant women with newly diagnosed subclinical hypothyroidism (defined as TSH above trimester-specific normal reference range [or above 4 milliunits/L if trimester-specific range unavailable] with normal free T4), regardless of thyroid peroxidase antibody status. Clinical experience also suggests treatment be considered in select pregnant women with TSH levels between 2.6 and 4 milliunits/L based on the presence or absence of thyroid peroxidase antibodies, clinical factors, and patient preferences Ross 2019b.
Based on the ATA guidelines for the diagnosis and management of thyroid disease during pregnancy and the postpartum, levothyroxine is recommended for select pregnant patients with subclinical hypothyroidism depending on the degree of TSH abnormality and presence or absence of thyroid peroxidase antibodies ATA [Alexander 2017].
Contraindications
Injection: Uncorrected adrenal insufficiency; consider contraindications for oral therapy if using as a temporary substitute for oral treatment (off-label use) in patients with chronic hypothyroidism.
Oral: Uncorrected adrenal insufficiency; hypersensitivity to glycerol (Tirosint oral solution); Note: Product labels may vary; also consult product labels. Reported hypersensitivity to levothyroxine or any component of the formulation is not considered an absolute contraindication (ATA [Jonklaas 2014]); refer to Warnings/Precautions.
Canadian labeling: Additional contraindications (not in US labeling): Untreated subclinical thyrotoxicosis, overt thyrotoxicosis of any etiology, acute myocardial infarction, acute myocarditis, or acute pancarditis
Dosage and Administration
Dosing: Adult
Note: Levothyroxine is synthetic thyroxine (T4). Due to its prolonged half-life, levothyroxine steady-state concentrations are not achieved until ~6 weeks after therapy is initiated or dosage adjustment; therefore, the full effect at a given dose may not be apparent until then. Individual T4 requirements correlate better with lean body mass than total body weight (Santini 2005). Weight-based dosing may overestimate initial replacement doses in obese patients. Initial doses >200 mcg/day are rarely used, regardless of patient weight (Roos 2005; manufacturer's labeling).
Deceased organ donor management (hormonal resuscitation for the deceased organ donor) (off-label use):
Note: Data supporting benefit are conflicting; if given, guidelines suggest use in hemodynamically unstable donors and/or potential cardiac donors with decreased left ejection fraction (<45%) (MacDonald 2012; Novitzky 2014; Novitzky 2015; SCCM/ACCP/AOPO [Kotloff 2015]).
IV: Initial: 20 mcg bolus, followed by a continuous infusion of 10 mcg/hour; levothyroxine is usually given as part of combination hormone therapy with vasopressin, methylprednisolone, and insulin (Kumar 2016; SCCM/ACCP/AOPO [Kotloff 2015]).
Hypothyroidism:
Note: Dose is individualized according to clinical response and serum thyroid stimulating hormone (TSH) and/or free T4 concentrations (ATA [Jonklaas 2014]; Ross 2019e). Average dose is ~1.6 mcg/kg/day; range of required doses is wide and varies from 50 to ≥200 mcg/day (Ross 2019e). Maintenance doses >300 mcg/day are rarely required; in patients who require high doses (eg, >2 mcg/kg/day), consider poor compliance, malabsorption, and/or drug interactions (Ross 2019e).
Primary hypothyroidism: Note: Adjust initial dose by 12 to 25 mcg/day every 3 to 6 weeks based on clinical response and serum TSH and/or free T4 concentrations until TSH is normalized at a stable dose for ≥6 weeks.
Patients ≤60 years of age without evidence of coronary heart disease: Oral: Initial: 1.6 mcg/kg/day (ATA [Jonklaas 2014]; Ross 2019e).
Patients >60 years of age without evidence of coronary heart disease: Oral: Initial: 25 to 50 mcg once daily (AACE/ATA Garber 2012]; ATA [Jonklaas 2014]); Ross 2019e).
Patients with coronary heart disease: Oral: Initial: 12.5 to 50 mcg once daily (AACE/ATA [Garber 2012]; ATA [Jonklaas 2014]; Ross 2019e); monitor for the onset of cardiac symptoms (eg, angina) and decrease the dose if needed (AACE/ATA [Garber 2012]). Note: Patients without other significant comorbidities who have had recent successful interventions to treat ischemia (eg, coronary artery bypass grafting or coronary artery stenting) can initially receive up to 80% of the weight-based dose (1.6 mcg/kg/day) (Ross 2019e).
Pregnant patients: Note: Thyroid function tests should be interpreted using population-based, trimester-specific reference ranges for TSH and assay method- and trimester-specific reference ranges for serum free T4 (ATA [Alexander 2017]).
Preexisting hypothyroidism in women receiving levothyroxine prenatally: Patients with suspected or confirmed pregnancy: Oral: Immediately increase the current dose by ~30% (eg, administer 2 additional tablets weekly of the current dose) and adjust dose as needed every 4 weeks (ATA [Alexander 2017]).
Newly diagnosed overt hypothyroidism: Oral: Initial: 1.6 mcg/kg/day; adjust dose by ~25 mcg/day as needed every 4 to 6 weeks to restore patient to euthyroidism as soon as possible (ACOG 2015; ATA [Alexander 2017]; Ross 2019b).
Newly diagnosed subclinical hypothyroidism (off-label use):
Note: The decision to treat is based on the degree of TSH elevation and the presence or absence of thyroid peroxidase antibodies. If treated, goal is to restore euthyroidism (ATA [Alexander 2017]). Some experts treat pregnant women with subclinical hypothyroidism (defined as TSH above trimester-specific normal reference range [or above 4 milliunits/L if trimester-specific range unavailable] with normal free T4), regardless of thyroid peroxidase antibody status, and would consider treatment in select pregnant women with TSH levels between 2.6 and 4 milliunits/L based on the presence or absence of thyroid peroxidase antibodies, clinical factors, and patient preferences (Ross 2019b).
Oral: Initial: 1 mcg/kg/day or 50 mcg daily; adjust dose by ~12 to 25 mcg/day as needed every 4 weeks (ATA [Alexander 2017]; Ross 2019b).
Postpartum dosage adjustment: In patients treated prenatally for hypothyroidism, decrease the dose to preconception levels following delivery. In patients who were initiated on levothyroxine during pregnancy, evaluate the need for continued treatment (ATA [Alexander 2017]).
Subclinical hypothyroidism (off-label use):
Note: Treatment may be considered in select patients with TSH levels above normal reference range depending on degree of TSH abnormality, age, and symptoms (Feller 2018; Ross 2019d). In patients with TSH >10 milliunits/L, treatment is generally warranted, whereas benefit of treatment in asymptomatic patients with TSH levels between 4.5 and 10 milliunits/L is not well established (AACE/ATA [Garber 2012]; Ross 2019d).
Adults <50 years of age without coronary heart disease: Oral: Initial: 1.5 mcg/kg/day (ETA [Pearce 2013]; Ross 2019d).
Patients with coronary heart disease or ≥50 years of age: Oral: Initial: 25 to 50 mcg once daily (ETA [Pearce 2013]; Ross 2019d).
Dosage adjustment: Initial dose is adjusted by 12 to 25 mcg/day once every 6 weeks until targeted TSH is achieved with a stable dose for ≥6 weeks; thereafter assess TSH level annually (Ross 2019d).
Postpartum thyroiditis (hypothyroid phase):
Note: Treat women who are symptomatic or planning another pregnancy (ATA [Alexander 2017]; Stagnaro-Green 2011); some experts will treat asymptomatic patients who are breastfeeding (ATA [Alexander 2017]) or who have a TSH >10 milliunits/L (Burman 2019). Dosing recommendations and duration of treatment are not standardized; treatment is individualized according to clinical assessment:
Oral: Initial: 25 to 75 mcg once daily (ACOG 2015); alternatively, some experts suggest an initial dose of 50 to 100 mcg once daily (Burman 2019). Adjust dose as needed once every 4 to 6 weeks until TSH is normalized. Tapering of the dose with a goal of discontinuation, if possible, may begin after 6 to 12 months of treatment (ACOG 2015; Stagnaro-Green 2011).
Secondary hypothyroidism:
Note: Patients with secondary (central) hypothyroidism should undergo assessment of their pituitary-adrenal function prior to initiation of therapy. If shown to have adrenal insufficiency, concomitant administration of a glucocorticoid is recommended to prevent an adrenal crisis (ATA [Jonklaas 2014]; Ross 2019a).
Oral: Initial: 1.6 mcg/kg/day; some experts initiate treatment at a lower dose in older patients or patients with underlying coronary heart disease (Ross 2019a). Adjust dose based on clinical response and serum free T4 concentrations. TSH cannot be used to monitor therapy (ATA [Jonklaas 2014]; Ross 2019a).
Myxedema coma:
IV: Initial loading dose of 200 to 400 mcg as a slow bolus; followed by a daily replacement dose of 50 to 100 mcg until the patient improves clinically and can transition to oral therapy; consider doses on the lower end of the dosing range for smaller or older patients and those with a history of or at risk for coronary disease or arrhythmia; concomitant glucocorticoid therapy is required until the possibility of coexisting adrenal insufficiency is excluded (ATA [Jonklaas 2014]; Ross 2019c); some experts administer liothyronine (T3) concomitantly with levothyroxine (T4) (Ross 2019c).
TSH suppression:
Well-differentiated thyroid cancer (papillary and follicular): Dosage is highly individualized as the degree of TSH suppression is initially based on the risk of disease recurrence using a staging system such as the American Thyroid Association (ATA) risk-of-recurrence stratification system (ATA [Haugen 2016]; Tuttle 2019). Long-term TSH suppression goals should account for response to therapy, risk of recurrent disease, age, and comorbid conditions (ATA [Haugen 2016]).
Oral: Initial: 1.6 to 2 mcg/kg/day immediately postsurgery (Tuttle 2019); adjust dose as needed in 6 weeks based on TSH suppression goals (ATA [Haugen 2016]):
Note: For patients with ATA low-risk disease whose initial surgery was a lobectomy, some experts initiate therapy at a later time when TSH concentrations or disease status dictate a need (ATA [Haugen 2016]; Lee 2015; Tuttle 2019).
Benign solitary nodules and nontoxic multinodular goiter: Routine use of levothyroxine for TSH suppression is not recommended in euthyroid patients with benign thyroid nodules in iodine-sufficient geographic areas. In patients deemed appropriate candidates, treatment should never be fully suppressive (ie, do not target TSH <0.1 milliunits/L) (AACE/ACE/AME [Gharib 2016]; ATA [Haugen 2016]).
IV/IM replacement in patients who are temporarily unable to receive oral therapy:
IM (off-label route), IV (off-label use): Administer ~75% to 80% of the established oral dose once daily (ATA [Jonklaas 2014]; Manzullo 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Doses should be adjusted based on clinical response and laboratory parameters; on a weight basis, dosing is higher in infants and children than adults due to the higher metabolic clearance.
Hypothyroidism (acquired or congenital): Note: Hyperactivity in older children may be minimized by starting at one-quarter (25%) of the recommended dose and increasing each week by that amount until the full dose is achieved (4 weeks).
Oral:
1 to 3 months: 10 to 15 mcg/kg/dose once daily; in severe cases of hypothyroidism (serum T4 <5 mcg/dL), initiating at higher doses (12 to 17 mcg/kg/dose) may be necessary (AAP 2006; ATA [Jonklaas 2014]; Léger 2014; Selva 2002).
>3 to 6 months: 8 to 10 mcg/kg/dose once daily
>6 to 12 months: 6 to 8 mcg/kg/dose once daily
1 to 5 years: 5 to 6 mcg/kg/dose once daily
6 to 12 years: 4 to 5 mcg/kg/dose once daily
>12 years with incomplete growth and puberty: 2 to 3 mcg/kg/dose once daily
Adolescents with growth and puberty complete: 1.6 mcg/kg/dose once daily; adjust dose by 12.5 to 25 mcg/day every 4 to 6 weeks as needed. Usual doses are ≤200 mcg/day (range: 100 to 125 mcg/day [70 kg adult]); doses ≥300 mcg/day are rare (consider poor compliance, malabsorption, and/or drug interactions).
Cardiac disease: Note: Lower initial doses are recommended.
Infants and Children: Initial: ~50% of target replacement dose; increase after 2 weeks based on free thyroxine levels (Léger 2014)
Adolescents with growth and puberty complete: Initial: 12.5 to 25 mcg/day; adjust dose by 12.5 to 25 mcg increments at 6- to 8-week intervals as needed
IV: Note: The relative bioavailability of injectable and oral levothyroxine has not been established; use caution when switching patients from oral to IV as accurate dosing conversions have not been established. Infants, Children, and Adolescents: ~75% to 80% of the oral dose has been suggested by guidelines (ATA [Jonklaas 2014]; Léger 2014).
Thyroid-stimulating hormone (TSH) suppression in well differentiated thyroid cancer (papillary): Infants, Children, and Adolescents: Oral: Highly individualized; doses >2 mcg/kg/day may be needed to suppress TSH to <0.1 milliunits/L in high-risk tumors; for intermediate-risk tumors, initial TSH suppression to 0.1 to 0.5 milliunits/L is recommended; for low-risk tumors, TSH may be maintained at 0.5 to 1 milliunits/L (ATA [Francis 2015]).
Organ donor management in brain-dead patients (hormone replacement therapy) (Nakagawa 2008; Zuppa 2004): IV:
Infants <6 months: Initial: 5 mcg/kg bolus dose, followed by 1.4 mcg/kg/hour infusion
Infants 6 to 12 months: Initial: 4 mcg/kg bolus dose, followed by 1.3 mcg/kg/hour infusion
Children 1 to 5 years: Initial: 3 mcg/kg bolus dose, followed by 1.2 mcg/kg/hour infusion
Children 6 to 12 years: Initial: 2.5 mcg/kg bolus dose, followed by 1 mcg/kg/hour infusion
Children ≥12 years and Adolescents ≤16 years: Initial: 1.5 mcg/kg bolus dose, followed by 0.8 mcg/kg/hour infusion
Adolescents >16 years: Initial: 0.8 mcg/kg bolus dose, followed by 0.8 mcg/kg/hour infusion
Dosing: Adjustment for Toxicity
Cardiac symptoms (onset or worsening): Manufacturer labeling recommends reducing dosage or withholding therapy for 7 days and then resuming therapy at reduced dosage. Specific dosing recommendations are not provided.
Dosing: Obesity
Individual T4 requirements correlate better with lean body weight than total body weight (Santini 2005); weight-based dosing may overestimate initial replacement doses in obese patients; as such, dosing in obesity must be individualized.
Reconstitution
For products requiring further dilution, reconstitute vial for injection with 5 mL NS. Reconstituted concentrations for the 100 mcg, 200 mcg, and 500 mcg vials are 20 mcg/mL, 40 mcg/mL, and 100 mcg/mL, respectively. Shake well and use immediately after reconstitution (manufacturer labeling suggests reconstituted vial is stable for 4 hours); discard any unused portions.
Extemporaneously Prepared
Note: A levothyroxine oral solution (multiple concentrations) is commercially available (Tirosint-SOL).
25 mcg/mL Oral Suspension
A 25 mcg/mL oral suspension may be made with tablets and 40 mL glycerol. Crush twenty-five 100 mcg levothyroxine tablets in a mortar and reduce to a fine powder. Add small portions of glycerol and mix to a uniform suspension. Transfer to a calibrated 100 mL amber bottle; rinse the mortar with about 10 mL of glycerol and pour into the bottle; repeat until all 40 mL of glycerol is used. Add quantity of water sufficient to make 100 mL. Label "shake well" and "refrigerate". Stable for 8 days refrigerated.
Boulton DW, Fawcett JP, and Woods DJ, "Stability of an Extemporaneously Compounded Levothyroxine Sodium Oral Liquid," Am J Health Syst Pharm, 1996, 53(10):1157-61.8734676
Administration
Oral: Administer consistently in the morning on an empty stomach, at least 30 to 60 minutes before food. Alternatively, may consistently administer at night 3 to 4 hours after the last meal (AACE/ATA [Garber 2012]; ATA [Jonklaas 2014]). Do not administer within 4 hours of calcium- or iron-containing products or bile acid sequestrants.
Capsule: Must be swallowed whole; do not cut, crush, or chew.
Solution (Tirosint): May administer undiluted or diluted in water only (do not dilute with any other liquid); if administering undiluted, squeeze contents of single unit-dose ampule into mouth or onto a spoon and administer immediately. If diluting with water, squeeze contents of ampule into a glass or cup, stir, and then administer entire contents immediately. Rinse glass or cup with additional water and administer contents to ensure entire dose is consumed.
Tablet: Administer with a full glass of water (choking, gagging, and dysphagia have been reported with some formulations). May be crushed and suspended in 5 to 10 mL of water; suspension should be used immediately.
Nasogastric tube: Bioavailability of levothyroxine (crushed tablets suspended in water) is reduced if administered with enteral tube feeds. Since holding feedings for at least 1 hour before and after levothyroxine administration may not completely resolve the interaction, an increase in dose (eg, additional 25 mcg) may be necessary (Dickerson 2010). Tirosint oral solution product labeling does not provide recommendations regarding nasogastric administration.
Parenteral: May be administered by IV injection at a maximum rate of 100 mcg/minute; may also be administered IM when oral administration is not feasible (off-label route).
Cadaveric organ recovery (hormonal resuscitation) (off-label use): After IV bolus administration, may administer as a continuous infusion (Salim 2007).
Storage
Capsules and tablets: Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect from heat, light, and moisture.
Oral solution (Tirosint): Store in original container (closed aluminum pouch) at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Keep ampules in pouch until ready to use; after opening the pouch, all ampules in the pouch should be used within 15 days.
Injection: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Additional stability data:
Stability in polypropylene syringes (100 mcg/mL in NS) at 5°C ± 1°C is 7 days (Gupta 2000).
Stability in latex-free, PVC minibags protected from light and stored at 15°C to 30°C (59°F to 86°F) was 12 hours for a 2 mcg/mL concentration or 18 hours for a 0.4 mcg/mL concentration in NS. May be exposed to light; however, stability time is significantly reduced, especially for the 2 mcg/mL concentration (Strong 2010).
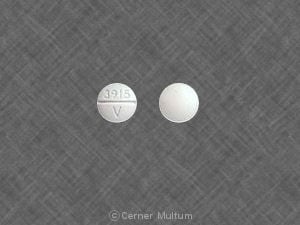
Levothyroxine Images
Drug Interactions
Aluminum Hydroxide: May decrease the serum concentration of Levothyroxine. Management: Separate administration of oral levothyroxine and aluminum hydroxide by at least 4 hours. Consider therapy modification
Amezinium: Thyroid Products may enhance the stimulatory effect of Amezinium. Monitor therapy
Amiodarone: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Apalutamide: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Bile Acid Sequestrants: May decrease the serum concentration of Thyroid Products. Management: Administer oral thyroid products at least 4 h prior to colesevelam, and at least 1 h before or 4-6 h after cholestyramine. Specific recommendations for colestipol are not available. Monitor for decreased concentrations/effects of the thyroid product. Consider therapy modification
Calcium Polystyrene Sulfonate: May decrease the serum concentration of Thyroid Products. Management: To minimize risk of interaction, separate dosing of oral calcium polystyrene sulfonate and thyroid products (eg, levothyroxine) or administer calcium polystyrene sulfonate rectally. Monitor for signs/symptoms of hypothyroidism with concomitant use (oral). Consider therapy modification
Calcium Salts: May diminish the therapeutic effect of Thyroid Products. Management: Separate the doses of the thyroid product and the oral calcium supplement by at least 4 hours. Consider therapy modification
CarBAMazepine: May decrease the serum concentration of Thyroid Products. Monitor therapy
Ciprofloxacin (Systemic): May decrease the serum concentration of Thyroid Products. Monitor therapy
Estrogen Derivatives: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Fosphenytoin: May decrease the serum concentration of Thyroid Products. Phenytoin may also displace thyroid hormones from protein binding sites. Monitor therapy
Iron Preparations: May decrease the serum concentration of Levothyroxine. Management: Separate oral administration of iron preparations and levothyroxine by at least 4 hours. Separation of doses is not required with parenterally administered iron preparations or levothyroxine. Exceptions: Ferric Carboxymaltose; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Lanthanum: May decrease the serum concentration of Thyroid Products. Management: Administer oral thyroid products at least two hours before or after lanthanum. Consider therapy modification
Magnesium Salts: May decrease the serum concentration of Levothyroxine. Management: Separate administration of oral levothyroxine and oral magnesium salts by at least 4 hours. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Levothyroxine. Management: Separate oral administration of iron-containing multivitamins and levothyroxine by at least 4 hours. Consider therapy modification
Orlistat: May decrease the serum concentration of Levothyroxine. Management: Separate administration of oral levothyroxine and orlistat by a least 4 hours. Monitor patients closely for signs and symptoms of hypothyroidism. Consider therapy modification
Patiromer: May decrease the serum concentration of Levothyroxine. Management: Administer oral levothyroxine at least 3 hours before or 3 hours after patiromer. Consider therapy modification
Phenytoin: May decrease the serum concentration of Thyroid Products. Phenytoin may also displace thyroid hormones from protein binding sites. Monitor therapy
Piracetam: May enhance the adverse/toxic effect of Thyroid Products. Specifically, symptoms including confusion, irritability, and sleep disorder have been described during concomitant use. Monitor therapy
Polaprezinc: May decrease the serum concentration of Levothyroxine. Consider therapy modification
Raloxifene: May decrease the absorption of Levothyroxine. Consider therapy modification
RifAMPin: May decrease the serum concentration of Thyroid Products. Monitor therapy
Ritonavir: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May diminish the therapeutic effect of Thyroid Products. Thyroid product dose requirements may be increased. Monitor therapy
Semaglutide: May increase the serum concentration of Levothyroxine. Monitor therapy
Sevelamer: May decrease the serum concentration of Levothyroxine. Management: Consider separating administration of sevelamer and levothyroxine by at least several hours whenever possible in order to decrease the risk of a significant interaction. Consider therapy modification
Sodium Iodide I131: Thyroid Products may diminish the therapeutic effect of Sodium Iodide I131. Avoid combination
Sodium Polystyrene Sulfonate: May decrease the serum concentration of Thyroid Products. Management: To minimize risk of interaction, separate dosing of oral sodium polystyrene sulfonate and thyroid products (e.g., levothyroxine) or administer sodium polystyrene sulfonate rectally. Monitor for signs/symptoms of hypothyroidism with concomitant use (oral). Consider therapy modification
Somatropin: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Sucralfate: May decrease the serum concentration of Levothyroxine. Monitor therapy
Sucroferric Oxyhydroxide: May decrease the serum concentration of Levothyroxine. Management: Administer oral/enteral levothyroxine at least 4 hours before administration of sucroferric oxyhydroxide. No interaction is anticipated with parenteral levothyroxine administration. Consider therapy modification
Theophylline Derivatives: Thyroid Products may increase the metabolism of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Tricyclic Antidepressants: Thyroid Products may enhance the arrhythmogenic effect of Tricyclic Antidepressants. Thyroid Products may enhance the stimulatory effect of Tricyclic Antidepressants. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Thyroid Products may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
T4-binding globulin (TBG): Factors that alter binding in serum (ATA/AACE [Garber 2012]):
Note: T4 is ~99.97% protein bound. Factors that alter protein binding will affect serum total T4 levels; however, measurement of serum free T4 (the metabolically active moiety) has largely replaced serum total T4 for thyroid status assessment.
Conditions/states that increase TBG binding: Pregnancy, hepatitis, porphyria, neonatal state
Medications that increase TBG binding: Estrogens, 5-fluorouracil, heroin, methadone, mitotane, perphenazine, selective estrogen receptor modulators (eg, tamoxifen, raloxifene)
Conditions/states that decrease TBG binding: Hepatic failure, nephrosis, severe illness.
Medications that decrease TBG binding: Androgens, anabolic steroids, glucocorticoids, L-asparaginase, nicotinic acid
Thyroxine (T4) and triiodothyronine (T3): Serum binding inhibitors (ATA/AACE [Garber 2012]):
Medications that inhibit T4 and T3 binding: Carbamazepine, furosemide, free fatty acids, heparin, NSAIDS (variable, transient), phenytoin, salicylates
Thyroid gland hormone: Interference with production and secretion (ATA/AACE [Garber 2012]):
Medications affecting iodine uptake: Amiodarone, iodinated contrast agents, iodine, ethionamide
Medications affecting hormone production: Amiodarone, ethionamide, iodinated contrast agents, iodine, sulfonylureas, sulfonamides, thionamides (carbimazole, methimazole, propylthiouracil),
Medications affecting secretion: Amiodarone, iodinated contrast agents, iodine, lithium
Medications inducing thyroiditis: Alemtuzumab, amiodarone, antiangiogenic agents (lenalidomide, thalidomide), denileukin diftitox, interferon alpha, interleukins, lithium, tyrosine kinase inhibitors (sunitinib, sorafenib)
Medications potentially causing the development of Graves’: Alemtuzumab, interferon alpha, antiretroviral therapy
Medications potentially ameliorating thyroiditis (if autoimmune) or Graves’: Glucocorticoids
Hypothalamic-pituitary axis and TSH: Interference with secretion (ATA/AACE [Garber 2012]):
Medications decreasing TSH secretion: Bexarotene, dopamine, dopaminergic agonists (bromocriptine, cabergoline), glucocorticoids, interleukin-6, metformin, opiates, somatostatin analogues (octreotide, lanreotide), thyroid hormone analogues
Medications increasing TSH secretion: Amphetamine, interleukin 2, metoclopramide, ritonavir, St John's wort
Medications potentially causing hypophysitis: Ipilimumab
Adverse Reactions
Adverse reactions are primarily those of hyperthyroidism due to therapeutic overdosage.
Frequency not defined:
Cardiovascular: Angina pectoris, cardiac arrhythmia, cardiac failure, flushing, increased blood pressure, increased pulse, myocardial infarction, palpitations, tachycardia
Central nervous system: Anxiety, emotional lability, fatigue, headache, heat intolerance, hyperactivity, insomnia, irritability, myasthenia, nervousness, pseudotumor cerebri (children)
Dermatologic: Alopecia, diaphoresis, skin rash
Endocrine & metabolic: Goiter (exophthalmic; IV), menstrual disease, weight loss
Gastrointestinal: Abdominal cramps, diarrhea, increased appetite, vomiting
Genitourinary: Reduced fertility
Hepatic: Increased liver enzymes
Neuromuscular & skeletal: Decreased bone mineral density, muscle spasm, slipped capital femoral epiphysis (children), tremor
Respiratory: Dyspnea
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Dysgeusia (Syed 2016), seizure
Warnings/Precautions
Disease-related concerns:
- Adrenal insufficiency: Use with caution in patients with adrenal insufficiency; symptoms may be exaggerated or aggravated. Treatment with glucocorticoids should precede levothyroxine therapy in patients with adrenal insufficiency. Use is contraindicated in patients with uncorrected adrenal insufficiency.
- Benign thyroid nodules: Appropriate use: Routine use of T4 for thyroid stimulating hormone (TSH) suppression is not recommended in patients with benign thyroid nodules. Treatment should never be fully suppressive (TSH <0.1 milliunits/L) (AACE/ACE/AME [Gharib 2016]; ATA [Haugen 2016]).
- Use of T4 may be considered in association with iodine supplementation only in young patients residing in iodine-deficient areas with small thyroid nodules and no evidence of functional autonomy (AACE/ACE/AME [Gharib 2016]).
- Use should be avoided in postmenopausal women, elderly patients, patients with cardiovascular disease, osteoporosis, large thyroid nodules or long-standing goiters, or low-normal TSH levels (AACE/ACE/AME [Gharib 2016]).
- Cardiovascular disease: Use with caution and reduce dosage in patients with cardiovascular disease; patients with developing or worsening cardiac symptoms should have their dose reduced or therapy withheld for 7 days and then resumed at a reduced dose. Chronic hypothyroidism predisposes patients to coronary artery disease; monitor patients closely for development of cardiac ischemia. Similarly, patients with heart failure and hypothyroidism should be closely followed.
- Diabetes: Use with caution in patients with diabetes mellitus (may worsen glycemic control) and diabetes insipidus (thyroid hormone increases glomerular filtration rate and downregulates aquaporin channels in the renal tubules, which could affect urinary output) (Mariani 2012).
- Osteoporosis: Long-term therapy can decrease bone mineral density and appears to be dose-related (Schneider 1994). Postmenopausal women and women using suppressive doses should receive the lowest dose necessary for clinical response.
- Subacute thyroiditis: Transient and mild hypothyroidism during the recovery phase of subacute thyroiditis often can be managed without treatment; levothyroxine therapy may be required in patients with overt and clinical hypothyroidism (Farwell 2013).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution; suppressed TSH levels may increase risk of atrial fibrillation and mortality secondary to cardiovascular disease (Gharib 2016; Parle 2001). Increase dose slowly and monitor for signs/symptoms of angina.
Dosage form specific issues:
- Product interchangeability: Switching between different levothyroxine products may result in variations in the administered dose and altered TSH values and is not generally recommended; if formulations are changed, close monitoring of TSH is recommended (ATA [Jonklaas 2014]). Pediatric patients with congenital hypothyroidism may be more sensitive to changes in formulation (Carswell 2013).
Other warnings/precautions:
- Hypersensitivity: Patients with reported hypersensitivity to levothyroxine may be managed with dose reductions and slow titration, by switching formulations or products, or referral to an allergist (ATA [Jonklaas 2014]).
- Weight reduction (off-label use): [US Boxed Warning]: Thyroid supplements are ineffective and potentially toxic when used for the treatment of obesity or for weight reduction, especially in euthyroid patients. High doses may produce serious or even life-threatening toxic effects, particularly when used with some anorectic drugs (eg, sympathomimetic amines). Levothyroxine, either alone or with other concomitant therapeutic agents, should not be used for the treatment of obesity or for weight loss.
Monitoring Parameters
Pediatrics: Monitor closely for under/overtreatment. Undertreatment may decrease intellectual development and linear growth and lead to poor school performance due to impaired concentration and slowed mentation. Overtreatment may adversely affect brain maturation and accelerate bone age (leading to premature closure of the epiphyses and reduced adult height); craniosynostosis has been reported in infants. Perform routine clinical examinations at regular intervals (to assess mental and physical growth and development). Treated children may experience a period of catch-up growth. Monitor TSH and total or free T4 at 2 and 4 weeks after starting treatment, every 1 to 2 months during the first year of life, every 2 to 3 months between ages 1 to 3 years, and every 3 to 12 months thereafter until growth is completed (AAP 2006; ATA [Jonklaas 2014]); repeat tests 2 weeks after any change in dosage.
Adults: Heart rate, blood pressure, clinical signs of hypo- and hyperthyroidism; bone mineral density (particularly with long term use in postmenopausal women)
Primary hypothyroidism: In patients who experience symptomatic improvement following initiation of therapy or dosage adjustment, measure TSH response at 6 weeks and titrate therapy as needed (ATA [Jonklaas 2014]). In those who continue to experience symptoms, consider measuring free T4 (FT4) and TSH at 3 weeks and increasing the dose if FT4 is below normal (Ross 2019e); clinicians should note that the full effect of the dose may not be apparent at 3 weeks as levothyroxine does not achieve steady state until ~6 weeks post-initiation or dosage adjustment. Continue to measure serum TSH (and FT4 if levothyroxine steady state has not yet been achieved) every 3 to 6 weeks and titrate the dose until the TSH concentration is within the goal range (ATA [Jonklaas 2014]; Ross 2019e).
Hypothyroidism in pregnant patients: Clinical decisions in this patient population should rely on trimester- and population-specific reference ranges (ATA [Alexander 2017]). TSH goals should target the lower half of the trimester-specific reference range (or <2.5 milliunits/L when trimester-specific targets are unavailable) (ATA [Alexander 2017]). Patients with or at risk for hypothyroidism should undergo TSH evaluation every 4 weeks until midgestation and at least once near 30 weeks gestation (ATA [Alexander 2017]; De Groot 2012); re-assess TSH 2 to 4 weeks after initiation of therapy or dosage adjustment (ATA [Alexander 2017]). In patients who were initiated on levothyroxine during pregnancy, the necessity of continuing treatment should be evaluated; some patients will not require continued therapy. TSH should be measured 6 weeks after dosage adjustment or discontinuation (ATA [Alexander 2017]).
Postpartum thyroiditis: Evaluate TSH every 2 months following resolution of the thyrotoxic phase of PPT until 1 year following delivery.
Secondary hypothyroidism: Monitor response to treatment with measurement of FT4 concentrations; goal of treatment is to maintain FT4 concentrations in upper half of the reference range (or slightly higher than mid-normal (ATA [Jonklaas 2014]; Ross 2019d).
Pregnancy
Pregnancy Considerations
Levothyroxine has not been shown to increase the risk of congenital abnormalities or miscarriage. Maternal hypothyroidism, however, can be associated with adverse effects in the mother and fetus, including spontaneous abortion, stillbirth, premature birth, low birth weight, impaired neurocognitive development in the off-spring, abruptio placentae, gestational hypertension, and preeclampsia (ACOG 148 2015; ATA [Alexander 2017]).
Thyroid replacement therapy minimizes the risk of adverse pregnancy outcomes in females with overt hypothyroidism and treatment is recommended during pregnancy (ACOG 148 2015; ATA [Alexander 2017]). Levothyroxine is the preferred treatment of maternal hypothyroidism; other agents should not be used in pregnant females (ACOG 148 2015; ATA [Alexander 2017]; ES [De Groot 2012]). Levothyroxine is also recommended in some cases of subclinical hypothyroidsim during pregnancy, and overt hypothyroidism in females with postpartum thyroiditis (ACOG 148 2015; ATA [Alexander 2017]; ES [De Groot 2012]).
Due to alterations of endogenous maternal thyroid hormones, hypothyroid patients treated with levothyroxine prior to pregnancy require a dose increase as soon as pregnancy is confirmed (ATA [Alexander 2017]; ES [De Groot 2012]). Close monitoring of pregnant patients is recommended (ATA [Alexander 2017]).
Overt hypothyrodism increases the risk of infertility; treatment with levothyroxine is recommended to normalize thyroid function in infertile females with overt hypothyroidism who desire pregnancy. Levothyroxine may also be used in infertile females with subclinical hypothyrodism using assisted reproductive techniques (ATA [Alexander 2017]).
Patient Education
What is this drug used for?
- It is used to add thyroid hormone to the body.
- It is used to manage thyroid cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hair loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Headache
- Dizziness
- Passing out
- Vision changes
- Shortness of breath
- Loss of strength and energy
- Lack of appetite
- Increased appetite
- Excessive weight gain or loss
- Swelling of arms or legs
- Diarrhea
- Abdominal cramps
- Vomiting
- Irritability
- Anxiety
- Emotional instability
- Tremors
- Trouble sleeping
- Temperature sensitivity
- Sweating a lot
- Muscle cramps
- Muscle weakness
- Flushing
- Bone pain
- Menstrual irregularities
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.