Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous:
Generic: 600 mg/300 mL (300 mL)
Solution, Intravenous [preservative free]:
Zyvox: 200 mg/100 mL (100 mL); 600 mg/300 mL (300 mL)
Generic: 600 mg/300 mL (300 mL)
Suspension Reconstituted, Oral:
Zyvox: 100 mg/5 mL (150 mL) [orange flavor]
Generic: 100 mg/5 mL (150 mL)
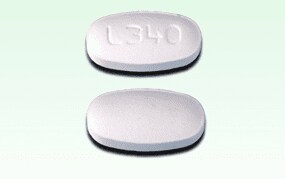
Tablet, Oral:
Zyvox: 600 mg
Generic: 600 mg
Pharmacology
Mechanism of Action
Inhibits bacterial protein synthesis by binding to bacterial 23S ribosomal RNA of the 50S subunit. This prevents the formation of a functional 70S initiation complex that is essential for the bacterial translation process. Linezolid is bacteriostatic against enterococci and staphylococci and bactericidal against most strains of streptococci.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and extensive
Distribution
Vd:
Preterm neonates <1 week: 0.81 L/kg
Full-term neonates <1 week: 0.78 L/kg
Full-term neonates ≥1 week to ≤28 days: 0.66 L/kg
Infants >28 days to <3 months: 0.79 L/kg
Infants and Children 3 months to 11 years: 0.69 L/kg
Adolescents: 0.61 L/kg
Adults: 0.65 L/kg
Metabolism
Hepatic via oxidation of the morpholine ring, resulting in two inactive metabolites (aminoethoxyacetic acid, hydroxyethyl glycine); minimally metabolized, may be mediated by cytochrome P450
Excretion
Urine (~30% of total dose as parent drug, ~50% of total dose as metabolites); two metabolites of linezolid may accumulate in patients with severe renal impairment; feces (~9% of total dose as metabolites)
Nonrenal clearance: Adults: ~65%
Clearance:
Preterm neonates <1 week: 2 mL/minute/kg
Full-term neonates <1 week: 3.8 mL/minute/kg
Full-term neonates ≥1 week to ≤28 days: 5.1 mL/minute/kg
Infants >28 days to <3 months: 5.4 mL/minute/kg
Infants and Children 3 months to 11 years: 3.8 mL/minute/kg
Adolescents: 2.1 mL/minute/kg
Adults: 1.7 mL/minute/kg
Time to Peak
Adults: Oral: 1 to 2 hours
Half-Life Elimination
Preterm neonates <1 week: 5.6 hours
Full-term neonates <1 week: 3 hours
Full-term neonates ≥1 week to ≤28 days: 1.5 hours
Infants >28 days to <3 months: 1.8 hours
Infants and Children 3 months to 11 years: 2.9 hours
Adolescents: 4.1 hours
Adults: 4.9 hours
Protein Binding
Adults: 31%
Use in Specific Populations
Special Populations: Renal Function Impairment
Data are conflicting regarding the contribution of renal dysfunction to the elimination of linezolid. Several studies indicate that linezolid exposure is increased in patients with significant renal dysfunction (Cattaneo 2016; Gervasoni 2015; Ide 2018; Matsumoto 2010; Nukui 2013; Sasaki 2011; Tsuji 2017) although this may be reduced by a compensatory increase in non-renal elimination (Brier 2003; El-Assal 2014). Metabolites A and B accumulate in patients with renal insufficiency; the significance of this accumulation is not known.
Use: Labeled Indications
Enterococcal infections (vancomycin-resistant): Treatment of vancomycin-resistant Enterococcus faecium infections, including cases with concurrent bacteremia. Note: Not a preferred agent in resistant Enterococcus faecalis infections, which are usually susceptible to beta-lactams (O’Driscoll 2015).
Pneumonia:
Community-acquired: Treatment of community-acquired pneumonia (CAP) caused by Streptococcus pneumoniae, including cases with concurrent bacteremia, or Staphylococcus aureus (methicillin-susceptible isolates only). Note: Not a preferred agent for CAP; may be used as an alternative in multidrug-resistant S. pneumoniae and methicillin-resistant S. aureus (MRSA) pneumonia. For methicillin-susceptible S. aureus, the use of beta-lactams is preferred (IDSA/ATS [Mandell 2007]).
Hospital-acquired or healthcare-associated: Treatment of hospital-acquired or healthcare-associated pneumonia caused by S. aureus (methicillin-susceptible and methicillin-resistant isolates) or S. pneumoniae. Note: For methicillin-susceptible S. aureus, the use of beta-lactams is preferred (IDSA/ATS [Kalil 2016]).
Skin and skin structure infections:
Complicated: Treatment of complicated skin and skin structure infections, including diabetic foot infections, without concomitant osteomyelitis, caused by S. aureus (methicillin-susceptible and methicillin-resistant isolates), Streptococcus pyogenes, or Streptococcus agalactiae.
Uncomplicated: Treatment of uncomplicated skin and skin structure infections caused by S. aureus (methicillin-susceptible isolates) or S. pyogenes.
Note: Generally reserved as alternative for skin and skin structure infections due to MRSA (IDSA [Liu 2011]; IDSA [Stevens 2014]).
Limitations of use: Linezolid has not been studied in the treatment of decubitus ulcers. Linezolid is not indicated for treatment of gram-negative infections; if a concomitant gram-negative pathogen is documented or suspected, initiate specific therapy immediately.
Use: Off Label
Anthrax, systemic infectionyes
Based on the Centers for Disease Control and Prevention expert panel meetings on prevention and treatment of anthrax in adults, linezolid is an effective and recommended agent for treatment of systemic anthrax.
CNS infection, health care-associated (eg, cerebrospinal fluid shunt infection)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for health care-associated ventriculitis and meningitis, linezolid is an effective and recommended alternative systemic therapy for treatment of cerebrospinal fluid shunt infections caused by staphylococci, including methicillin-resistant Staphylococcus aureus (MRSA).
Cystic fibrosis, acute pulmonary exacerbation, moderate to severec
Clinical experience suggests the utility of linezolid for treatment of acute pulmonary exacerbation in patients with cystic fibrosis Chmiel 2014, Simon 2019.
Endocarditis, treatment, native or prosthetic valveyes
Based on the American Heart Association scientific statement on infective endocarditis in adults, linezolid is an effective and recommended agent in the treatment of patients with infective endocarditis (native or prosthetic valve) due to enterococci resistant to penicillin, aminoglycosides, and vancomycin.
Intracranial abscess (brain abscess, intracranial epidural abscess) and spinal epidural abscesscyes
Based on the IDSA guidelines for the treatment of MRSA infections in adults and children, linezolid is an effective and recommended alternative agent in the treatment of MRSA infections of the CNS, including brain abscess and spinal epidural abscess. Clinical experience also suggests the utility of linezolid as an alternative agent for the treatment of intracranial epidural abscess Sexton 2019a.
Meningitis, bacterialyes
Based on the IDSA guidelines for the management of bacterial meningitis and for health care-associated ventriculitis and meningitis, linezolid is an effective and recommended alternative therapy for treatment of bacterial meningitis caused by Cutibacterium acnes or staphylococci (including MRSA) and a recommended therapy for enterococci resistant to penicillin, ampicillin, and vancomycin.
Osteomyelitis and/or discitisyes
Based on the IDSA guidelines for the treatment of MRSA infections in adults and children, linezolid is an effective and recommended alternative agent in the treatment of MRSA bone and joint infections, including osteomyelitis. Based on the IDSA guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults, linezolid is an effective and recommended alternative treatment option for native vertebral osteomyelitis due to staphylococci (oxacillin-susceptible or oxacillin-resistant) or Enterococcus spp. (penicillin-resistant or penicillin-sensitive).
Prosthetic joint infectionyes
Based on the IDSA guidelines for the management of prosthetic joint infection, linezolid is an effective and recommended alternative agent for the treatment of prosthetic joint infection with staphylococci (oxacillin-sensitive and oxacillin-resistant) and Enterococcus spp. (penicillin-sensitive and penicillin-resistant).
Septic arthritisyes
Based on the IDSA guidelines for the treatment of MRSA infections in adults and children, linezolid is an effective and recommended alternative agent in the treatment of MRSA bone and joint infections, including septic arthritis.
Toxic shock syndromec
Clinical experience suggests the utility of linezolid as an alternative agent for the treatment of streptococcal and staphylococcal toxic shock syndrome Chu 2019, Rac 2017, Stevens 2006, Stevens 2019.
Tuberculosis, drug-resistantbyes
Data from a randomized clinical trial conducted in South Korea evaluating the addition of linezolid to the existing anti-tuberculosis regimen in patients with sputum culture-positive extensively drug-resistant tuberculosis support the use of linezolid in this condition Lee 2012.
Based on the World Health Organization consolidated guidelines on drug-resistant tuberculosis treatment, linezolid is an effective and recommended alternative agent for treatment of resistant tuberculosis.
Contraindications
Hypersensitivity to linezolid or any component of the formulation; concurrent use or within 2 weeks of MAO inhibitors
Canadian labeling: Additional contraindications (not in US labeling): Unless monitored for potential increases in blood pressure, linezolid should not be administered to patients with uncontrolled hypertension, pheochromocytoma, thyrotoxicosis and/or patients taking any of the following: sympathomimetic agents (eg, pseudoephedrine, phenylpropanolamine), vasopressive agents (eg, epinephrine, norepinephrine), dopaminergic agents (eg, dopamine, dobutamine). Unless carefully observed for signs and/or symptoms of serotonin syndrome, linezolid should not be administered to patients with carcinoid syndrome and/or patients taking any of the following: SSRIs, TCAs, serotonin 5-HT1 receptor agonists (triptans), meperidine or buspirone.
Dosage and Administration
Dosing: Adult
Note: Linezolid is not a preferred agent for the treatment of infections requiring prolonged therapy as the risk of serious hematologic and neurologic toxicity increases after >2 weeks and >4 weeks of therapy, respectively.
Anthrax, systemic infection (off-label use): Note: Consult public health officials for event-specific recommendations.
IV: 600 mg every 12 hours as part of an appropriate combination regimen. The duration for non-CNS infection is ≥2 weeks or until clinically stable, whichever is longer. The duration for meningitis is ≥2 to 3 weeks or until clinically stable, whichever is longer (CDC [Hendricks 2014]).
Note: Antitoxin should also be administered. Following the course of IV combination therapy for systemic anthrax infection (including meningitis), patients exposed to aerosolized spores require oral monotherapy with an appropriate agent to complete a total antimicrobial course of 60 days (CDC [Hendricks 2014]).
Bloodstream infection:
Empiric therapy or pathogen-directed therapy for vancomycin-resistant enterococci: Oral, IV: 600 mg every 12 hours; treat uncomplicated bacteremia for 7 to 14 days from day of first negative blood culture, with longer courses warranted for endocarditis or metastatic sites of infection (IDSA [Mermel 2009]; Zhao 2016).
Empiric therapy or pathogen-directed therapy for methicillin-resistant Staphylococcus aureus (alternative agent) (off-label use): Oral, IV: 600 mg every 12 hours (Lowy 2019; Moise 2002); treat uncomplicated S. aureus bacteremia for ≥14 days from day of first negative blood culture, with longer courses warranted for endocarditis or metastatic sites of infection (IDSA [Mermel 2009]).
CNS infection, health care-associated (eg, cerebrospinal fluid shunt infection) (alternative agent) (off-label use): Pathogen-directed therapy for Staphylococcus spp., including methicillin-resistant species or Cutibacterium acnes.
Oral, IV: 600 mg every 12 hours; duration of therapy is generally 10 to 14 days (Boak 2006; Castro 2005; IDSA [Tunkel 2017]; Kanafani 2019; Nagashima 2008). For staphylococci, usually used in combination with rifampin (eg, in the setting of retained hardware) (IDSA [Tunkel 2017]), but conflicting data are available on the effect of rifampin on linezolid levels (Blassman 2016; Gómez 2011; Hoyo 2012).
Cystic fibrosis, acute pulmonary exacerbation, moderate to severe (off-label use): Empiric therapy or pathogen-directed therapy for methicillin-resistant S. aureus (MRSA) (Chmiel 2014; Simon 2019).
Oral, IV: 600 mg every 12 hours (Chmiel 2014; Keel 2011). Duration is usually 10 days to 3 weeks or longer based on clinical response (Flume 2009; Simon 2019).
Diabetic foot infection, moderate to severe: Empiric therapy or pathogen-directed therapy for MRSA.
Oral, IV: 600 mg every 12 hours; for empiric therapy, use as part of an appropriate combination regimen. Duration is usually 2 to 4 weeks in the absence of osteomyelitis; prolonged use of linezolid may be limited by toxicity (IDSA [Lipsky 2012]; Lipsky 2004; Weintrob 2019).
Endocarditis, treatment, native or prosthetic valve (off-label use): Pathogen-directed therapy for penicillin-, aminoglycoside-, and vancomycin-resistant enterococci.
IV, Oral: 600 mg every 12 hours for >6 weeks; prolonged use of linezolid may be limited by toxicity (AHA [Baddour 2015]).
Intracranial abscess (brain abscess, intracranial epidural abscess) and spinal epidural abscess (alternative agent) (off-label use): Pathogen-directed therapy for MRSA.
IV, Oral: 600 mg every 12 hours; duration generally ranges from 4 to 8 weeks for brain abscess and spinal epidural abscess, and 6 to 8 weeks for intracranial epidural abscess; prolonged use of linezolid may be limited by toxicity (Bodilsen 2018; IDSA [Liu 2011]; Ntziora 2007; Sexton 2019a; Sexton 2019b; Southwick 2019).
Meningitis, bacterial (off-label use): As pathogen-directed therapy (eg, penicillin-, ampicillin-, and vancomycin-resistant enterococci; Staphylococcus spp., including MRSA [alternative agent]; C. acnes [alternative agent]).
IV: 600 mg every 12 hours. Treatment duration is usually 10 to 14 days (IDSA [Tunkel 2004]; IDSA [Tunkel 2017]; Ntziora 2007; Sipahi 2013).
Osteomyelitis and/or discitis (alternative agent) (off-label use):
Pathogen-directed therapy for Staphylococcus spp., including methicillin-resistant S. aureus: Oral, IV: 600 mg every 12 hours (Birmingham 2003; IDSA [Berbari 2015]; IDSA [Liu 2011]; Rao 2004). Some experts combine with rifampin in the presence of retained hardware (IDSA [Liu 2011]), but conflicting data are available on the effect of rifampin on linezolid levels (Blassman 2016; Gómez 2011; Hoyo 2012).
Pathogen-directed therapy for Enterococcus spp.: Oral, IV: 600 mg every 12 hours (Birmingham 2003; IDSA [Berbari 2015]; IDSA [Liu 2011]; Rao 2004).
Duration of therapy: Duration is generally ≥6 weeks; prolonged use of linezolid may be limited by toxicity. Shorter courses are appropriate if the affected bone is completely resected (eg, by amputation) (IDSA [Berbari 2015]; Osmon 2019).
Pneumonia:
Community-acquired pneumonia: As a component of empiric therapy or pathogen-directed therapy for MRSA.
Oral, IV: 600 mg every 12 hours; duration is for ≥7 days; patients should be afebrile for ≥48 hours and clinically stable prior to discontinuation. When used for empiric therapy, give as part of an appropriate combination regimen (IDSA/ATS [Mandell 2007]; IDSA [Liu 2011]).
Hospital-acquired or ventilator-associated pneumonia: As a component of empiric therapy or pathogen-directed therapy for MRSA.
IV, Oral: 600 mg every 12 hours; duration is for ≥7 days and varies based on disease severity and response to therapy. When used for empiric therapy, give as part of an appropriate combination regimen (IDSA/ATS [Kalil 2016]; IDSA [Liu 2011]).
Prosthetic joint infection (alternative agent) (off-label use):
Pathogen-directed therapy for Enterococcus spp. (penicillin-susceptible or penicillin-resistant): Oral, IV: 600 mg every 12 hours for 4 to 6 weeks; prolonged use of linezolid may be limited by toxicity (IDSA [Osmon 2013]; manufacturer's labeling).
Pathogen-directed therapy for Staphylococcus spp., including methicillin-resistant S. aureus: Oral, IV: 600 mg every 12 hours. Duration ranges from 2 to 6 weeks depending on prosthesis management, use of rifampin, and other patient-specific factors; prolonged use of linezolid may be limited by toxicity (IDSA [Osmon 2013]; manufacturer's labeling).
Note: In select cases (eg, debridement and retention of prosthesis or one-stage arthroplasty), give oral suppressive antibiotic therapy with an appropriate regimen following completion of initial treatment (Berbari 2019; IDSA [Osmon 2013]).
Septic arthritis (alternative agent) (off-label use): Pathogen-directed therapy for MRSA.
Oral, IV: 600 mg every 12 hours. Total treatment duration is 3 to 4 weeks (in the absence of osteomyelitis); prolonged use of linezolid may be limited by toxicity (Goldenberg 2019; IDSA [Liu 2011]). Some experts recommend 4 weeks of therapy for patients with concomitant bacteremia (Goldenberg 2019).
Skin and soft tissue infection (alternative agent): Empiric therapy or pathogen-directed therapy for resistant gram-positive organisms (eg, MRSA).
Oral, IV: 600 mg every 12 hours. Total duration of therapy is usually 5 to 14 days; for necrotizing infection, continue until further debridement is not necessary and the patient has improved clinically, including being afebrile for ≥48 hours (IDSA [Liu 2011]; IDSA [Stevens 2014]). Note: For empiric therapy, give as part of an appropriate combination regimen (IDSA [Stevens 2014]).
Toxic shock syndrome (alternative agent) (off-label use):
Toxin production suppression due to group A streptococci: Oral, IV: 600 mg every 12 hours as part of an appropriate combination regimen. Duration is until clinically and hemodynamically stable for ≥48 to 72 hours; then discontinue linezolid and give monotherapy with an appropriate antistreptococcal agent (Rac 2017; Stevens 2019).
Empiric therapy or pathogen-directed therapy for S. aureus, including methicillin-resistant S. aureus and toxin production suppression: Oral, IV: 600 mg every 12 hours. Duration for toxin production is until clinically and hemodynamically stable for ≥48 to 72 hours; then discontinue linezolid and give monotherapy with an appropriate antistaphylococcal agent. If linezolid is given alone to complete therapy, the duration is typically 10 to 14 days in the absence of bacteremia (Chu 2019; Stevens 2006).
Tuberculosis, drug-resistant (alternative agent) (off-label use): Oral, IV: 600 mg once daily as part of an appropriate combination regimen including pyridoxine (Ahmad 2018; Caminero 2017; Lee 2012; Migliori 2009; Schluger 2019; WHO 2019); dose reduction to 300 to 450 mg once daily or 600 mg 3 to 4 times weekly may be used for patients who develop toxicity (Caminero 2017; Drew 2019; Schluger 2019). Consider serum monitoring to ensure therapeutic concentration (Bolhuis 2016; Kamp 2017; Schluger 2019). Note: Some experts recommend an initial dose of 600 mg twice daily for 4 to 6 weeks before reducing the dose to 300 to 600 mg once daily (Agyeman 2016; Tang 2015).
Duration of therapy: Individualize based on rapidity of culture conversion, extent of disease, and patient-specific factors, including clinical response and toxicity; use of linezolid for >6 months is recommended for optimal effectiveness (Schluger 2019; WHO 2019). Monitor closely for hematologic and neurologic toxicity (Lee 2012; WHO 2019).
Urinary tract infection, complicated (pyelonephritis or cystitis with signs/symptoms of systemic infection) (alternative agent): As a component of empiric therapy or pathogen-directed therapy for resistant gram-positive pathogens (eg, for vancomycin-resistant enterococci).
Oral, IV: 600 mg every 12 hours (Hooton 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Linezolid is not a preferred agent in treatment of infections requiring prolonged therapy (ie, >2 weeks) due to the risk of serious hematologic and neurologic toxicity. Use of linezolid is generally reserved for treatment of infections due to drug-resistant organisms (eg, MRSA, VRE).
General dosing, susceptible infection (mild, moderate, or severe) (Red Book 2012): Oral, IV:
Infants and Children <12 years: 10 mg/kg/dose every 8 hours, maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Bacteremia: Oral, IV: Note: Treatment should continue for 10 to 28 days depending on the organism.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Bone and joint infection (Liu 2011):
Osteomyelitis [S. aureus (methicillin-resistant)]: Oral, IV: Note: Treatment should continue for a minimum of 4 to 6 weeks.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Septic arthritis [S. aureus (methicillin-resistant)]: Oral, IV: Note:Treatment should continue for a minimum of 3 to 4 weeks.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Catheter (peritoneal dialysis); exit-site or tunnel infection (Warady [ISPD 2012]): Oral:
Infants and Children <5 years: 10 mg/kg/dose three times daily; maximum dose: 600 mg/dose
Children ≥5 years to 11 years: 10 mg/kg/dose twice daily; maximum dose: 600 mg/dose
Children ≥12 years and Adolescents: 600 mg/dose twice daily
Catheter-related infections, Staphylococcal (methicillin-resistant) or enterococcal (resistant) (confirmed infection): Oral, IV: Note: Not recommended use for empiric treatment (Mermel 2009).
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 10 mg/kg/dose every 12 hours; maximum dose: 600 mg
CNS infection:
Brain abscess, subdural empyema, spinal epidural abscess [S. aureus (methicillin-resistant)]: Oral, IV: Note: Treatment should continue for 4 to 6 weeks (Liu 2011). Note: The manufacturer does not recommend the use of linezolid for empiric treatment of pediatric CNS infections since therapeutic linezolid concentrations are not consistently achieved or maintained in the CSF of patients with ventriculoperitoneal shunts.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Meningitis [S. aureus (methicillin-resistant)]: Oral, IV: Note: Treatment should continue for 2 weeks (Liu 2011; Tunkel 2004).
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Endocarditis, treatment [E. faecium (vancomycin-resistant)]: Oral, IV: Note: Treatment should continue for at least 8 weeks (Baddour 2005).
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Peritonitis (peritoneal dialysis) (Warady [ISPD 2012]): Oral:
Infants and Children <5 years: 10 mg/kg/dose three times daily; maximum dose: 600 mg/dose
Children 5 to 11 years: 10 mg/kg/dose twice daily; maximum dose: 600 mg/dose
Children ≥12 years and Adolescents: 600 mg/dose twice daily
Pneumonia
Community- or hospital-acquired (non-MRSA): Oral, IV: Note: Treatment should continue for 10 to 14 days.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
S. aureus (methicillin-resistant): Oral, IV: Note: Treatment should continue for 7 to 21 days depending on severity (Liu 2011).
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Septic thrombosis of cavernous or dural venous sinus [S. aureus (methicillin-resistant)]: Oral, IV: Note: Treatment should continue for 4 to 6 weeks (Liu 2011).
Infants and Children <12 years: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: 600 mg every 12 hours
Skin and skin structure infections: Note: Treatment should continue for 10 to 14 days.
Uncomplicated:
Infants and Children <5 years: Oral: 10 mg/kg/dose every 8 hours
Children 5 to 11 years: Oral: 10 mg/kg/dose every 12 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: Oral: 600 mg every 12 hours
Complicated:
Infants and Children <12 years: Oral, IV: 10 mg/kg/dose every 8 hours; maximum dose: 600 mg
Children ≥12 years and Adolescents: Oral, IV: 600 mg every 12 hours
Tuberculosis, multidrug-resistant: Limited data available: Oral: Note: Experience in pediatric patients reflects extrapolation of dosing approach used in adult patients which includes a lower daily dose to decrease risk of adverse effects due to the anticipated long duration of therapy and if toxicity does occur, further dosage reductions (a 25% to 50% dose decrease or increased dosing interval have been used); reported treatment duration dependent upon clinical course; reported range: 13 to 36 months in pediatric patients. All reports describe linezolid as part of a multidrug antimycobacterial regimen; other reported agents within the combination therapy were variable, dependent upon specific organism sensitivities, and generally included 3 to 5 other agents.
Infants ≥4 months and Children: 10 to 12 mg/kg/dose twice daily; maximum dose: 600 mg; dosing based on case reports describing successful treatment in infants and a young child (n=3; ages: 4.5 months, 11 months, and 23 months) (Pinon 2010; Schaaf 2009). Use has also been reported in a 10-year old child, treatment was successfully completed with dosing of 600 mg once daily (Condos 2008).
Adolescents: 600 mg once daily was reported in a retrospective review of 30 patients (n= four adolescents) and a case report (patient age: 14 years) (Dauby 2011; Schecter 2010). In another case series, 600 mg twice daily dosing was used for the initial 2 weeks of therapy and then decreased to once daily dosing; at reduced dosage, patients seemed to have decreased hematologic toxicity while neurotoxicity remained unchanged (Park 2006).
Vancomycin-resistant Enterococcus faecium (VREF) infections: Oral, IV: Note: Treatment should continue for 14 to 28 days.
Infants and Children <12 years: 10 mg/kg/dose every 8 hours, maximum dose: 600 mg
Children ≥12 years and Adolescents: Oral, IV: 600 mg every 12 hours
Dosing: Obesity
Note: There are limited data on the effect of obesity on dosing requirements. In one study of obese patients, linezolid trough concentrations at steady state were not influenced by weight or BMI, but more so by estimated GFR using the CKD-EPI equation (Cojutti 2018).
Oral, IV: 600 mg every 12 hours for patients weighing ≤150 kg (Bhalodi 2013); alternatively, initial loading dose 600 mg once (expert opinion), then 450 mg every 8 hours in patients (BMI ≥25 kg/m2) with GFRCKD-EPI 60 to 129 mL/minute/1.73 m2 and organism minimal inhibitory concentration (MIC) of ≤1 mg/mL, based on Monte Carlo simulations. With MICs ≥2 mg/mL, this regimen may be suboptimal, but evidence-based dosing strategies are currently not available. Some authors advocate for doses up to 600 mg every 8 hours while performing therapeutic drug monitoring to ensure trough concentrations <8 mg/L. In the absence of therapeutic drug monitoring, doses of 600 mg every 8 hours and above should be avoided due to unacceptable risks for myelosuppression (Cojutti 2018).
Reconstitution
Oral suspension: Refer to manufacturer’s product labeling for reconstitution instructions. Prior to administration mix gently by inverting bottle; do not shake.
Administration
IV: Administer intravenous infusion over 30 to 120 minutes. Do not mix or infuse with other medications. When the same intravenous line is used for sequential infusion of other medications, flush line with D5W, NS, or LR before and after infusing linezolid. The yellow color of the injection may intensify over time without affecting potency.
Oral: Administer without regard to meals.
Oral suspension: Invert gently to mix prior to administration, do not shake.
Dietary Considerations
Some products may contain sodium and/or phenylalanine. Avoid consuming large amounts of tyramine-containing foods/beverages. Some examples include aged or matured cheese, air-dried or cured meats (including sausages and salami), fava or broad bean pods, tap/draft beers, Marmite concentrate, sauerkraut, soy sauce, and other soybean condiments.
Storage
Infusion: Store at 25°C (77°F). Protect from light and freezing. Keep infusion bags in overwrap until ready for use.
Oral suspension: Store at 25°C (77°F); following reconstitution store at room temperature and use suspension within 21 days. Protect from light.
Tablet: Store at 25°C (77°F). Protect from light and moisture.
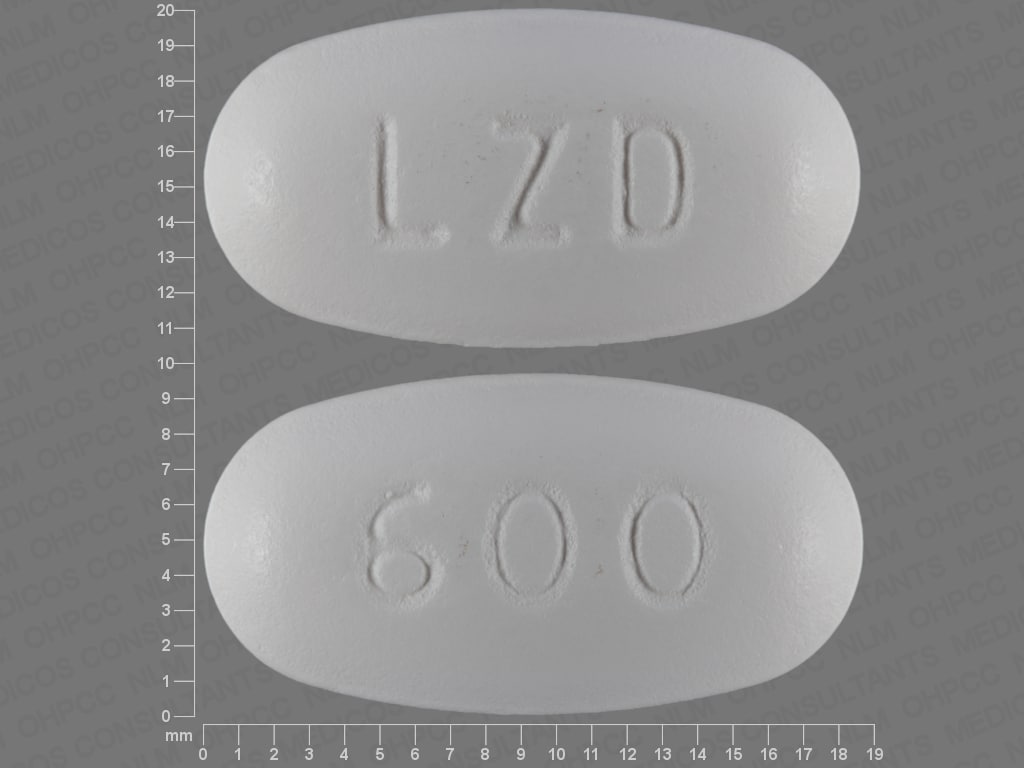
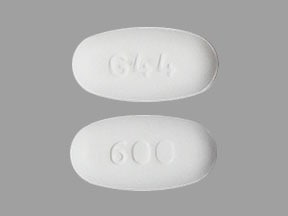
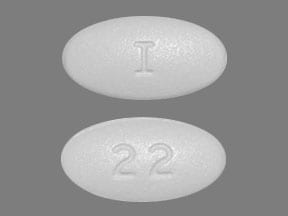
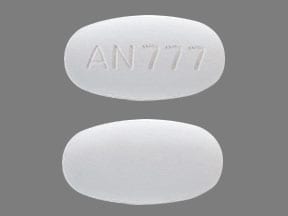
Linezolid Images
Drug Interactions
Alcohol (Ethyl): May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amphetamines: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Amphetamines. While linezolid and tedizolid may interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to monographs specific to those agents for details. Avoid combination
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Apraclonidine: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Apraclonidine. Monoamine Oxidase Inhibitors may increase the serum concentration of Apraclonidine. Avoid combination
AtoMOXetine: Monoamine Oxidase Inhibitors may enhance the neurotoxic (central) effect of AtoMOXetine. Avoid combination
Atropine (Ophthalmic): Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Atropine (Ophthalmic). Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Benzhydrocodone: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Management: The use of benzhydrocodone is not recommended for patients taking monoamine oxidase inhibitors (MAOIs) or within 14 days of MAOI discontinuation. Consider therapy modification
Betahistine: Monoamine Oxidase Inhibitors may increase the serum concentration of Betahistine. Monitor therapy
Bezafibrate: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Bezafibrate. Avoid combination
Blood Glucose Lowering Agents: Monoamine Oxidase Inhibitors may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Brimonidine (Ophthalmic): Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Brimonidine (Ophthalmic). Monoamine Oxidase Inhibitors may increase the serum concentration of Brimonidine (Ophthalmic). Monitor therapy
Brimonidine (Topical): Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Brimonidine (Topical). Monoamine Oxidase Inhibitors may increase the serum concentration of Brimonidine (Topical). Monitor therapy
Buprenorphine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
BuPROPion: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of BuPROPion. Avoid combination
BusPIRone: May enhance the serotonergic effect of Linezolid. This could result in serotonin syndrome. Avoid combination
CarBAMazepine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Management: Avoid concurrent use of carbamazepine during, or within 14 days of discontinuing, treatment with a monoamine oxidase inhibitor. Avoid combination
Cerebrolysin: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
Codeine: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Codeine. Avoid combination
COMT Inhibitors: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Consider therapy modification
Cyclobenzaprine: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Avoid combination
Cyproheptadine: Monoamine Oxidase Inhibitors may enhance the anticholinergic effect of Cyproheptadine. Cyproheptadine may diminish the serotonergic effect of Monoamine Oxidase Inhibitors. Avoid combination
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Deutetrabenazine: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Deutetrabenazine. Avoid combination
Dexmethylphenidate: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Dexmethylphenidate. Avoid combination
Dextromethorphan: Monoamine Oxidase Inhibitors may enhance the serotonergic effect of Dextromethorphan. This may cause serotonin syndrome. Avoid combination
Diethylpropion: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Diethylpropion. Avoid combination
Dihydrocodeine: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Monitor therapy
Diphenoxylate: May enhance the hypertensive effect of Monoamine Oxidase Inhibitors. Avoid combination
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Domperidone: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Domperidone. Monoamine Oxidase Inhibitors may diminish the therapeutic effect of Domperidone. Domperidone may diminish the therapeutic effect of Monoamine Oxidase Inhibitors. Monitor therapy
DOPamine: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of DOPamine. Management: Initiate dopamine at no greater than one-tenth (1/10) of the usual dose in patients who are taking (or have taken within the last 2 to 3 weeks) monoamine oxidase inhibitors. Monitor for an exaggerated hypertensive response to dopamine. Consider therapy modification
Droxidopa: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Droxidopa. Avoid combination
EPINEPHrine (Oral Inhalation): Monoamine Oxidase Inhibitors may enhance the hypertensive effect of EPINEPHrine (Oral Inhalation). Avoid combination
Epinephrine (Racemic): Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Epinephrine (Racemic). Monitor therapy
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Esketamine: May enhance the hypertensive effect of Monoamine Oxidase Inhibitors. Monitor therapy
Guanethidine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Heroin: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Heroin. Avoid combination
HYDROcodone: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of HYDROcodone. Management: Consider alternatives to this combination when possible. Consider therapy modification
HYDROmorphone: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of HYDROmorphone. Avoid combination
Indoramin: Monoamine Oxidase Inhibitors may enhance the hypotensive effect of Indoramin. Avoid combination
Iobenguane Radiopharmaceutical Products: Monoamine Oxidase Inhibitors may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Isometheptene: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Isometheptene. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Levodopa-Containing Products: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Of particular concern is the development of hypertensive reactions when levodopa is used with nonselective MAOI. Avoid combination
Levomethadone: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Levonordefrin: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Levonordefrin. Avoid combination
Lithium: Linezolid may enhance the serotonergic effect of Lithium. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Maprotiline: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Meptazinol: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Meptazinol. Avoid combination
Mequitazine: Monoamine Oxidase Inhibitors may enhance the anticholinergic effect of Mequitazine. Avoid combination
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methadone: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Avoid combination
Methyldopa: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Methyldopa. Avoid combination
Methylene Blue: May enhance the serotonergic effect of Linezolid. This could result in serotonin syndrome. Avoid combination
Methylphenidate: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Methylphenidate. Avoid combination
Metoclopramide: May enhance the hypertensive effect of Monoamine Oxidase Inhibitors. Avoid combination
Mianserin: Monoamine Oxidase Inhibitors may enhance the neurotoxic effect of Mianserin. Avoid combination
Monoamine Oxidase Inhibitors (Antidepressant): Linezolid may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Antidepressant). This could result in serotonin syndrome. Avoid combination
Monoamine Oxidase Inhibitors (Type B): Linezolid may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Type B). This could result in serotonin syndrome. Avoid combination
Morphine (Systemic): Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Morphine (Systemic). Avoid combination
Nefazodone: Linezolid may enhance the serotonergic effect of Nefazodone. This could result in serotonin syndrome. Avoid combination
Nefopam: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Nefopam. Avoid combination
Normethadone: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Normethadone. Avoid combination
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FentaNYL; Meperidine; TraMADol. Monitor therapy
Opium: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Opium. Avoid combination
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
OxyCODONE: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Avoid combination
OxyMORphone: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Pheniramine: May enhance the anticholinergic effect of Monoamine Oxidase Inhibitors. Avoid combination
Pholcodine: May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Avoid combination
Pizotifen: Monoamine Oxidase Inhibitors may enhance the anticholinergic effect of Pizotifen. Avoid combination
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Reboxetine: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Reboxetine. Avoid combination
Remifentanil: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Remifentanil. Specifically, the risk for opioid toxicity (eg, respiratory depression) may be increased. Remifentanil may enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Management: The use of remifentanil is not recommended for patients taking monoamine oxidase inhibitors (MAOIs) or within 14 days of MAOI discontinuation. Consider therapy modification
Reserpine: Monoamine Oxidase Inhibitors may enhance the adverse/toxic effect of Reserpine. Existing MAOI therapy can result in paradoxical effects of added reserpine (e.g., excitation, hypertension). Management: Monoamine oxidase inhibitors (MAOIs) should be avoided or used with great caution in patients who are also receiving reserpine. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: Linezolid may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Exceptions: Dapoxetine. Avoid combination
Serotonergic Non-Opioid CNS Depressants: Linezolid may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Avoid combination
Serotonergic Opioids (High Risk): Linezolid may enhance the serotonergic effect of Serotonergic Opioids (High Risk). This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Monoamine Oxidase Inhibitors may increase the serum concentration of Serotonin 5-HT1D Receptor Agonists (Triptans). Avoid combination
Serotonin/Norepinephrine Reuptake Inhibitors: Linezolid may enhance the serotonergic effect of Serotonin/Norepinephrine Reuptake Inhibitors. This could result in serotonin syndrome. Avoid combination
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Solriamfetol: Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Solriamfetol. Avoid combination
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
SUFentanil: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Specifically, the risk for serotonin syndrome or opioid toxicities (eg, respiratory depression, coma) may be increased. Management: Sufentanil should not be used with monoamine oxidase (MAO) inhibitors (or within 14 days of stopping an MAO inhibitor) due to the potential for serotonin syndrome and/or excessive CNS depression. Avoid combination
Sympathomimetics: Linezolid may enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tapentadol: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Specifically, the additive effects of norepinephrine may lead to adverse cardiovascular effects. Tapentadol may enhance the serotonergic effect of Monoamine Oxidase Inhibitors. This could result in serotonin syndrome. Avoid combination
Tetrabenazine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Tetrahydrozoline (Nasal): Monoamine Oxidase Inhibitors may enhance the hypertensive effect of Tetrahydrozoline (Nasal). Avoid combination
Tianeptine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Tricyclic Antidepressants: Linezolid may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Avoid combination
Tryptophan: Linezolid may enhance the serotonergic effect of Tryptophan. This could result in serotonin syndrome. Avoid combination
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Valbenazine: May enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Adverse Reactions
>10%:
Gastrointestinal: Diarrhea (8% to 11%)
Hematologic & oncologic: Decreased white blood cells (neonates, infants, and children: 12%; children, adolescents, and adults: ≤2%), decreased platelet count (adults: ≤10%)
1% to 10%:
Central nervous system: Headache (children, adolescents, and adults: 6% to 9%; neonates, infants, and children: <1%), dizziness (adults: 2% to 3%), vertigo (children and adolescents: 1%)
Dermatologic: Skin rash (adults: 1% to 2%), pruritus (neonates, infants, children, and adolescents: ≤1%; nonapplication site)
Endocrine & metabolic: Increased amylase (≤2%), increased lactate dehydrogenase (adults: ≤2%)
Gastrointestinal: Vomiting (3% to 9%), nausea (2% to 7%), increased serum lipase (adults: 3% to 4%; children and adolescents: <1%), loose stools (neonates, infants, children, and adolescents: 2%), abdominal pain (≤2%), oral candidiasis (adults: ≤2%), dysgeusia (adults: 1% to 2%), tongue discoloration (≤1%)
Genitourinary: Vulvovaginal candidiasis (adults: 1% to 2%)
Hematologic & oncologic: Anemia (neonates, infants, and children: 6%; adults ≤2%), decreased neutrophils (neonates, infants, and children: 6%; children, adolescents, and adults: ≤1%), thrombocytopenia (neonates, infants, and children: 5%), eosinophilia (neonates, infants, children, and adolescents: ≤2%)
Hepatic: Increased serum ALT (2% to 10%), increased serum bilirubin (neonates, infants, and children: 6%; adults: <1%), increased serum AST (adults: 2% to 5%), increased serum alkaline phosphatase (adults: ≤4%), abnormal hepatic function tests (adults: ≤2%)
Infection: Fungal infection (adults: ≤2%)
Renal: Increased blood urea nitrogen (adults: ≤2%), increased serum creatinine (≤2%)
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, blurred vision, bone marrow depression, bullous skin disease, Clostridioides (formerly Clostridium) difficile-associated diarrhea, dental discoloration, hypoglycemia, lactic acidosis, optic neuropathy, pancytopenia, peripheral neuropathy, seizure, serotonin syndrome (with concurrent use of other serotonergic agents), severe dermatological reaction, sideroblastic anemia, Stevens-Johnson syndrome, toxic epidermal necrolysis, vision loss
Warnings/Precautions
Concerns related to adverse effects:
- Lactic acidosis: Has been reported with use. Patients who develop recurrent nausea and vomiting, unexplained acidosis, or low bicarbonate levels need immediate evaluation.
- Myelosuppression: Has been reported and may be dependent on duration of therapy (generally >2 weeks of treatment); use with caution in patients with preexisting myelosuppression, in patients receiving other drugs which may cause bone marrow suppression, or in chronic infection (previous or concurrent antibiotic therapy). Weekly CBC monitoring is recommended; consider discontinuation in patients developing myelosuppression (or in whom myelosuppression worsens during treatment). Thrombocytopenia is the most frequently observed blood dyscrasia.
- Peripheral and optic neuropathy (with vision loss): Has been reported in adults and children and may occur primarily with extended courses of therapy >28 days; any symptoms of visual change or impairment warrant immediate ophthalmic evaluation and possible discontinuation of therapy.
- Serotonin syndrome: Symptoms of agitation, confusion, hallucinations, hyper-reflexia, myoclonus, shivering, and tachycardia may occur with concomitant proserotonergic drugs, agents which reduce linezolid's metabolism, or in patients with carcinoid syndrome. Avoid use in such patients unless clinically appropriate and under close monitoring for signs/symptoms of serotonin syndrome or neuroleptic malignant syndrome-like reactions.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Carcinoid syndrome: Use with caution and closely monitor for serotonin syndrome in patients with carcinoid syndrome; linezolid has not been studied in patients with this condition. Do not use in the absence of close monitoring.
- Diabetes mellitus: Hypoglycemic episodes have been reported; use with caution and closely monitor glucose in diabetic patients. Dose reductions/discontinuation of concurrent hypoglycemic agents or discontinuation of linezolid may be required.
- Hypertension: Use with caution and closely monitor blood pressure in patients with uncontrolled hypertension; linezolid has not been studied in patients with this condition. Do not use in the absence of close monitoring.
- Hyperthyroidism: Use with caution and closely monitor blood pressure in patients with untreated hyperthyroidism; linezolid has not been studied in patients with this condition. Do not use in the absence of close monitoring.
- Pheochromocytoma: Use with caution and closely monitor blood pressure in patients with pheochromocytoma; linezolid has not been studied in patients with this condition. Do not use in the absence of close monitoring.
- Seizure disorder: Seizures have been reported; use with caution in patients with a history of seizures.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: The manufacturer does not recommend the use of linezolid for empiric treatment of pediatric CNS infections since therapeutic linezolid concentrations are not consistently achieved or maintained in the CSF of patients with ventriculoperitoneal shunts. However, limited data in the form of case reports in pediatric and adult patients suggest that linezolid may be useful in treating gram-positive CNS infections that have failed to respond to other treatment options describing successful treatment of documented VRE and Staphylococcus aureus CNS and shunt infections in the literature (Cook 2005; da Silva 2007; Milstone 2007; Shaikh 2001; Villani 2002).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Phenylalanine: Some products may contain phenylalanine.
Other warnings/precautions:
- Appropriate use: Unnecessary use may lead to the development of resistance to linezolid; consider alternatives before initiating outpatient treatment.
- Catheter-related bloodstream infections (CRBSI): Linezolid should not be used in the empiric treatment of CRBSI, but may be appropriate for targeted therapy (Mermel 2009).
Monitoring Parameters
Weekly CBC, particularly in patients at increased risk of bleeding, with pre-existing myelosuppression, on concomitant medications that cause bone marrow suppression, in those who require >2 weeks of therapy, or in those with chronic infection who have received previous or concomitant antibiotic therapy; peripheral sensory and visual function with extended therapy (≥3 months) or in patients with new onset neuropathic or visual symptoms, regardless of therapy length; in patients with renal impairment, monitor for hematopoietic (eg, anemia, leukopenia, thrombocytopenia) and neuropathic (eg, peripheral neuropathy) adverse events when administering for extended periods. Periodic serum bicarbonate with extended therapy. Consider monitoring lactic acid in patients with renal dysfunction (Mori 2018).
Linezolid has been found to have significant interpatient variability (Cattaneo 2016; Pea 2010; Pea 2017) and limited data suggest that monitoring linezolid trough concentrations may be used to optimize dosing, especially in patients with renal dysfunction (Cattaneo 2016; Gervasoni 2015; Pea 2017) and/or concern for thrombocytopenia (Matsumoto 2010; Nukui 2013; Tsuji 2017).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Information related to linezolid use during pregnancy is limited (Jaspard 2017; Mercieri 2010). Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of linezolid may be altered (van Kampenhout 2017).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Lactic acidosis like fast breathing, fast heartbeat, abnormal heartbeat, vomiting, drowsiness, shortness of breath, loss of strength and energy, severe dizziness, feeling cold, or muscle pain or cramps.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Vision changes
- Severe headache
- Dizziness
- Passing out
- Seizures
- Burning or numbness feeling
- Bruising
- Bleeding
- Severe loss of strength and energy
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.